About Us
Founded in 1950 by Variety Clubs International, Nicklaus Children’s Hospital is South Florida’s only licensed specialty hospital exclusively for children, with approximately 800 attending physicians, including more than 500 pediatric subspecialists. The 307-bed hospital, known as Miami Children’s Hospital from 1983 through 2014, is renowned for excellence in all aspects of pediatric medicine with many specialty programs routinely ranked among the best in the nation by U.S. News & World Report since 2008. The hospital is also home to the largest pediatric teaching program in the southeastern United States and since 2003 has been designated an American Nurses Credentialing Center (ANCC) Magnet facility, the nursing profession’s most prestigious institutional honor.
The Nicklaus Children's Hospital network includes more than a dozen outpatient centers extending from Martin County to southern Miami-Dade County, offering a range of pediatric healthcare services, including urgent care, rehabilitation services and subspecialty physician appointments for children of all ages, including up to age 21.
We are committed to being a resource for children from throughout South Florida and around the world.
About Nicklaus Children's Health System
Nicklaus Children’s Health System is the parent organization of Nicklaus Children’s Hospital, South Florida’s only licensed specialty hospital exclusively for children. The 307-bed nonprofit hospital, known as Miami Children’s Hospital from 1983 through 2014, was founded in 1950 by Variety Clubs International and is renowned for excellence in all aspects of pediatric medicine, with many programs routinely ranked among the nation’s best by U.S. News & World Report. The health system also includes Nicklaus Children’s Hospital Foundation, the organization's 501c3 fundraising arm; a network of nonprofit outpatient and urgent care centers situated in Miami-Dade, Broward, Palm Beach and Martin counties; a nonprofit physician practice subsidiary; and an ambulatory surgery center. Nicklaus Children's Health System is the region’s only healthcare system exclusively for children.
Our vision is to create a healthy future for every child. Ultimately, this means being there through all stages of health and life, both physically and emotionally. To be a trusted partner to children and their families, not only in times of illness but throughout their life journey.
Our Mission
To inspire hope and promote lifelong health by providing the best care to every child.
Our Vision
To CREATE a healthy future for every child.
Values and Guiding Behaviors
- C ollaboration
- R esponsibility
- E mpowerment
- A dvocacy
- Transformation
- E mpathy
Forward for the Children, 2023-2025 Strategic Plan
Nicklaus Children’s Health System is pleased to share our 2023-2025 Strategic Plan. As stewards of the region’s only freestanding children’s hospital – one that has served this community with distinction for more than 70 years – we recognize the critical importance of strategic planning and alignment. Our three-year plan guides our collaboration internally and within the broader community to advance our mission of providing the best care to every child.
Download PDF
Medical Services
Pediatric Medical Services
News & Events
Receive regular updates with our news, community events and other updates
How Can I Help?
Become a Volunteer
Volunteers are an important part of the patient-care process at Nicklaus Children's Hospital. Each makes a significant contribution to our mission of providing the highest quality healthcare to our patients.
Learn more about volunteering
Sponsor a Special Event
Special Events refer to visits that allow our patients the opportunity for hands-on participation and involvement via unique experiences and activities. Since many of our programs already provide ample craft and play opportunities daily, we value your creativity in proposing a visit which will provide our patients with a “one-of-a-kind” activity.
Apply to sponsor a special event
Make a Donation
 Each year, our hospital provides thousands of children with the pediatric care they need. You can help us be there for the children by making an investment in their future through a contribution to Nicklaus Children's Hospital Foundation.
Each year, our hospital provides thousands of children with the pediatric care they need. You can help us be there for the children by making an investment in their future through a contribution to Nicklaus Children's Hospital Foundation.
Make a contribution
Join our Advocacy Team
Nicklaus Children's Hospital Department of Public Policy and Government Relations needs the support and involvement of parents, families, physicians and other interested individuals, as well as healthcare and community organizations, to ensure a better quality of life for all children. You can take an active role in ensuring that our young people enjoy a healthier and safer future by joining the Children’s Advocacy Network.
Advocate for children's health
ENRICH Literacy Program
The ENRICH Literacy Program was created in collaboration with clinicians to educate and empower all parents to engage, nurture, and read to infants and children. The program provides resources for parents and educators in our community to increase literacy rates from birth and beyond.
Learn moreMedical Professionals
Nicklaus Children's Hospital offers a wide array of resources for pediatric physicians, other pediatric healthcare providers and medical researchers. Whether you are a new pediatric physician looking for residency opportunities, a pediatric nurse looking into the Nicklaus Children's Hospital Nursing program or a member of our medical staff wanting to refer a patient or conducting research, this section will help you find the answers to your questions.
Pediatric Medical Education
The Nicklaus Children's Hospital Medical Education Department is committed to the oversight and provision of high-quality, evidence-based, and innovative education.
For Pediatric Nurses
Nicklaus Children's Hospital is proud to have received multiple Magnet designations - a testament to our nurses and our commitment to pediatric health. Learn more about our nationally recognized nursing leadership.
For Students and Interns
Nicklaus Children's Hospital is committed to its role as a teaching hospital providing medical school rotations throughout most of the departments.
Latest News
Careers & Employment
If you feel your purpose is to positively impact a child’s world, apply today. Our employees have access to a generous benefits package that goes way beyond standard offerings. View job listings, career and employment opportunities available.
Florida Health Finder
In order to help families make an informed decision when considering where to seek healthcare for their child, Nicklaus Children's Hospital is making available a link to the consumer health website www.FloridaHealthFinder.gov
The State of Florida's FloridaHealthFinder website includes information regarding all ages of patients in all Florida hospitals and healthcare facilities. It is important to note that Nicklaus Children's Hospital is a specialty hospital licensed to serve children from premature newborns to 21 years of age.
The FloridaHealthFinder website displays information regarding:
- Number of patients admitted to the hospital or seen for specific procedures
- Average length of stay (days) in the hospital
- Average hospital charges
- Average readmission rates to the hospital
- Mortality rates
- Complication rates for various medical conditions and procedures
- Quality care indicators such as these are monitored very closely at our hospital, and our staff strives to perform at levels that are often times the standard for other hospitals nationwide.
Hospital Services
While reviewing the data pertaining to Nicklaus Children's Hospital you may find the following information helpful in clarifying our unique services:
Neonatal Intensive Care Unit (NICU)
Nicklaus Children's Hospital has a Level 3 NICU. Level 3 represents the highest level of services that any hospital can provide a newborn. Because we do not have a maternity department nor do we birth infants at Nicklaus Children's Hospital other hospitals throughout Florida, U.S. Territories, and Atlantic/Caribbean countries regularly send their seriously ill newborns to our NICU for specialized, comprehensive medical and surgical care. Learn more.
Burn Centers
The State of Florida has designated 4 trauma centers throughout the state as 'burn centers'. These burn centers offer comprehensive, specialized care for the most serious burns (3rd degree burns or 2nd degree burns affecting a significant percent of the patient's body surface area) as outlined by the American Burn Association. Any pediatric patient who comes to Nicklaus Children's Hospital with a burn receives initial treatment at the Nicklaus Children's Hospital Emergency Department. All pediatric burn patients with a mild to moderate burn (1st degree burn to a 2nd degree burn affecting a less expansive of the body surface area) will remain at Nicklaus Children's Hospital for treatment. All severe burn patients are transferred to the designated burn unit in the region.
Trauma Center
Nicklaus Children's Hospital is a state approved pediatric trauma center. Nicklaus Children's is proud to be one of only two freestanding pediatric trauma centers in the State of Florida; and the only freestanding pediatric trauma center in South Florida. Learn more.
Pediatric Open Heart
Nicklaus Children's Hospital, a Children's Medical Services (CMS) Pediatric Cardiovascular Center, performs more cardiac procedures with better outcomes than any other facility in the region. Learn more.
Adult Open Heart
Since Nicklaus Children's Hospital is a pediatric facility that provides care for children 21 years of age and younger, The Heart Institute treats only a limited number of cases where the patient is between the ages of 18-21 years.
Organ Transplantation
Nicklaus Children's Hospital is a certified Bone Marrow Transplantation center. The Nicklaus Children's Hospital Bone Marrow Transplantation Program has been accredited by The Foundation for Accreditation of Hematopoietic Cell Therapy (FAHCT).
Nicklaus Children's Hospital works with patients and families to select the optimal transplant center for the specific organ and medical condition of the patient. Learn more.
Statutory Teaching Hospital
Nicklaus Children's Hospital is not listed as a statutory teaching hospital on the FloridaCompareCare website.
A statutory teaching hospital is defined as "any Florida hospital officially affiliated with an accredited Florida medical school". Nicklaus Children's Hospital is affiliated with the State University of New York (SUNY), an accredited medical school which is located in New York, not Florida. Nicklaus Children's is a world leader in pediatric medical education and is the largest freestanding pediatric teaching hospital in the Southeastern United States. Learn more.
Psychiatric Acute Care
Nicklaus Children's Hospital provides psychiatric acute care services for the pediatric population only. Learn more.
Rehabilitation Care
Nicklaus Children's Hospital works with patients and families to select the optimal rehabilitation program based on the child's specific needs. Learn more.
Rural Hospital
Nicklaus Children's Hospital is located in Miami, FL, a metropolitan area in the southeastern part of the state.
Critical Care Access Hospital
Nicklaus Children's Hospital does not meet the criteria of a Critical Care Access Hospital based on the fact that the hospital is not located in a rural area.
By definition, a Critical Care Access Hospital is a hospital located in a rural area that must maintain key services for patients needing critical care, as designated by the Social Security Act and certified by the Secretary of Health and Human Services.
Primary Stroke Center
Nicklaus Children's Hospital is not a Primary Stroke Center due to the fact that this category is applicable solely to adult acute care facilities.
Comprehensive Cancer Center
Nicklaus Children's Hospital is not a National Cancer Institute-designated Comprehensive Cancer Center.
The Nicklaus Children's Hospital Cancer Center has received national recognition and full member status in the Children Oncology Group (COG), a national cooperative oncology research group, and was awarded a grant by the National Cancer Institute for pediatric cancer research. Nicklaus Children's Hospital provides care for more pediatric cancer patients than any other hospital in South Florida. Learn more.
Risk Adjusted Average Charge Data
The risk adjusted average charge data contains charge information from hospitals and healthcare facilities throughout the State of Florida. While Nicklaus Children's Hospital average charge data is higher than the statewide average, please note that the cost of living in Miami-Dade County is 17.9% higher than the average cost of living statewide*.
Please note that the data compares risk adjusted average charges for hospitals caring for adults, children, and newborns; thus, as a specialty hospital caring solely for acutely ill children and newborns, this overall state average is not optimal for purposes of comparison.
It may be more appropriate for parents/guardians to contact Nicklaus Children's Hospital directly in order to obtain a more accurate estimation of charges and/or receive counseling on the availability of known financial resources for their own child's potential healthcare needs.
Risk Adjusted Readmission Data
It is important to note that the risk adjusted pediatric data comparisons (i.e. readmission rate) provided on the FloridaCompareCare website are based on entire state populations (all age groups), not just the pediatric population (ages 0-17 years).
Nicklaus Children's Hospital clinical programs are highly acclaimed by peer children's hospitals across the country. We're here for the children and to help you make the right choice for your child's healthcare needs.
*Average cost of living calculated by Sperling's Best Place (www.bestplaces.net). Visit FloridaHealthFinder.gov, for more information.
Highlights
Nicklaus Children's Hospital, part of Nicklaus Children's Health System, is Florida's pediatric care leader. The 307-bed pediatric specialty hospital and its network of pediatric outpatient centers offers comprehensive care for children of the region and beyond.
Our Campus
- The 40-bed Level III and Level II Neonatal Intensive Care Unit receives referrals of the most critically ill neonates from hospitals throughout South Florida, the Caribbean and Latin America.
- The 40-bed Pediatric Intensive Care Unit (PICU)Pediatric Intensive Care Unit receives referrals of complex cases from throughout the region and beyond.
- The 34-bed Cardiac Intensive Care Unit was the first in the Southeast, and provides care for newborns and children receiving treatment for congenital heart defects.
- Nicklaus Children’s Hospital is home to South Florida’s only freestanding pediatric trauma center and one of the most visited emergency rooms in the nation.
Our Community Outreach
Nicklaus Children’s Hospital contributes greatly to the well-being of Florida’s children and their families. Here’s how we make a difference in ways both BIG and small:
- The health system contributes millions of dollars in uncompensated care.
- The hospital is proud to be the largest provider of pediatric medical education in the southeastern United States.
- The hospital provides primary care and a medical home to the Medicaid population through its 10 Pediatric Care Centers.
- Dental services for underserved children and adolescents are offered at the Nicklaus Children’s Doral Outpatient Center. In addition, a Nicklaus mobile dental unit extends services to communities with little access to affordable dental care.
- Nicklaus Children’s Hospital’s School Health Program aims to improve access to quality healthcare through the delivery of health services and community resources to children in schools. The School Health Program is supported by two partnerships, one with The Children’s Trust serving 13 schools, and the other with the Department of Health and Miami-Dade County Public Schools, serving 62 schools. These programs bring RNs, APRNs, licensed social workers, care assistants and mental health therapists to more than 30,000 students in schools throughout Miami-Dade county.
- Nicklaus Children’s Hospital has served children from every single county in Florida, providing care that only a world-class children’s hospital makes possible.
- Nicklaus Children’s Virtual Care offers convenient access to pediatric care through the hospital’s Telehealth Center, bringing expert care and peace of mind to families in the comfort of their homes.
- Through the Nicklaus Children’s Research Institute, the hospital contributes significantly to pediatric medical research, with approximately 300 research protocols underway with potential to advance future clinical offerings for children around the globe.
- Nicklaus Children’s is the exclusive member hospital for Children’s Miracle Network in the region, serving eight counties in South Florida and the Treasure Coast. Visit give.nicklauschildrens.org
Awards, Highlights and Achievements
History
Our Mission, Vision and Values
Mission
To inspire hope and promote lifelong health by providing the best care to every child.
Vision
To create a healthy future for every child.
Values and Guiding Behaviors
- Collaboration
- Responsibility
- Empowerment
- Advocacy
- Transformation
- Empathy

Phone Directory
Search our phone number listings and department phone number directory.
To search for a physicians' office please search using the physician directory.
Web Site Information Disclaimer
Variety Children’s Hospital D/B/A Nicklaus Children's Hospital, formerly Miami Children's Hospital, Web Site Information, Disclaimers and Liability
By using this web site, you acknowledge that you have read and understand the following notices and disclaimers, and you agree to be bound by these terms. Any subsequent access to this web site by means that bypass this page shall also constitute a reaffirmation and agreement to the following terms and to any modifications or amendments thereto which Nicklaus Children's Hospital may establish from time to time. Nicklaus Children's Hospital reserves the right to change the terms and conditions pursuant to which the materials on this web site are made available. You agree to review these terms and conditions periodically to become aware of any such changes. Your continued use of the web site shall be deemed your acceptance of any changed terms and conditions.
1. PURPOSE: The purpose of this web site is to provide information on pediatric health and disease prevention. This information is not intended to be, nor should it be, used as a substitute for examination, diagnosis and medical treatment by a licensed and qualified health care professional. Always seek the advice of your physician or other qualified health provider prior to making any treatment decisions and with any questions you may have regarding a medical condition or its treatment. This web site is not intended to be advertising and shall not be deemed to constitute advertising in any state where this web site fails to comply with all laws and ethical rules of such state.
2. LIMITATION OF LIABILITY: Nicklaus Children's Hospital disclaims any and all warranties, express or implied, related to this web site and any information contained herein, including any warranties as to the accuracy, completeness, timeliness, correctness, noninfringement, merchantability or fitness for a particular purpose of the data, materials, interpretations, analyses, reports and any other information available through this web site, or the web site itself. To the extent permitted by law, Nicklaus Children's Hospital shall not be liable to you or anyone else for any loss or injury caused directly or indirectly, in whole or in part, by its construction and publication of this web site or for any decision made, or action taken, in reliance on the contents hereof.
3. CONTENTS: Nicklaus Children's Hospital attempts to insure the integrity and accuracy of this web site; however, Nicklaus Children's Hospital makes no guarantees whatsoever as to the correctness and accuracy of this site. The materials on this web site are offered as is. It is possible that the site may include inaccuracies or errors, and that unauthorized additions and alterations may be made to the site by third parties. In the event you detect such an inaccuracy, please inform Nicklaus Children's Hospital.
4. LINKS TO OTHER SITES: Nicklaus Children's Hospital makes no judgment or warranty with respect to the accuracy, timeliness or safety of the content of other Internet sites to which these pages may link. A link to a non-Nicklaus Children's Hospital web site is not an endorsement of that site, its content or its sponsoring organization.
5. COPYRIGHT AND LIMITATIONS ON USE: This web site, including, without limitation, the images and information contained herein, including but not limited to, the text, graphics or html code, are the property of Nicklaus Children's Hospital and are protected by copyright and other intellectual property laws. By using this site, you agree not to reproduce, retransmit, distribute, disseminate, sell, publish, broadcast, print or circulate any of the contents of this web site to anyone without the express, prior written consent of Nicklaus Children's Hospital. You may download any of these materials for your own personal, non-commercial use, as long as you do not remove any copyright or other proprietary notices from the downloaded materials.
6. GOVERNING LAW: Use of this web site shall be deemed to have occurred in the state of Florida. The terms of this disclaimer, notice and agreement shall be interpreted and enforced in accordance with Florida law. You agree to the exclusive jurisdiction and venue of the courts in Dade County, Florida, U.S.A. in all disputes arising out of or relating to the use of this web site. Use of this web site is unauthorized in any jurisdiction that does not give effect to all provisions contained in the above terms and conditions.
7. LACK OF CONFIDENTIALITY: Any communication or material that you transmit to this site by electronic mail or otherwise, including any data, questions, comments or suggestions, will be treated as non-confidential and non-proprietary.
Ethics & Compliance and Internal Audit
Ethics & Compliance
Nicklaus Children's Hospital is proud of its tradition of conducting its business in an ethical manner. To this end, Nicklaus Children's Hospital has established a compliance department and program to advance the prevention, detection and correction of violations of federal, state or local law or regulations governing health care and human services programs by employees, contractors of agents. Our compliance staff is available as valuable resources in your decision making processes or to answer questions regarding the ethical conduct of business practices at Nicklaus Children's Hospital.

Denise Longman
Chief Compliance Officer
(786) 624-3838
Send email
Cory Hall
Information Security Officer
(786) 624-6939
Send email
Lisa Arenas
Privacy Officer
(786) 624-3500
Send email
Internal Audit
Internal Auditing is an independent, objective, assurance and consulting activity that adds value to and improves an organization's operations. It helps an organization accomplish its objectives by bringing a systematic, disciplined approach to evaluate and improve the effectiveness of risk management, control, and governance processes.
Employee and Physician Login
Remote User Citrix Access
If you are connecting from home or a computer other than a Nicklaus Children's Hospital computer please click here to login to the NCHS Portal.
Process Improvement
We are dedicated to supporting an army of
curious problem solvers in their pursuit of:
Amazing Patient Care
Operational Excellence
Building the Future
The purpose of our Process Improvement Office is to:
- Facilitate operational and clinical continuous improvement across the organization.
- Connect the purpose and people of the organization from the top down and from the bottom up and across via formalized channels.
- Enable the mechanism for problems to be solved scientifically and locally, where they happen, when they happen, with top-level support to help build infrastructure to sustain improvement
The Process Improvement Team
The Process Improvement team is an exceptionally talented group who provide project facilitation, quality science training, and technical support, and analysis for accelerating clinical, and operational quality improvement across the organization.
Fahd Lahrech
Manager, Quality and Data Sciences
CPIM, CQE, CMfgE, ML, MS, LSSBB
(305) 793-9579
Email Fahd
Mary Szabo
Project Management Coordinator
(786) 564-0225
Email Mary
Lazaro Alfonso
Lead Quality Analytics Analyst
BSEE, BSMATH, MSEE, LSSBB
(786) 624-5080
Email Lazaro
William Smit
Data/Quality Program Analyst
BME, MSCE
(786) 624-2392
Email William
Notice of Privacy Practices
Effective date: March 26, 2013
(Revised: July 17, 2020)
You may also download this notice in PDF form:
THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND DISCLOSED AND HOW YOU CAN GET ACCESS TO THIS INFORMATION
PLEASE REVIEW IT CAREFULLY.
As a parent/legal guardian of a minor patient at Nicklaus Children’s Health System “NCHS”, you are the patient’s “personal representative.” When reading this Notice please understand that when we use the term “you” we mean the pediatric patient.
Applicability of Notice - This Notice describes the privacy practices of Nicklaus Children’s Health System and affiliated entities, including Nicklaus Children’s Hospital and outpatient facilities listed on the signature page. Each of these affiliated entities are legally separate covered entities, but for purposes of the HIPAA privacy rule designate themselves as a single covered entity and will each follow the terms of this Notice. For purposes of this Notice, the terms “NCHS,” “we” and “our” are used in this Notice to refer to Nicklaus Children’s Health System and its facilities and affiliated entities, including Nicklaus Children’s Hospital and outpatient facilities. Each of these entities may share information with each other for purposes of treatment, payment or health care operations as described in this Notice.
Privacy Obligations - NCHS is required by law to maintain the privacy of health information about you that can identify you (“Protected Health Information” or “PHI”), to provide you with this Notice of our legal duties and privacy practices with respect to your PHI, to notify you following a breach of protected health information and to abide by the terms of this Notice currently in effect. We reserve the right to change this Notice. We reserve the right to make the revised or changed Notice effective for medical information we already have about you as well as any information we receive in the future. We will post a copy of the current Notice in each of the locations identified below. The Notice will contain the effective date. A copy of the current Notice will be made available to you when you initially register with Nicklaus Children’s Health System for treatment or services, upon your request, and on subsequent visits if the Notice has been revised.
Our Pledge - We understand that all information about you and your health is personal. We are committed to protecting this information. When you receive services at NCHS, a medical record is created. This record describes the services provided to you and is needed to provide you with quality care and to comply with certain legal requirements.
This Notice applies to care generated by NCHS, whether made by a NCHS employee or a doctor involved in your care at NCHS. This Notice tells you about the ways in which we may use and disclose your medical information. It also describes your rights and certain obligations we have regarding the use and disclosure of your medical information.
HOW WE MAY USE AND DISCLOSE YOUR HEALTH INFORMATION
The following categories describe different ways in which we use your health information within NCHS and may release your information to persons and entities outside of NCHS. We have not listed every use or disclosure within the categories, but all permitted uses and disclosures will fall within one of the following categories:
Uses and Disclosures for Treatment, Payment and Health Care Operations: : Your PHI may be used to treat you, to obtain payment services provided to you and to conduct “health care operations” as described below:
Treatment: Your health information may be used and disclosed to provide treatment and other services to you – for example, to diagnose and treat your injury or illness. We may disclose your PHI to doctors, nurses, technicians, medical students, interns, or other personnel who are involved in taking care of you during your visit with us or to individuals outside of NCHS who are also part of your healthcare team.
Payment: Your PHI may be used and disclosed to your insurance company or other third party to collect payment for services. For example, we may need to give your health plan information about surgery you received while here so that they will pay us or reimburse you. We may also tell your health plan about a treatment you are going to receive to obtain prior approval or to determine whether your plan will cover the treatment.
Exception: If you pay out of pocket in full for a health care item or service, you have the right to restrict certain disclosures of your PHI to your health plan (see section on ‘Right to Request Restrictions’).
Health Care Operations: Your PHI may be used and disclosed in connection with our health care operations. For example, your PHI may be used to conduct quality assurance activities, such as for evaluating the quality and competence of physicians, nurses and other health care workers; to perform customer service activities, or for investigating complaints. We may also disclose this information to our business associates who assist us with administrative and other functions. We require our business associates to appropriately safeguard the health information of our patients.
Appointment Reminders/Treatment Alternatives/Health-Related Benefits and Services - We may use and disclose your PHI to contact you to provide appointment reminders or information about treatment alternatives or other health-related benefits and services that may be of interest to you.
Fundraising Activities - NCHS may use or disclose health information about you to contact you in an effort to raise money for our organization and its operations. We may disclose this information to the Nicklaus Children’s Health Foundation to assist us in our fundraising activities. Only contact information such as your name, address and telephone number, and the dates you received treatment or services at NCHS would be released. You have the right to opt out of fundraising communications at any time and your request must be honored. If you would like to opt-out of receiving fundraising communications, please notify our Privacy Officer in writing or make your opt-out request using the method provided to you with every fundraising communication.
SITUATIONS WHERE YOU HAVE AN OPPORTUNITY TO AGREE OR OBJECT TO USES AND DISCLOSURES OF YOUR PHI
Hospital Directory - Nicklaus Children’s Hospital may include your name, location in the hospital, general health condition (e.g. fair, stable, etc.), and religious affiliation in a patient directory without obtaining your authorization unless you object to inclusion in the directory. This information, except for your religious affiliation, may be released to people who ask for you by name. Your religious affiliation may be given to a member of the clergy, even if they don’t ask for you by name. This is so your family, friends and clergy can visit you in the hospital and generally know how you are doing.
Individuals Involved in Your Care or Payment for Your Care - Your PHI may be disclosed to a family member, friend or other person to the extent necessary to help with your health care or with payment for your health care. Before we disclose your medical information to a person involved in your health care or payment for your health care, we will provide you with an opportunity to object to such uses or disclosures. If you are not present, or in the event of your incapacity or an emergency, we will disclose your medical information based on our professional judgment of whether the disclosure would be in your best interest.
SPECIAL SITUATIONS THAT DO NOT REQUIRE YOUR AUTHORIZATION
In certain circumstances, federal or state laws may require or allow us to provide your PHI to the following agencies without any oral or written permission from you:
Public Health Authorities/Health Oversight Agencies - We may disclose your medical information for public health activities, including for the reporting of disease, injury, vital events such as birth or death, and for the conducting of public health surveillance, investigation and/or intervention. We may disclose your medical information to a health oversight agency for oversight activities authorized by law, including for audits, investigations, inspections, licensure or disciplinary actions, administrative and/or legal proceedings or actions.
Abuse or Neglect - In accordance with federal and state law, we may disclose your PHI when it concerns abuse, neglect, or domestic violence to you. We are required to report suspected child or vulnerable adult abuse or neglect to the Florida Department of Children and Families Central Abuse Hotline.
Department of Health and Human Services/Florida Agency for Health Care Administration (the “Agency”) - We may disclose your PHI when required by the United States Department of Health and Human Services as part of an investigation or a determination of our compliance with relevant laws. We may disclose your PHI to the agency for purposes of health care cost containment or in response to a subpoena.
In Connection with Judicial and Administrative Proceedings - We may disclose your PHI in any civil or criminal action, unless otherwise prohibited by law, in response to a court or administrative order or if compelled by subpoena at a deposition, evidentiary hearing, or trial, but only if efforts have been made to tell you about the request.
Law Enforcement - We may disclose your PHI to a law enforcement official or the medical examiner to alert them about a death we believe may be the result of criminal conduct. We may notify a law enforcement official if you were injured in a motor vehicle crash and your blood alcohol level is above the legal limit. We are required to report to local law enforcement officials any gunshot wound or life-threatening injuring indicating an act of violence.
National Security and Intelligence Organizations - We may disclose your PHI for specialized governmental functions, such as national security and intelligence activities, and for the provision of protective services to the President.
Coroners, Medical Examiners, and Funeral Directors - We may disclose your PHI to coroners, medical examiners or funeral directors consistent with applicable law to carry out their duties.
Organ and Tissue Donation Organizations - If you are an organ donor, we may disclose your medical information to an organ donation and procurement organization.
Workers’ Compensation Agents - We may release your PHI for workers’ compensation or similar programs.
Military Command Authorities - If you are a member of the armed forces, we may disclose your PHI as required by military command authorities.
Correctional Institutions - We may disclose your medical information to a correctional institution having lawful custody of you if doing so would be necessary for your health and the health and safety of other individuals.
Emergency Circumstances and Disaster Relief - Your PHI may be used or disclosed to a public or private entity authorized by law or by its charter to assist in disaster relief efforts (such as the Red Cross).
To Avert a Serious Threat to Health or Safety - We may use and disclose medical information about you when necessary to prevent a serious threat to your health and safety or the health and safety of the public or another person. Any disclosure, however, would only be to a government agency or authority that is able to help prevent the threat.
Research - Under certain circumstances and provided that your identity is protected, we may use and disclose medical information about you for statistical and research purposes, including research planning and the creation of research proposals as long as Protected Health Information is not removed, copied, or compromised.
As Required by Law - We will disclose your PHI when required to do so by federal, state or local law.
If a use or disclosure of health information described above in this Notice is prohibited or materially limited by state law, it is our intent to meet the requirements of the more stringent law.
SITUATIONS THAT REQUIRE YOUR AUTHORIZATION
Special Protections for HIV, Alcohol and Substance Abuse, Mental Health, and Genetic Information - State and/or federal laws may place restrictions on the manner in which specific types of PHI may be used and/or to whom such medical information may be disclosed, such as HIV status, alcohol and substance abuse treatment, psychiatric treatment, and genetic information. In those instances where the use and/or disclosure of this PHI is specifically restricted, we will seek appropriate authorization from you, your legal representative or a court of law/administrative tribunal before using or disclosing this information.
Marketing - We will not use your PHI for marketing purposes without your authorization. If you have consented to receive marketing information but no longer wish to receive further information, please notify our Privacy Officer in writing to make your opt-out request.
Sale of PHI - We will not disclose your PHI in return for any financial compensation without your authorization.
Research - We may share your health information with researchers after you have signed a specific written authorization for a specific research study. In very limited circumstances, we may share your health information with researchers when the Institutional Review Board (IRB) issues a waiver after having ensured that safeguards are in place to protect your privacy. An IRB is a committee responsible for protecting individual research subjects and ensuring that research is conducted ethically. All research projects are subject to special approval by the IRB. Your health information will not be used and you will not be asked to participate in a research project that is not reviewed and approved by an IRB.
Other Uses and Disclosure of Your PHI - Other uses and disclosures of your PHI not covered by this Notice or the laws that apply to NCHS will be made only with your written permission (authorization), which authorization may be revoked as described below.
YOUR RIGHTS REGARDING HEALTH INFORMATION ABOUT YOU
Right to Request Restrictions - You have the right to request limits on the use of your medical information for either treatment, payment or health care operations. You also have the right to request a limit on medical information we disclose to someone who is involved in your care or the payment of your care, such as a family member or friend. For example, you could ask that we not disclose information about a surgery you had. To request restrictions, the request must be made in writing to the Nicklaus Children’s Health System Health Information Management Department. If your health care provider believes it is in your best interest to permit use and disclosure of your protected health information, your protected health information will not be restricted. If Nicklaus Children’s Health System does agree to the requested restriction, we may not use or disclose your protected health information in violation of that restriction unless it is needed to provide emergency treatment.
Out-of-Pocket Payments - If you make a payment in full at the time of, or prior to, receiving an item or service from Nicklaus Children’s Health System, you have the right to request that your Protected Health Information with respect to that item or service not be disclosed to your Health Plan. We will honor your request as long as financial obligations are met.
Right to Request Confidential Communications - You have the right to request that we communicate with you about medical matters in a certain way or at a certain location. For example, you can ask that we only contact you at work or by mail. Your request must specify how or where you wish to be contacted. We will accommodate all reasonable requests. To request restrictions, the request must be made in writing to the Health Information Management Department.
Right to Inspect and Copy - You have the right to inspect and/or receive a copy of any medical information maintained about you that may be used to make decisions about your care or payment for your care. Typically, this will include your medical and billing records, but not psychotherapy notes. If your PHI is maintained in an electronic format (known as an electronic medical record or an electronic health record), you have the right to request that an electronic copy be given to you or transmitted to another individual or entity.
To inspect and/or get a copy of your medical or billing records you must submit your request in writing to:
Nicklaus Children’s Health System
Health Information Management Department
Attention: Director
3100 S.W. 62 Avenue
Miami, Florida 33155-3009
We may charge a reasonable fee for copying and mailing the records. We may deny your request in certain limited circumstances. If your request is denied, you may request that your denial be reviewed. Such reviews will be performed by an independent licensed healthcare professional chosen by our Privacy Officer. We will comply with the outcome of the review.
Right to Amend - If you feel that information about you is incorrect, you may ask us to amend the record. To request an amendment, the request must be made in writing to the Health Information Management Department at the address noted above. In addition, you must provide a reason that supports your request. We are not obligated to comply with your request to amend your record.
Right to Revoke your Authorization - If you provide us with authorization to use or disclose medical information about you, you may revoke that authorization, in writing, at any time. If you revoke your authorization, we will no longer use or disclose medical information about you for the reasons covered by your written authorization. We are unable to take back any disclosures we have already made with your permission and we are required to retain our records of the care that we provided to you. A form of written revocation is available upon request from our Health Information Management Department.
Breach Notification - In certain instances, you have the right to be notified in the event that we, or one of our Business Associates, discover an inappropriate use or disclosure of your health information. Notice of any such use or disclosure will be made in accordance with state and federal requirements.
Accounting of Disclosures - You have the right to request an «accounting of disclosures.» This is a list of disclosures that we have made of your PHI. We are not required to list certain disclosures, including (1) disclosures made for treatment, payment, and health care operations purposes, (2) disclosures made with your authorization, (3) disclosures made to create a limited data set, and (4) disclosures made directly to you. You must submit your request in writing to our Health Information Management Department. Your request must state a time period which may not be longer than 6 years before your request. Your request should indicate in what form you would like the accounting (for example, on paper or by e-mail). The first accounting you request within any 12-month period will be free. For additional requests, we may charge you for the reasonable costs of providing the accounting. We will notify you of the costs involved and you may choose to withdraw or modify your request before any costs are incurred.
Right to a Paper Copy of this Notice - You have a right to a paper copy of this Notice, even if you agreed to receive it electronically. Please contact us as directed below to obtain this Notice in written form.
Foreign Language Version - If you have difficulty reading or understanding English, you may request a copy of this Notice in Spanish or Creole. Additional languages or formats will be made available upon request.
QUESTIONS OR CONCERNS
If you would like more information about our privacy practices or have questions or concerns about this Notice, please contact our Privacy Officer at the number listed below.
If you believe your privacy rights have been violated, you may file a complaint, in writing, to the NCHS Privacy Officer located at:
Nicklaus Children’s Health System Privacy Officer
3100 S.W. 62 Avenue
Miami, Florida 33155-3009
Telephone: (786) 624-3838
or you may contact the Secretary of the U.S. Department of Health and Human Services (HHS).
To file a complaint with the U.S. Department of Health and Human Services, you may call toll free 1-877-696-6775 or visit the website of the Office of Civil Rights at www.hhs.gov/ocr/privacy. You can also mail a written request to:
Office for Civil Rights
U.S. Department of Health and Human Services
Sam Nunn Atlanta Federal Center
Suite 16T70
61 Forsyth Street, S.W.
Atlanta, GA 30303-8909
You will not be penalized or retaliated against in any way for making a complaint.
NICKLAUS CHILDREN’S HEALTH SYSTEM FACILITIES AND AFFILIATED ENTITIES
This Notice applies to the privacy practices of the following Nicklaus Children’s Health System facilities and Affiliated Entities:
Nicklaus Children’s Health System, Inc.
- Nicklaus Children’s Hospital
- Nicklaus Children’s Urgent Care Centers
- Nicklaus Children’s Outpatient Centers
- Nicklaus Children’s Pediatric Specialists
- Nicklaus Children’s Health System Foundation
For a list of entities click on the following link:
www.nicklauschildrens.org/locationsCommunity Health Needs Assessment & Implementation Plan
Every three years not-for-profit hospitals are required to conduct a Community Health Needs Assessment (CHNA) of the local populations they serve.
Our goal in conducting the assessment was to better understand the health status, behaviors, and needs of children and adolescents in South Florida so that we as a community – patients, families, Nicklaus Children’s, and partner organizations – can optimally support their health and wellbeing. Information on both the CHNA and Implementation Plan can be found below.
Implementation Plan Goals
Access to Community and Health Services
- Enhance access to timely, equitable and comprehensive medical, social, behavioral health and wellness services for children and their families in traditional and non-traditional settings.
- Increase care coordination and collaboration within the intersecting systems of health, social and community services (collaborators) through the development of collaborations.
- Continue to enhance hospital care coordination through new strategies that address culture, language, etc.
- Increase utilization of primary care and social service systems.
Health Education
- Empower parents and children to lead healthy lifestyles by providing culturally, linguistically, and developmentally tailored education and resources.
- Increase awareness of preventative primary care, and knowledge and utilization of appropriate levels of care, through educational campaigns and messages.
- Increase points of distribution for nutrition education materials and resources in each of The Children's Trust defined priority zip codes.
- Promote community understanding of comprehensive health and safety through the implementation of community initiatives.
Children’s Mental Health
- Promote overall mental wellness of children and adolescents by engaging an ecosystem of support and services for them and their families.
- Implement mental wellness initiatives for children and youth.
- Expand intervention services across the ecosystem for children and their families through collaborative initiatives.
- Increase skills and capacity throughout the ecosystem to respond to mental health crisis among children and youth through training opportunities.
Previous Reports
Application Requirements
We are now on NAFCAS!
There are two ways to apply to the Nicklaus Children's Administrative Fellowship Program:
- Apply via the National Administrative Fellowship Centralized Application Service (NAFCAS)website and then submit a copy of your NAFCAS application materials to our Career Portal by September 27, 2024 at 11:59PM EST.
- Apply directly through our Career Portal by September 27, 2024 at 11:59PM EST.
Applicants who apply via the Career Portal will be asked to upload:
- Resume
- Personal Statement (one page, single spaced, 11-point Times New Roman Font) answering the following questions:
- Why are you interested in Nicklaus Children's Health System?
- What are your future career objectives within healthcare administration?
- How will this fellowship help you to obtain your goals?
- Official graduate school transcripts (from all universities attended)
- Three letters of recommendation (1 professional, 1 academic, & 1 academic or professional)
Please note all documents uploaded to our career portal must be a single, combined PDF document.
Incomplete applications will not be considered.
Fellowship Application Timeline
Application Receipt Deadline: September 27, 2024 at 11:59PM EST
Selection Announcement: November, 2024
Start Date: June 2025 (Date Negotiable)
Qualifications
- Recent graduates with an MHA, MSHA, MHSA, MPH, MBA with an emphasis in healthcare management, or degree equivalent to the aforementioned studies.
- Applicants from CAHME accredited programs are strongly preferred.
- Applicants completing the fellowship as a requirement for graduation are welcome to apply.
Salary and Benefits
Nicklaus Children’s Health System will provide a salary that is competitive with the industry and a comprehensive benefits package that includes medical, dental, vision, life and disability insurance. In addition, reimbursement and travel expenses to one health care conference of the fellow’s choosing will be provided.
Selection Process
The fellowship selection process is highly competitive. Each application will be given careful review, upon which qualified applicants will be contacted for first-round phone-interviews. After the round of phone-interviews, selected candidates will be invited to further rounds of interviewing via video conference. Later, interviews with the executive leadership team will occur on-site, COVID-permitting.
Please note that completion of the one-year fellowship does not guarantee prolonged employment within Nicklaus Children’s Health System. Nicklaus Children’s Health System is an equal opportunity employer. Selection of applications will be conducted without regard to race, religion, creed, sex, national origin or disability.
Incomplete applications will not be considered. Again, please submit all materials as a consolidated PDF to the aforementioned contact person. Nicklaus Children’s maintains the right to modify the application timeline (selection dates) as time and schedules permit.
Project Work
The following list contains examples of past projects that fellows have worked on at Nicklaus Children's Hospital:
Past Projects
- Advanced Pediatric Care Pavilion Inpatient Demand Analysis
- Ambulatory Care Center Construction/Expansion
- Ambulatory Surgery Center Project Management
- Budget (Operational and Capital) Planning
- Developing Bioethics Committee
- Evaluating Value Based Care Programs
- Management Services Organization (MSO) Development and Coordination
- Master Facility Planning
- Observation Case Task Force
- Pediatric Health Optimization Program Development
- Population Health and Health System Integration Framework Development
- Primary Care Strategic Planning
- Process Improvement
- Service Provision Analyses for Joint Ventures
- Telehealth Strategic Planning, Development, and Operations
Frequently Asked Questions
Upon review of the following FAQs, if you are unable to find the information and answers you were looking for, please feel free to contact the current fellows.
Can I apply for the Nicklaus Children's Health System Administrative fellowship on NAFCAS?
Yes, applicants can now apply for our fellowship on the National Administrative fellowship Centralized Application Service (NAFCAS) website. Individual applications can still be submitted through the process outlined under the Application Requirements tab, if applicants choose not to utilize NAFCAS.
When are the application materials due?
September 27, 2024, at 11:59 p.m. EST. Applications received after this date will not be considered.
What documents should I submit for consideration of the 2025-2026 fellowship program?
Updated resume, official graduate school transcripts (from all institutions attended), completed Nicklaus Children’s Health System fellowship Application (including Personal Statement), and and 3 letters of recommendation (1 professional, 1 academic, & 1 academic or professional). All materials should be submitted as a consolidated PDF, letters of recommendation should be sent separately from recommendation writers.
When will the 2025-2026 fellows be selected?
Early November 2024 is when the selected fellows and all other applicants will be notified of a decision.
How long is the administrative fellowship and when is the start date?
One year (12 months) beginning in June or July (negotiable).
How many fellows are selected each year?
Two.
Can the current fellows be contacted with further questions about the application/fellowship experience to date?
Absolutely. Comments and questions are most welcome. You can reach the current fellows via email at Adminfellows@NicklausHealth.org
How long has the Nicklaus Children’s fellowship Program existed?
The fellowship program has existed for over 12 years.
Can the administrative fellowship program substitute as the administrative residency requirement for my university’s degree program?
Yes, it can serve as a substitute for university required administrative residencies.
Does the administrative fellowship choose students from any university?
Nicklaus Children’s has a strong preference for choosing qualifying applicants from a CAHME-accredited graduate program, but applicants from non-CAHME-accredited programs will also be considered.
Will applicants to the program be notified of the status of their final application?
Yes, all applicants who are no longer considered for the fellowship program will be notified in writing on a timely basis.
Will the fellows have the opportunity to attend senior leadership meetings?
Yes. The fellows will have many opportunities to attend a diverse range of meetings throughout the organization, including but not limited to Executive Leadership Team (ELT) meetings, Board of Directors meetings, finance and investment committees, technology committees, physician advisory councils, chiefs and heads (medical executive meetings), and health system strategic planning meetings.
Are rotations preselected or based on the interest of the fellows?
The fellows must rotate through core departments, which include Finance, Clinical Service Lines, Information Technology, and Hospital Operations areas. In addition to these rotations, the fellows will have full opportunity to select specific areas of interest for rotation.
What facilities are owned/operated by Nicklaus Children's Health System?
Please visit our Locations page for a full list of facilities.
Where will the fellows be based?
The fellows will be based at the Main Campus (Miami, FL) but there will be sufficient opportunity to assist at each of the health system’s entities.
Is there a requirement that the fellows accept a position after completing the fellowship?
No.
Is there any obligation for Nicklaus Children’s to hire the fellows upon completion of the fellowship program?
No.
Is there a requirement that the fellows be bilingual in English and Spanish?
No. However, fluent or at least conversational Spanish will be helpful in your interaction with the culture of Miami.
About Miami, Florida
Culture
Greater Miami is so much more than a tropical getaway. The city, its many neighborhoods, and beaches are a vibrant departure from the ordinary, offering vast array of culture through music, museums, galleries, theater performances and exciting festivals that take place throughout the year.
Attractions
Recreation and Sports
Professional Associations
Links available in this page are not necessarily endorsed, reviewed, or sponsored by Nicklaus Children's Hospital, by clicking on any of the links, you will be leaving Nicklaus Children's Website.
Previous Fellows
Current Administrative Fellows
2024-2025 Fellow
Katrina Piccolo, MHA
University of Miami
Administrative Fellow
Nicklaus Children’s Health System
Email: adminfellow@NicklausHealth.org
2024-2025 Fellow
Lauren Stekler, MHA
Columbia University
Administrative Fellow
Nicklaus Children’s Health System
Email: adminfellow@NicklausHealth.org
Previous Administrative Fellows
2023 - 2024 Fellow
Meredith Steinfeldt, MPH
Tufts University School of Medicine
Manager, Administrative Services
Nicklaus Children’s Health System
Email: meredith.steinfeldt@NicklausHealth.org
2022 – 2023 Fellow
Madeline Cremin, MHA
University of Missouri School of Medicine
Business Analyst
Mayo Clinic
2021 - 2022 Fellow
Leigh Bouskila, MHA
Columbia University Mailman School of Public Health
Director, Practice Development & Support Services
Nicklaus Children’s Health System
Email: leigh.bouskila@nicklaushealth.org
2020 - 2021 Fellow
Alex Wolfred, MHSA
Xavier University
Implementation Manager, Population Health & Wellness
Kroger Health
2019 - 2020 Fellow
Megan Murphy, MBA, MHA
University of Missouri
Manager, Telemedicine
University of Missouri Health Care
2018 - 2019 Fellow
Jasmine Oesch, MHSA
University of Michigan
Senior Project Manager, Division of General Medicine
Michigan Medicine
2017 - 2018 Fellow
Mayra Caswell, MHA
Tulane University
Grant Coordinator
CMC Community Health Foundation
2016 - 2017 Fellow
Umar Ahmad, MHA
Texas State University
Program Manager
UNC Health Care
2015 - 2016 Fellow
Sofia Debs, MHA
Saint Louis University
Manager, Healthcare Strategy
Baptist Health South Florida
2014 - 2015 Fellow
Brian Gurucharri, MHA
University of Florida
Associate Administrator
Manatee Memorial Hospital
2013 - 2014 Fellow
Peter Carr, MHSA, MSHI
The University of Alabama at Birmingham
Director, Digital Health & Innovation
Moffitt Cancer Center
2012 - 2013 Fellow
Briana (Rader) Sikir, MSHA
The University of Alabama at Birmingham
Program Manager, Strategy and Business Development
Northwestern Medicine
Meet the Pediatric Hospitalist Team
Pediatric Urology Success Stories
Patient Stories
Patient Stories
Patient Stories
Conditions We Treat
The Division of Neurosurgery offers state of the art surgical management of disorders of the nervous system including:
Patient Stories
Special Procedures
Among the special procedures performed by the ENT physicians at Nicklaus Children's are:
- Head and neck cancer and tumor surgery
- Diagnostic and therapeutic surgery for pediatric airway disorders
- Speech fluoroscopy
- Removal of foreign bodies from the ears, nose and throat
- Treatment for complex head and neck tumors
- Treatment of symptoms resulting from cystic fibrosis
- Tonsillectomy and adenoidectomy for children with bleeding disorders
- Routine procedures performed on children with high-risk medical problems
- Evaluation and treatment for facial trauma
- Routine and complex surgery for pediatric sinus disease
- Treatment for craniofacial disorders
- Treatment for complex airway diseases
- Treatment for various pediatric otology and neurotology diseases, including mastoid disorders and tumors of the cerebellopontine angle
- Additionally, physicians perform reconstruction of the eardrum or associated ossicles and repair of congenital aural atresia
Patient Stories
Patient Stories
Important Resources for Children with Special Needs
Health and Safety Resources
| For information on Emergency Services: |
| Helpine |
856-764-6940 |
| Immunization Hotline |
800-232-4636 |
| Poison Control |
800-222-1222 |
| Car seat installation & safety |
305-471-1716 |
| Health Department |
305-324-2400 |
| Children’s Medical Services (North Office) |
305-349-1330 |
| Children's Medical Services (South Office) |
786-624-5700 |
| American Heart Association |
954-364-5000 |
| Dade County Safe Kids Coalition |
305-663-6800 |
| Switchboard of Miami |
305-358-4357 |
| Water Safety |
305-644-1200 |
Financial Support
| For Information about Economic/Financial Support for Families in Need: |
Economic Self-sufficient Services
(Temporary assistance for needy families) |
850-300-4353 |
| Florida Kid Care (Free health insurance) |
888-540-5437 |
| Social Security Administration |
800-772-1213 |
| Medicaid |
800-300-4323 |
| Women & Infant Care Program (WIC) |
786-336-1300 |
| Special Transportation Services (STS) |
305-630-5301 |
| For Information about Breastfeeding: |
| La Leche League |
1-800-525-3243 |
Child Care
| For Help in Finding and using Childcare: |
| Headstart and Early Headstart |
786-409-4622 |
| Childcare Resource and Referral Hotline |
866-357-3239 |
| Early Learning Coalition |
305-646-7220 Miami-Dade
305-296-5557 Monroe |
Parenting & Child Guidance/Nicklaus
Children's Hospital Preventive Medicine |
305-666-6511, ext. 4268 |
Child Development
| For Information on Children's Evaluations or Services Related to a Developmental Delay or Disability (Birth-three years): |
| University of Miami Early Steps North Dade |
305-243-5600 |
| Dade County Public Schools |
305-995-1000 |
| Child Find FDLRS |
305-274-3501 |
Department of Children & Families Office of
Developmental services |
800-232-4636 |
| Information on Child Development- Family Health Line |
800-451-BABY |
| For Support and Information about Parenting Challenges: |
| Helpline |
1-855-427-2736 |
| Advocacy Network for Disabilities |
305-596-1160 |
| Family Counseling Services |
305-271-9800 |
| Family Network on Disabilities of Florida |
800-825-5736 |
| Parents as Teachers |
813-974-7875 |
| Parent to Parent of Miami |
305-271-9797 |
| For Assistance Translating into Another Language: |
| Nicklaus Children's Hospital Switchboard Operator Will assist you |
305-666-6511 |
| AT & T Language Line |
800-643-2255 |
| For Economic & Family Support: |
Legal Aid (provides free legal assistance to people
with disabilities, low income or elderly citizens) |
305-579-5733 |
| Miami Dade Transit Information |
305-770-3131 |
Other Important Resources
Dental Health Patient Education
The following information guides are provided to educate patients in the most common dental concerns in children and children with specific conditions or diseases that require extra care to maintain healty teeth.
Telemedicine
Nicklaus Children's Hospital's Telehealth Center is a high-tech program designed to advance pediatric care for children around the world through enhanced access to pediatric subspecialty physicians and remote reading of diagnostic tests by highly trained experts.
For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org

Physician-to-Physician Videoconferencing
The center makes possible sophisticated videoconferencing, bringing together referring physicians from countries all over the world to consult with renowned subspecialty physicians based at Nicklaus Children's Hospital. Physician-to-physician consultative offerings include:

- Pediatric subspecialist consults
- Emergency care consults
- Complex multi-specialty team consultations
- Second opinions
Remote Reading of Diagnostic Tests
Nicklaus Children's Hospital also offers remote reading of diagnostic tests. The imaging teams at Nicklaus Children's Hospital, are among the region’s most experienced at reviewing and interpreting diagnostic tests.
Consultative Services with a Pediatric Leader
Nicklaus Children's Hospital, is one of the leading pediatric hospitals in the United States, with a 650-member medical staff that includes experts in virtually every pediatric subspecialty.
Consultations can be scheduled with individual subspecialists or a team of subspecialists as needed. Medical translation services are also provided when needed to support communications.
Offering Benefits for Overseas Patients and Partners
The Telehealth Center offers benefits to our overseas patients, physician colleagues and insurers.
- Participation in plan of care
- Educational opportunities
- Quality service offerings
- Efficient response time
Benefits to Overseas Patients
Physician-to-physician consultative services benefit patients in many ways. Families avoid the stress and expense of traveling, saving on airfare, local transportation and accommodations. They also avoid missing school and work days.
For More Information
The Nicklaus Children's Hospital Telehealth Center is a service of Global Health Services, which offers coordinated care and ease of access for international children and their families. For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org
Telemedicine
Nicklaus Children's Hospital's Telehealth Center is a high-tech program designed to advance pediatric care for children around the world through enhanced access to pediatric subspecialty physicians and remote reading of diagnostic tests by highly trained experts.
For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org

Physician-to-Physician Videoconferencing
The center makes possible sophisticated videoconferencing, bringing together referring physicians from countries all over the world to consult with renowned subspecialty physicians based at Nicklaus Children's Hospital. Physician-to-physician consultative offerings include:

- Pediatric subspecialist consults
- Emergency care consults
- Complex multi-specialty team consultations
- Second opinions
Remote Reading of Diagnostic Tests
Nicklaus Children's Hospital also offers remote reading of diagnostic tests. The imaging teams at Nicklaus Children's Hospital, are among the region’s most experienced at reviewing and interpreting diagnostic tests.
Consultative Services with a Pediatric Leader
Nicklaus Children's Hospital, is one of the leading pediatric hospitals in the United States, with a 650-member medical staff that includes experts in virtually every pediatric subspecialty.
Consultations can be scheduled with individual subspecialists or a team of subspecialists as needed. Medical translation services are also provided when needed to support communications.
Offering Benefits for Overseas Patients and Partners
The Telehealth Center offers benefits to our overseas patients, physician colleagues and insurers.
- Participation in plan of care
- Educational opportunities
- Quality service offerings
- Efficient response time
Benefits to Overseas Patients
Physician-to-physician consultative services benefit patients in many ways. Families avoid the stress and expense of traveling, saving on airfare, local transportation and accommodations. They also avoid missing school and work days.
For More Information
The Nicklaus Children's Hospital Telehealth Center is a service of Global Health Services, which offers coordinated care and ease of access for international children and their families. For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org
Patient Stories
Cardiac Intensive Care Unit (CICU)
Treatment and Procedures
Heart Institute Videos
Congenital Heart Surgery Real Time Outcomes ℠
Pediatric Interventional Cardiology
Pediatric Cardiovascular Surgery
Pediatric Cardiovascular Surgery
Meet the Pediatric Cardiology Team
EMTALA
IT’S THE LAW!
IF YOU HAVE A MEDICAL EMERGENCY OR ARE IN LABOR,
YOU HAVE THE RIGHT TO RECEIVE:
Within the capabilities of this Hospital’s staff and facilities
AN APPROPRIATE MEDICAL SCREENING EXAMINATION
NECESSARY STABILIZING TREATMENT
(including treatment for an unborn child)
APPROPRIATE TRANSFER TO ANOTHER FACILITY (if necessary)
ABOVE SERVICES WILL BE RENDERED, EVEN IF YOU ARE UNABLE
TO PAY, DO NOT HAVE MEDICAL INSURANCE OR ARE NOT
ENTITLED TO MEDICAID.
This hospital does participate in the Medicaid Program.
¡ES LA LEY!
SI TIENE UNA EMERGENCIA MÉDICA O ESTÁ EN PROCESO DE PARTO,
USTED TIENE EL DERECHO A RECIBIR:
Dentro de las capacidades del personal de este hospital e instalaciones
UN EXAMEN MÉDICO DE EVALUACIÓN ADECUADO
EL TRATAMIENTO NECESARIO PARA SU ESTABILIZACIÓN
(incluyendo el tratamiento de un niño por nacer)
TRANSFERENCIA ADECUADA A OTRO CENTRO (si es necesario)
LOS SERVICIOS ARRIBA DESCRITOS SERÁN PROVEIDOS
INCLUSO SI USTED NO PUEDE PAGAR, NO TIENE SEGURO MÉDICO
O NO TIENE DERECHO A MEDICAID.
Este hospital participa en el programa de Medicaid.
SE LA LWA
SI OU GENYEN YON IJANS MEDIKAL
OSINON OU GENYEN TRANCHE POU OU AKOUCHE,
OU DWE KAPAB JWEN SÈVIS IJAN SILA YO
(Selon moyen ak kalifikasyon amplwaye yo ki nan lopital la).
OU DWE RESEVWA YON BON EKZAMEN MEDIKAL ANSANM AK
TRETMAN KI NESESÈ POU ESTABILIZE KONDISYON MEDIKAL LA
(Menm pou yon ti bebe ki poko fèt)
SI LI NESESÈ, SE POU YO TRANSFERE OU NAN YON
LOPITAL KI PI KALIFYE POU SWEN SA YO.
OU DWE KAPAB JWEN SÈVIS SILA YO, MENM SI KE OU PAKAB PEYE,
OSINON KE OU PA TA GENYEN ASIRANS MEDIKAL,
OUBYEN ANKO KE OU PA KALIFYE POU ED LETA (MEDICAID).
Lopital sa a patisipe nan program nan medicaid.
Patient Stories
fMRI Studies (Functional Magnetic Resonance Imaging)
What is fMRI?
Functional magnetic resonance imaging (fMRI) is a development of MRI techniques that allows visualization of brain functions related to specific tasks. The study does not require any substance to be administered since it is based on the indigenous brain vascular response, requiring only cooperation for periods ranging from 15 to 60 minutes.
To date, several tasks have been utilized for mapping the brain cortex. Simple tasks include stimuli based on presentation of light, colors, tones, chords, music, syllables, movement of fingers and basic sensory perceptions. More complex and refined experiments have been implemented to map subtle cognitive functions. Currently, there is a vast armamentarium for mapping memory, attention, inhibition, face recognition, sensory discrimination, fear, etc.
However, most fMRI work has been directed in mapping language. Language mapping has been performed in children and adults. Reading, listening to meaningful text, generating words, making semantic decisions, are the most frequent paradigms described in the abundant current literature on fMRI. The technique has received ample acceptance among neuroscientists interested in epilepsy for the potential it has to become a tool to replace the Wada test.
Functional MRI is based on small signal changes that result from the following cascade of events. A task elicits activation in one or several brain areas. These areas increase their metabolic demands, suffer vasodilatation, and alter their levels of deoxyhemoglobin and oxyhemoglobin. Since deoxyhemoglobin is a paramagnetic molecule, it influences the phase of local proton-spins, altering the source signal that is converted into images. Therefore, the image is a representation of local changes of levels of deoxyhemoglobin, related to the brain region performing a task.
Although fMRI is almost risk-free, it cannot be performed in patients with claustrophobia, metal implants, wires and pace-makers. Patients with vagal nerve stimulators, or dental braces, may be included. However, some degradation of the images is expected.
Research and studies conducted by:
Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
Go to a Section
Clinical Cases Language Mapping Auditory Mapping 3D fMRI
fMRI in Sedated Children
fMRI Studies (Functional Magnetic Resonance Imaging)
What is fMRI?
Functional magnetic resonance imaging (fMRI) is a development of MRI techniques that allows visualization of brain functions related to specific tasks. The study does not require any substance to be administered since it is based on the indigenous brain vascular response, requiring only cooperation for periods ranging from 15 to 60 minutes.
To date, several tasks have been utilized for mapping the brain cortex. Simple tasks include stimuli based on presentation of light, colors, tones, chords, music, syllables, movement of fingers and basic sensory perceptions. More complex and refined experiments have been implemented to map subtle cognitive functions. Currently, there is a vast armamentarium for mapping memory, attention, inhibition, face recognition, sensory discrimination, fear, etc.
However, most fMRI work has been directed in mapping language. Language mapping has been performed in children and adults. Reading, listening to meaningful text, generating words, making semantic decisions, are the most frequent paradigms described in the abundant current literature on fMRI. The technique has received ample acceptance among neuroscientists interested in epilepsy for the potential it has to become a tool to replace the Wada test.
Functional MRI is based on small signal changes that result from the following cascade of events. A task elicits activation in one or several brain areas. These areas increase their metabolic demands, suffer vasodilatation, and alter their levels of deoxyhemoglobin and oxyhemoglobin. Since deoxyhemoglobin is a paramagnetic molecule, it influences the phase of local proton-spins, altering the source signal that is converted into images. Therefore, the image is a representation of local changes of levels of deoxyhemoglobin, related to the brain region performing a task.
Although fMRI is almost risk-free, it cannot be performed in patients with claustrophobia, metal implants, wires and pace-makers. Patients with vagal nerve stimulators, or dental braces, may be included. However, some degradation of the images is expected.
Research and studies conducted by:
Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
Go to a Section
Clinical Cases Language Mapping Auditory Mapping 3D fMRI
fMRI in Sedated Children
fMRI Studies (Functional Magnetic Resonance Imaging)
What is fMRI?
Functional magnetic resonance imaging (fMRI) is a development of MRI techniques that allows visualization of brain functions related to specific tasks. The study does not require any substance to be administered since it is based on the indigenous brain vascular response, requiring only cooperation for periods ranging from 15 to 60 minutes.
To date, several tasks have been utilized for mapping the brain cortex. Simple tasks include stimuli based on presentation of light, colors, tones, chords, music, syllables, movement of fingers and basic sensory perceptions. More complex and refined experiments have been implemented to map subtle cognitive functions. Currently, there is a vast armamentarium for mapping memory, attention, inhibition, face recognition, sensory discrimination, fear, etc.
However, most fMRI work has been directed in mapping language. Language mapping has been performed in children and adults. Reading, listening to meaningful text, generating words, making semantic decisions, are the most frequent paradigms described in the abundant current literature on fMRI. The technique has received ample acceptance among neuroscientists interested in epilepsy for the potential it has to become a tool to replace the Wada test.
Functional MRI is based on small signal changes that result from the following cascade of events. A task elicits activation in one or several brain areas. These areas increase their metabolic demands, suffer vasodilatation, and alter their levels of deoxyhemoglobin and oxyhemoglobin. Since deoxyhemoglobin is a paramagnetic molecule, it influences the phase of local proton-spins, altering the source signal that is converted into images. Therefore, the image is a representation of local changes of levels of deoxyhemoglobin, related to the brain region performing a task.
Although fMRI is almost risk-free, it cannot be performed in patients with claustrophobia, metal implants, wires and pace-makers. Patients with vagal nerve stimulators, or dental braces, may be included. However, some degradation of the images is expected.
Research and studies conducted by:
Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
Go to a Section
Clinical Cases Language Mapping Auditory Mapping 3D fMRI
fMRI in Sedated Children
fMRI Studies (Functional Magnetic Resonance Imaging)
What is fMRI?
Functional magnetic resonance imaging (fMRI) is a development of MRI techniques that allows visualization of brain functions related to specific tasks. The study does not require any substance to be administered since it is based on the indigenous brain vascular response, requiring only cooperation for periods ranging from 15 to 60 minutes.
To date, several tasks have been utilized for mapping the brain cortex. Simple tasks include stimuli based on presentation of light, colors, tones, chords, music, syllables, movement of fingers and basic sensory perceptions. More complex and refined experiments have been implemented to map subtle cognitive functions. Currently, there is a vast armamentarium for mapping memory, attention, inhibition, face recognition, sensory discrimination, fear, etc.
However, most fMRI work has been directed in mapping language. Language mapping has been performed in children and adults. Reading, listening to meaningful text, generating words, making semantic decisions, are the most frequent paradigms described in the abundant current literature on fMRI. The technique has received ample acceptance among neuroscientists interested in epilepsy for the potential it has to become a tool to replace the Wada test.
Functional MRI is based on small signal changes that result from the following cascade of events. A task elicits activation in one or several brain areas. These areas increase their metabolic demands, suffer vasodilatation, and alter their levels of deoxyhemoglobin and oxyhemoglobin. Since deoxyhemoglobin is a paramagnetic molecule, it influences the phase of local proton-spins, altering the source signal that is converted into images. Therefore, the image is a representation of local changes of levels of deoxyhemoglobin, related to the brain region performing a task.
Although fMRI is almost risk-free, it cannot be performed in patients with claustrophobia, metal implants, wires and pace-makers. Patients with vagal nerve stimulators, or dental braces, may be included. However, some degradation of the images is expected.
Research and studies conducted by:
Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
Go to a Section
Clinical Cases Language Mapping Auditory Mapping 3D fMRI
fMRI in Sedated Children
fMRI Studies (Functional Magnetic Resonance Imaging)
What is fMRI?
Functional magnetic resonance imaging (fMRI) is a development of MRI techniques that allows visualization of brain functions related to specific tasks. The study does not require any substance to be administered since it is based on the indigenous brain vascular response, requiring only cooperation for periods ranging from 15 to 60 minutes.
To date, several tasks have been utilized for mapping the brain cortex. Simple tasks include stimuli based on presentation of light, colors, tones, chords, music, syllables, movement of fingers and basic sensory perceptions. More complex and refined experiments have been implemented to map subtle cognitive functions. Currently, there is a vast armamentarium for mapping memory, attention, inhibition, face recognition, sensory discrimination, fear, etc.
However, most fMRI work has been directed in mapping language. Language mapping has been performed in children and adults. Reading, listening to meaningful text, generating words, making semantic decisions, are the most frequent paradigms described in the abundant current literature on fMRI. The technique has received ample acceptance among neuroscientists interested in epilepsy for the potential it has to become a tool to replace the Wada test.
Functional MRI is based on small signal changes that result from the following cascade of events. A task elicits activation in one or several brain areas. These areas increase their metabolic demands, suffer vasodilatation, and alter their levels of deoxyhemoglobin and oxyhemoglobin. Since deoxyhemoglobin is a paramagnetic molecule, it influences the phase of local proton-spins, altering the source signal that is converted into images. Therefore, the image is a representation of local changes of levels of deoxyhemoglobin, related to the brain region performing a task.
Although fMRI is almost risk-free, it cannot be performed in patients with claustrophobia, metal implants, wires and pace-makers. Patients with vagal nerve stimulators, or dental braces, may be included. However, some degradation of the images is expected.
Research and studies conducted by:
Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
Go to a Section
Clinical Cases Language Mapping Auditory Mapping 3D fMRI
fMRI in Sedated Children
Service Locations
At Nicklaus Children's, not only do we offer pediatric imaging excellence, we also offer convenience.
Main Hospital Campus Service Hours
Nicklaus Children's Hospital (Main Campus) in Coral Gables
Monday – Friday: 5:45 A.M. to 8:00 P.M.
Saturday: 5:45 A.M. to 8:00 P.M.
Sunday: 7:00 A.M. to 12:00 P.M.
Self-scheduling Hospital X-ray Services
As part of Nicklaus Children’s Hospital’s ongoing focus on enhancing service access for patient families, we now offer self-scheduling of X-rays (for the main hospital campus). To self-schedule an X-ray, fill out the Central Scheduling request form, when selecting a procedure, choose Radiology/Digital X-ray. You will then be presented with a series of available dates/times to choose from. Complete the form, and submit your request.
*Scoliosis series and full length bone service not available in outpatient centers.
EOS Imaging System
The EOS x-ray is the first technology that creates full-body 3D images of patients in a natural, standing position. While it provides orthopedic imaging for patients with spine, hip, and leg disorders, the EOS scanner also produces much less radiation than traditional scanners do. In fact, this technology forms high-quality images with radiation levels up to nine times less than a computed radiography x-ray, and 20 times less than a CT scan.
What is an EOS scan like?
When your child comes in for EOS medical imaging, they will stand inside the machine for about 30 seconds. Unlike traditional x-rays, the EOS scanners produce such small amounts of radiation that protective lead aprons are not necessary.
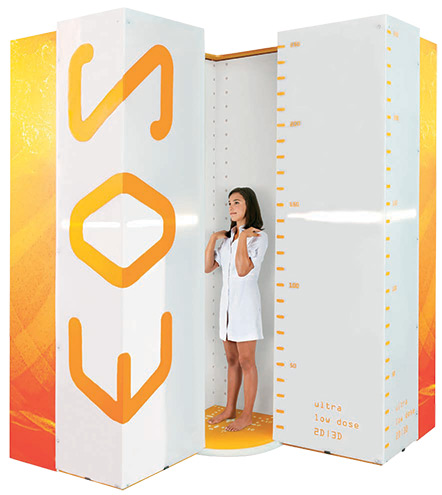
What are the benefits of EOS imaging?
An EOS scan creates a comprehensive 3D image, making it much more accurate than other scanners (all other x-rays require piecing multiple pictures together to approximate). And because the chamber allows the patient to stand up straight, the images reflect the most realistic depiction of posture. For patients with ongoing concerns such as scoliosis, the EOS Imaging System offers shorter scanning times than a traditional x-ray while producing a fraction of the radiation. This makes it both safer and more convenient for routine visitors.
Key Aspects of the EOS Imaging System
Patients with scoliosis typically undergo imaging every three to six months over a period of several years, which can amount to more than 20 total scans over the course of treatment. This technology makes possible high-quality images with a radiation dose up to nine times less than a computed radiography X-ray and up to 20 times less than a CT scan, enabling clinicians to make a more informed diagnosis and create individualized treatment plans for children with musculoskeletal disorders. The device also reduces the amount of time it takes to conduct a radiological scan.
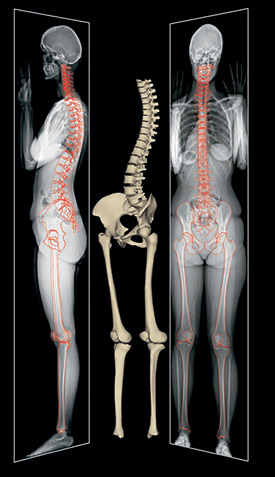
Leaders in EOS radiology
The Radiology Department at Nicklaus Children’s Hospital housed the first EOS medical Imaging System in the Miami-Dade area and the second in the state of Florida. A leader in pediatric radiology, we produced 120,000 radiological images in 2012 and have served thousands since. At Nicklaus Children’s Hospital, we offer the most advanced technology to ensure your child receives the highest quality care possible.
EOSEdge: The Newest Spine Imaging Technology Reduces Radiation Exposure
At Nicklaus Children's Hospital, we are committed to providing our patients and their families with the best care and technology available. This focus has led to our recent acquisition of the EOSedge™, an imaging system that delivers high-quality, three-dimensional full-body images of patients in a standing position using low-dose radiation.
EOSedge has a unique setting called Flex DoseTM that adjusts the amount of radiation patients receive. This setting minimizes exposure of areas of the body when possible, while still delivering the high- resolution images needed for our doctors to make treatment decisions. EOSedge is now available at Nicklaus Children’s Hospital’s main campus.
The Center for Spinal Disorders at Nicklaus Children's has been using EOS imaging systems for its pediatric spine patients since 2013.
EOS Imaging System
The EOS x-ray is the first technology that creates full-body 3D images of patients in a natural, standing position. While it provides orthopedic imaging for patients with spine, hip, and leg disorders, the EOS scanner also produces much less radiation than traditional scanners do. In fact, this technology forms high-quality images with radiation levels up to nine times less than a computed radiography x-ray, and 20 times less than a CT scan.
What is an EOS scan like?
When your child comes in for EOS medical imaging, they will stand inside the machine for about 30 seconds. Unlike traditional x-rays, the EOS scanners produce such small amounts of radiation that protective lead aprons are not necessary.
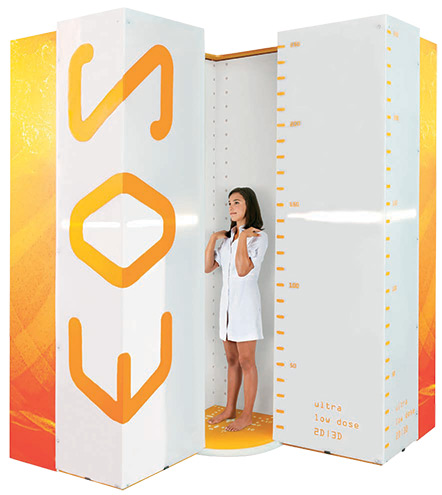
What are the benefits of EOS imaging?
An EOS scan creates a comprehensive 3D image, making it much more accurate than other scanners (all other x-rays require piecing multiple pictures together to approximate). And because the chamber allows the patient to stand up straight, the images reflect the most realistic depiction of posture. For patients with ongoing concerns such as scoliosis, the EOS Imaging System offers shorter scanning times than a traditional x-ray while producing a fraction of the radiation. This makes it both safer and more convenient for routine visitors.
Key Aspects of the EOS Imaging System
Patients with scoliosis typically undergo imaging every three to six months over a period of several years, which can amount to more than 20 total scans over the course of treatment. This technology makes possible high-quality images with a radiation dose up to nine times less than a computed radiography X-ray and up to 20 times less than a CT scan, enabling clinicians to make a more informed diagnosis and create individualized treatment plans for children with musculoskeletal disorders. The device also reduces the amount of time it takes to conduct a radiological scan.
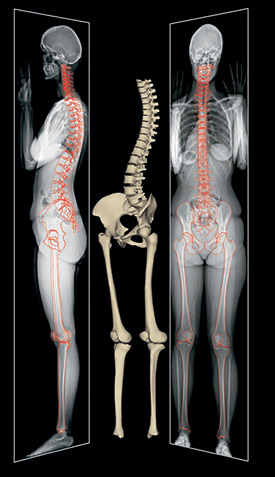
Leaders in EOS radiology
The Radiology Department at Nicklaus Children’s Hospital housed the first EOS medical Imaging System in the Miami-Dade area and the second in the state of Florida. A leader in pediatric radiology, we produced 120,000 radiological images in 2012 and have served thousands since. At Nicklaus Children’s Hospital, we offer the most advanced technology to ensure your child receives the highest quality care possible.
EOSEdge: The Newest Spine Imaging Technology Reduces Radiation Exposure
At Nicklaus Children's Hospital, we are committed to providing our patients and their families with the best care and technology available. This focus has led to our recent acquisition of the EOSedge™, an imaging system that delivers high-quality, three-dimensional full-body images of patients in a standing position using low-dose radiation.
EOSedge has a unique setting called Flex DoseTM that adjusts the amount of radiation patients receive. This setting minimizes exposure of areas of the body when possible, while still delivering the high- resolution images needed for our doctors to make treatment decisions. EOSedge is now available at Nicklaus Children’s Hospital’s main campus.
The Center for Spinal Disorders at Nicklaus Children's has been using EOS imaging systems for its pediatric spine patients since 2013.
EOS Imaging System
The EOS x-ray is the first technology that creates full-body 3D images of patients in a natural, standing position. While it provides orthopedic imaging for patients with spine, hip, and leg disorders, the EOS scanner also produces much less radiation than traditional scanners do. In fact, this technology forms high-quality images with radiation levels up to nine times less than a computed radiography x-ray, and 20 times less than a CT scan.
What is an EOS scan like?
When your child comes in for EOS medical imaging, they will stand inside the machine for about 30 seconds. Unlike traditional x-rays, the EOS scanners produce such small amounts of radiation that protective lead aprons are not necessary.
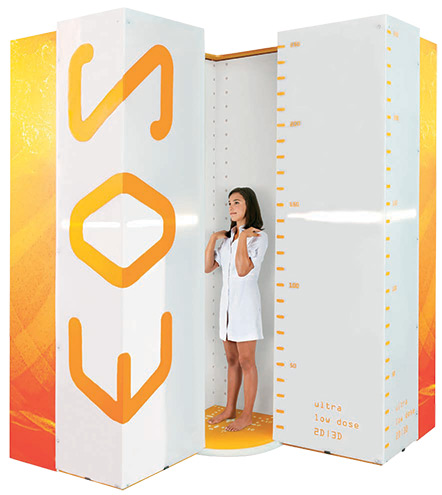
What are the benefits of EOS imaging?
An EOS scan creates a comprehensive 3D image, making it much more accurate than other scanners (all other x-rays require piecing multiple pictures together to approximate). And because the chamber allows the patient to stand up straight, the images reflect the most realistic depiction of posture. For patients with ongoing concerns such as scoliosis, the EOS Imaging System offers shorter scanning times than a traditional x-ray while producing a fraction of the radiation. This makes it both safer and more convenient for routine visitors.
Key Aspects of the EOS Imaging System
Patients with scoliosis typically undergo imaging every three to six months over a period of several years, which can amount to more than 20 total scans over the course of treatment. This technology makes possible high-quality images with a radiation dose up to nine times less than a computed radiography X-ray and up to 20 times less than a CT scan, enabling clinicians to make a more informed diagnosis and create individualized treatment plans for children with musculoskeletal disorders. The device also reduces the amount of time it takes to conduct a radiological scan.
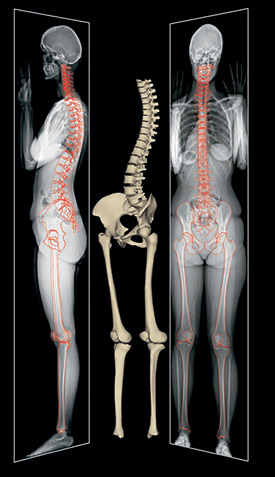
Leaders in EOS radiology
The Radiology Department at Nicklaus Children’s Hospital housed the first EOS medical Imaging System in the Miami-Dade area and the second in the state of Florida. A leader in pediatric radiology, we produced 120,000 radiological images in 2012 and have served thousands since. At Nicklaus Children’s Hospital, we offer the most advanced technology to ensure your child receives the highest quality care possible.
EOSEdge: The Newest Spine Imaging Technology Reduces Radiation Exposure
At Nicklaus Children's Hospital, we are committed to providing our patients and their families with the best care and technology available. This focus has led to our recent acquisition of the EOSedge™, an imaging system that delivers high-quality, three-dimensional full-body images of patients in a standing position using low-dose radiation.
EOSedge has a unique setting called Flex DoseTM that adjusts the amount of radiation patients receive. This setting minimizes exposure of areas of the body when possible, while still delivering the high- resolution images needed for our doctors to make treatment decisions. EOSedge is now available at Nicklaus Children’s Hospital’s main campus.
The Center for Spinal Disorders at Nicklaus Children's has been using EOS imaging systems for its pediatric spine patients since 2013.
Patient Stories
Post-Anesthesia Care Unit (PACU)
What is the PACU?
PACU (which stands for Post- Anesthesia Care Unit) is also called the recovery room. It is a specialized care unit near the operating room where patients who have had surgery are cared for as they wake up from anesthesia. In the pediatric recovery room, a nurse will be at your child's bedside for the entire recovery period to ensure his/ her safety and comfort.
You may be invited into pediatric post-anesthesia care unit to be with your child as they wake up from their surgical procedure. Please understand that your ability to visit your child in the PACU depends on the activity and patient load of the unit at the time.
If you are asked to enter the PACU, you will be escorted in and out of the recovery room area either by a hospital employee or volunteer.
When you enter the PACU, you may see that there are several patients in the PACU in different stages of recovery post-anesthesia. We ask you to respect the privacy and confidentiality of all our patients and families by staying at your child's bedside. We also ask that you avoid the use of cell phones and cameras.
Before you enter the PACU, staff will first be sure that:
- No child's safety or privacy will be affected
- Your child is breathing well and has regained the ability to cough
Before you enter the PACU, you must first be sure that:
- You feel comfortable in a medical setting – you do not have to go into the post-anesthesia care unit if you are not comfortable in a medical setting
- You can provide a calm, supportive presence for your child
- You are willing to follow all directions from staff. If we cannot answer your questions or explain a situation fully at the moment you inquire, we will be sure to attend to your concerns as soon as we can.
For a patient's safety, yours or someone else's, you may be asked to leave PACU and return to the family waiting area.
What you'll see in pediatric post-anesthesia care unit
- Most children receive oxygen for a period of time after anesthesia. Sometimes children look pale, puffy or swollen after surgery. This is normal.
- Children differ in their reactions to anesthesia. Some have an upset stomach and may vomit. Often children are given medications to help decrease the possibility of nausea and vomiting. Some may have dizziness and/or blurred vision for a period of time.
- If a breathing tube is used during surgery your child may have a sore throat. This is normal.
- Children wake up differently from anesthesia. Some children wake up quickly and may be awake before their families arrive at their bedside. Other children may still be sleeping from the effects of anesthesia.
- Please do not wake your child. In our experience, children often have a gentler and more comfortable wake-up process when they do so on their own.
- Some children wake up shivering even if they are not cold. Your child will receive warmed blankets by the post-anesthesia care unit staff if needed.
- Some children who have had intravenous (IV) pain medication may have an extremely itchy nose. This itch will go away.
- Some children wake up restless or irritable. Some appear awake but are not aware of what is going on around them.
- Emergence Delirium: Some cry, thrash, arch their back, reach out and seem inconsolable, even when they are in their parents' arms. This behavior is not usually related to pain, and children do not usually remember it. This restless or irritable behavior is known as "emergence delirium". About one third of young children who have brief procedures experience emergence delirium. It may occur in children of any age, even after procedures that require a longer time under anesthesia. Emergence delirium may be upsetting for parents to see, but be assured that it will go away. Sometimes it lasts about 10 minutes; other times it may last up to an hour or longer.
- By staying calm and speaking softly, you can be a comfort to your child.
- Pain medicine is given as needed. After receiving pain medicine, children need to be observed due to the sleepiness and possible changes in breathing caused by most pain medications.
- If your child takes a comfort item along to surgery – such as a toy or special blanket – it will be with him or her in the PACU. If he is comforted by a pacifier, and it is sent with him to surgery, he will be given the pacifier in PACU (unless contraindicated by the type of surgery he or she has had).
How long will my child be in the PACU?
Because each child and each surgery are different, the length of time spent in the post-anesthesia care unit varies from a few minutes to more than 2 hours. Do not be alarmed if your child is in PACU longer than you expected. A staff member or volunteer will keep you informed.
Children leave PACU when:
- They respond to their surroundings.
- They are medically stable.
- Our staff has treated any pain they may have to the best of our ability.
Where will my child go next?
Once your child is fully recovered, and his/her vital signs are stable, he/she will be moved from the PACU. If your child requires hospital admission, he/she will be moved to a regular patient room. If he/she will be coming home with you, he'll/she'll be moved to PACU II for a minimum of a one hour stay prior to going home.
Post-Anesthesia Care Unit (PACU)
What is the PACU?
PACU (which stands for Post- Anesthesia Care Unit) is also called the recovery room. It is a specialized care unit near the operating room where patients who have had surgery are cared for as they wake up from anesthesia. In the pediatric recovery room, a nurse will be at your child's bedside for the entire recovery period to ensure his/ her safety and comfort.
You may be invited into pediatric post-anesthesia care unit to be with your child as they wake up from their surgical procedure. Please understand that your ability to visit your child in the PACU depends on the activity and patient load of the unit at the time.
If you are asked to enter the PACU, you will be escorted in and out of the recovery room area either by a hospital employee or volunteer.
When you enter the PACU, you may see that there are several patients in the PACU in different stages of recovery post-anesthesia. We ask you to respect the privacy and confidentiality of all our patients and families by staying at your child's bedside. We also ask that you avoid the use of cell phones and cameras.
Before you enter the PACU, staff will first be sure that:
- No child's safety or privacy will be affected
- Your child is breathing well and has regained the ability to cough
Before you enter the PACU, you must first be sure that:
- You feel comfortable in a medical setting – you do not have to go into the post-anesthesia care unit if you are not comfortable in a medical setting
- You can provide a calm, supportive presence for your child
- You are willing to follow all directions from staff. If we cannot answer your questions or explain a situation fully at the moment you inquire, we will be sure to attend to your concerns as soon as we can.
For a patient's safety, yours or someone else's, you may be asked to leave PACU and return to the family waiting area.
What you'll see in pediatric post-anesthesia care unit
- Most children receive oxygen for a period of time after anesthesia. Sometimes children look pale, puffy or swollen after surgery. This is normal.
- Children differ in their reactions to anesthesia. Some have an upset stomach and may vomit. Often children are given medications to help decrease the possibility of nausea and vomiting. Some may have dizziness and/or blurred vision for a period of time.
- If a breathing tube is used during surgery your child may have a sore throat. This is normal.
- Children wake up differently from anesthesia. Some children wake up quickly and may be awake before their families arrive at their bedside. Other children may still be sleeping from the effects of anesthesia.
- Please do not wake your child. In our experience, children often have a gentler and more comfortable wake-up process when they do so on their own.
- Some children wake up shivering even if they are not cold. Your child will receive warmed blankets by the post-anesthesia care unit staff if needed.
- Some children who have had intravenous (IV) pain medication may have an extremely itchy nose. This itch will go away.
- Some children wake up restless or irritable. Some appear awake but are not aware of what is going on around them.
- Emergence Delirium: Some cry, thrash, arch their back, reach out and seem inconsolable, even when they are in their parents' arms. This behavior is not usually related to pain, and children do not usually remember it. This restless or irritable behavior is known as "emergence delirium". About one third of young children who have brief procedures experience emergence delirium. It may occur in children of any age, even after procedures that require a longer time under anesthesia. Emergence delirium may be upsetting for parents to see, but be assured that it will go away. Sometimes it lasts about 10 minutes; other times it may last up to an hour or longer.
- By staying calm and speaking softly, you can be a comfort to your child.
- Pain medicine is given as needed. After receiving pain medicine, children need to be observed due to the sleepiness and possible changes in breathing caused by most pain medications.
- If your child takes a comfort item along to surgery – such as a toy or special blanket – it will be with him or her in the PACU. If he is comforted by a pacifier, and it is sent with him to surgery, he will be given the pacifier in PACU (unless contraindicated by the type of surgery he or she has had).
How long will my child be in the PACU?
Because each child and each surgery are different, the length of time spent in the post-anesthesia care unit varies from a few minutes to more than 2 hours. Do not be alarmed if your child is in PACU longer than you expected. A staff member or volunteer will keep you informed.
Children leave PACU when:
- They respond to their surroundings.
- They are medically stable.
- Our staff has treated any pain they may have to the best of our ability.
Where will my child go next?
Once your child is fully recovered, and his/her vital signs are stable, he/she will be moved from the PACU. If your child requires hospital admission, he/she will be moved to a regular patient room. If he/she will be coming home with you, he'll/she'll be moved to PACU II for a minimum of a one hour stay prior to going home.
Asthma Center
Cystic Fibrosis Center
The Cystic Fibrosis Center at Nicklaus Children’s Hospital offers comprehensive family-centered care for children and adults with cystic fibrosis. Since 1993, the program has been awarded affiliate program accreditation status from the Cystic Fibrosis Foundation, ensuring access to the most current treatments and research findings.
The program serves as a referral center for cystic fibrosis patients identified by the state of Florida’s Newborn Screening Program. The center is equipped to provide prompt interventions with specialized therapies to provide newly diagnosed patients with immediate treatment, in order to prevent complications and promote health.
Conditions we Treat
- Genetic testing
- Routine blood work
A Comprehensive Approach to Care
The program includes a comprehensive care team including:
- Pulmonologist
- Gastroenterologist
- Endocrinologist
- Cystic fibrosis coordinator
- Nurse practitioner
- Dietitian
- Respiratory therapist
- Social worker
- Psychologist
Programs and Services
The program includes comprehensive services, including:
- Outpatient care clinics
- Family education to support care
- Inpatient care
Education to Support Care
The Cystic Fibrosis Foundation assists patients and their families with education, disease management and supportive care.
Medical Research
The program participates in research protocols to advance care and understanding of cystic fibrosis.
Pulmonary Function Tests
When your patients require cardiopulmonary function tests, Nicklaus Children's Hospital, the region’s pediatric care leader – offers a comprehensive array of tests geared for children ages 5 and up. The tests are administered in the hospital’s new state-of-the art Pediatric Pulmonary Function Lab.
You’ll be confident knowing that pulmonary function tests are performed and interpreted by experts specially trained and highly experienced in testing and evaluating children.
Hard-to-Diagnose Asthma Patients
The Nicklaus Children's Hospital Cardiopulmonary Function Lab offers three specialized Bronchial Challenge Tests to confirm the presence or absence of bronchial hyperactivity in children. Bronchial Challenge Testing is indicated for the diagnosis of bronchial airway hyperactivity in subjects who do not have clinically apparent asthma. Bronchial challenge testing is an objective means to help you establish a diagnosis of asthma. A negative Bronchial Challenge Test result can rule out asthma as a potential etiology with a high degree of accuracy. By ruling out asthma as a causative factor in patient presentation, practitioners can work up an alternative diagnosis and avoid unnecessary medications or costs for patients.
Bronchial Challenge Tests
- Exercise Challenge Test: Utilizes a treadmill or ergometer. For those pediatric patients who are incapable or unwilling to sustain exercise long enough for reliable test results the Nicklaus Children's Hospital Cardiopulmonary Function Lab offers two additional widely supported reliable methods.
- Cold Air Challenge
- Methacholine Challenge Test
Cardiopulmonary Exercise Testing
The Nicklaus Children's Hospital Cardiopulmonary Lab offers pediatric cardiopulmonary exercise testing that can be used to evaluate:
- Cardiopulmonary performance in preoperative or postoperative congenital heart defects
- Functional capacity for vocational, recreational, armed forces, and athletic recommendations
- Specific symptoms or signs induced by exercise including palpitations, syncope, or possible arrhythmias
- Cardiomyopathies and overall fitness levels
- Suspected pulmonary disorders such as exercise-induced bronchospasm
Unlike most medical tests, which are performed on resting subjects, cardiopulmonary exercise testing can assess the functional capacity of the individual and can provide a more complete understanding of the patient’s physical abilities and limitations.
Additional Pulmonary Function Tests
Other tests offered through the Pulmonary Function Lab include:
- Spirometry and pre- and postbronchodilator testing to quantify the severity of known lung disease and/or assess the change in lung function over time or following a change in therapy. The test is also used to assess the potential effects of environmental or occupational exposure.
- Lung Volume Studies (Body Plethysmography or Helium Dilution) to assist doctors in differentiating between obstructive and restrictive disease patterns and assess response to therapeutic interventions (transplantation, radiation, chemotherapy, lobectomy). The study also supports physicians in making preoperative assessments in patients with impaired lung function and in quantifying the amount of non-ventilated lung.
- Carbon Monoxide Diffusing Capacity (DLCO) testing to differentiate among chronic bronchitis, emphysema, and asthma in patients with obstructive patterns. The test also supports physicians in predicting arterial desaturation during exercise in obstructive pulmonary disease and in evaluation and follow-up of interstitial lung disease and parenchymal lung diseases associated with dust (eg, asbestos) or drug reactions.
Patient Stories
Patient Stories
Related Web Links
Related informational web links:
*Links available in this page are not necessarily endorsed, reviewed, or sponsored by Nicklaus Children's Hospital.
Hot Topics for Parents
Educational resources for parents to talk with their children.
Preparing for Your Child’s Psychiatric Hospitalization
Parents have varied reactions to the experience of having a child hospitalized for depression or other behavioral health illnesses. Some parents become anxious upon learning that their child will be hospitalized, while others find it a relief that their child is getting help for his/her symptoms. We hope this guide will help in managing the experience. Our goal is to help you and your child through this transition to treatment and beyond.
Our interdisciplinary team provides evaluation and interventions for a broad spectrum of child and adolescent mental health conditions. The care of all patients admitted to the psychiatric unit is guided by a comprehensive, interdisciplinary treatment approach based on the bio/psycho/social model, which offers a holistic approach to evaluation and treatment.
The Hagerty Family Behavioral Health Unit embraces a family-centered approach to care. This means that you are an essential part of the team and will be involved in care decision making.
For the safety of patients, psychiatry is a secured unit with restricted access. The department features an acute stabilization program and the average inpatient stay is three to five days, although some patients may require a longer hospitalization to address individual needs. During your child’s stay the focus of treatment will include individual, group and family therapy, crisis intervention, on-going psychiatric/psychological evaluation, stabilization, and discharge planning.
Protecting your child’s safety and confidentiality is a priority for us. Due to the therapeutic structure of psychiatry, we do not offer open visiting hours/telephone calls, or parents staying on the unit.
Admission and Visiting Hours
On admission you will meet the assigned nurse and behavioral health technician who will provide you with in-patient information, including guidelines and policies for the unit. You will be asked to provide information regarding your child and sign consent forms. A family therapy session will also be scheduled on admission.
Within 24 hours of admission the attending psychiatrist, psychiatric fellow/resident, nurse practitioner, and a therapist will evaluate your child and contact you.
If you have special needs due to your work schedule, please inform your case coordinator or charge nurse so we may best accommodate your request. Visitors are limited to two at a time. Visiting minors need to be escorted by an adult while in the Hagerty Family Behavioral Health Unit. All visits are supervised by staff members.
The Treatment Plan
Your child will be seen by the treatment team every day to review his/her progress. The team can be available to answer any questions you may have. The team meets on an on-going basis throughout the week to discuss your child’s progress, including group participation, medication, and discharge planning.
Security and Personal Safety
For unit safety and the protection of patient confidentiality, a Personal Patient Identification Code (PPIC) will be given to you at the time of admission. Please remember that this number is necessary when asking for information or contact with the patient. This number is intended for guardians and immediate family.
All patients are under the close observation by a staff member 24 hours a day. Special precautions exist to provide a higher level of care for certain patients.
Hagerty Family Behavioral Health Unit Guidelines:
- Before entering the unit, family and visitors are required to obtain an identification tag from security. We ask all family members/visitors to leave personal belongings including cell phones in the lockers assigned by staff before entering the unit.
- For the safety of your child and the unit environment, all personal baggage is examined before entering the unit. Any belongings that are inappropriate will be given to the guardian to take home or will be kept in a locker. No sharp items are allowed on the unit.
- To help keep your child and the unit safe, acts of violence, and verbal or physical abuse are not allowed. All psychiatric staff is trained in crisis prevention interventions.
- Please leave any valuable items at home.
- Telephone calls can be made between the hours of noon to 1 pm, 5 p.m. – 7 p.m. and 8 p.m. – 9 p.m. as per unit protocol. Patients can only call individuals approved by the legal guardian. Parents are always welcome to call the unit to speak to the nurses or staff members if they have questions.
Frequently Asked Questions
Q: How long will my child need to be hospitalized?
A: Length of stay varies depending on the progress of the patient and family. The case coordinator will keep you informed regarding changes in your child’s length of stay.
Q: Will my child be safe on the unit?
A: All patients are closely supervised 24 hours a day and are frequently assessed for the need for higher levels of supervision.
Q: Can I stay with my child?
A: Due to safety, confidentiality, and space we are not able to have parents stay with their child on the unit.
Q: How do I get in touch with my child?
A: Patients do not have telephones in their rooms. Patients can make one phone call a day.
Staff monitors all calls. In order to protect confidentiality, parents will have a personal patient identification number to utilize when calling to talk to their child or check on their status. Parents should feel comfortable calling our unit at any time to share concerns.
Q: Will my child be talking to or visiting with his/her friends while in the hospital?
A: To maintain confidentiality and encourage families to work on treatment goals, we encourage phone calls and visits to be with patient and legal guardians/immediate family members.
Q: Will my child automatically receive medications during his/her hospitalization?
A: Any medications prescribed by the psychiatrist would only be recommended after an evaluation. Medication is often needed for the effective treatment and stabilization of psychiatric conditions. You as a parent/guardian are a part of the team and the psychiatrist and/or nurse will call you to obtain consent for medications. It is your legal right to be involved in all decisions regarding psychiatric medications and treatment while your child is under our care. Parents need to sign or give a witnessed verbal consent before the medication is given to a patient.
Q: What will my child’s typical day be like?
A: A typical day will include psychiatric medical rounds, various groups and activities, including individual therapy/family therapy, and group therapy. Patients may also participate in recreational entertainment at the Michael Fux Family Center under the supervision of the behavioral health techs.
Q: What behavioral intervention will be used with my child?
A: Staff uses a collaborative problem solving approach when dealing with patients. This focuses on children and adults working together to develop mutually satisfactory solutions to problems.
Q: Do parents/guardian need to attend therapy during the hospitalization?
A: Family therapy sessions are an integral part of the program. It is vital for family members to participate in these sessions as part of their child’s treatment. In-patient psychiatry stresses a family approach towards the setting and attainment of goals. These family sessions are also used to determine the patient’s readiness for discharge and ability to communicate effectively with the family members.
Q: What happens if my child has a medical problem during the hospital stay in the psychiatry unit?
A: The psychiatrist , nurse practitioner, or medical doctor will assess your child’s medical status through the use of nursing assessments, history and physical exam, lab work (including urine screen and blood screen), and other medical tests as deemed necessary. Results will be discussed with parents. If your child needs serious medical attention, he/she will be admitted to the medical floor.
Q: What if I have any concerns regarding my child’s treatment?
A: Please feel free to contact the team for any concerns. You may contact the unit manager if necessary at 305-666-6511 ext. 1075.
Health Promotion & Education
Sports Medicine
Because children and teens are still growing and developing, they experience different types of sports-related injuries than adults. The Nicklaus Children's Hospital, Pediatric Sports Medicine Program is dedicated to preventing and treating sports injuries in the growing athlete, or young sports enthusiast.
Our interdisciplinary orthopedic sports medicine specialists at three Nicklaus Children's locations work together to provide the most advanced care in orthopedic sports medicine for their patient by incorporating an array of diagnostic and therapeutic services such as X-ray, MRI, occupational and physical therapy to the treatment plan as needed.
Patient Stories
Fracture & Trauma Care
Hip Program
The Orthopedic, Sports Health and Spine Institute at Nicklaus Children’s Hospital provides evaluation and treatment of a full spectrum of hip disorders in children, adolescents and young adults. These disorders include a variety of congenital, developmental and post-traumatic conditions. Treatment methods include open and arthroscopic surgical techniques such as hip surgery. Our evaluation process combines a detailed clinical examination with state-of-the-art radiographic imaging.
Pediatric Hip Conditions we Treat
Pediatric Hip Disorder Treatment
- Surgical dislocation of the hip
- Closed and open reduction of developmental hip dislocations
- Other pelvic and femoral osteotomies
Hip imaging
The
Hip Program at Nicklaus Children’s is supported by a staff of fellowship-trained pediatric radiologists that utilize the latest imaging equipment and techniques. Our imaging capabilities include:
Patient Stories
Patient Stories
Testings and Diagnostics
MRI
- Magnet Resonance Imaging (MRI) uses a large magnet and radio waves to produce a picture of a body structure. Your child will be able to watch a movie, listen to the radio or play a favorite CD wile the scan is being performed. Learn more.
PillCam
- Camera pill, a non-invasive capsule endoscopy.
Patient Stories
Meet the Craniofacial Team
The members of the Craniofacial team work together to develop and deliver a coordinated plan of care to meet each child’s individual needs. The multidisciplinary team is comprised of specialists in the following disciplines:
Conditions we Treat
Patient Stories
Prenatal Clinic for Craniofacial Anomalies
Enhancements in prenatal ultrasound imaging technology have resulted in increasing numbers of families learning that their baby has a craniofacial difference before his or her birth. That knowledge can bring anxiety and many questions. Expectant parents often ask:
- What is the anomaly?
- What caused it?
- What is the prognosis for the baby?
- Can it be repaired?
- How do I take care of my baby?
To address the questions and concerns of expectant parents in a comprehensive way, the Nicklaus Children's Hospital Craniofacial Center has created a Prenatal Clinic in which families are evaluated by a team of specialists including nurses, plastic and reconstructive surgeons, and geneticists.
Families are provided information on the causes of craniofacial differences and what to expect when the baby is born. They are shown photographs of children before and after repair of craniofacial differences, and are given necessary contact information and supplies when the baby is born.
With this information, families feel more prepared for the birth of their baby. Further, the families leave knowing where to find support, which helps decrease anxiety and promotes a more enjoyable pregnancy and birth experience.
Care for a Full Spectrum of Craniofacial Anomalies
The Craniofacial Center at Nicklaus Children's Hospital, serves children with various craniofacial differences such as:
- Cleft lip and palate
- Pierre Robin sequence
- Hemifacial microsomia
- Treacher Collins
- Craniosynostosis
The Craniofacial Center conducts a multidisciplinary evaluation for affected children, and develops and coordinates a plan of care.
Prenatal Clinic for Craniofacial Anomalies
Enhancements in prenatal ultrasound imaging technology have resulted in increasing numbers of families learning that their baby has a craniofacial difference before his or her birth. That knowledge can bring anxiety and many questions. Expectant parents often ask:
- What is the anomaly?
- What caused it?
- What is the prognosis for the baby?
- Can it be repaired?
- How do I take care of my baby?
To address the questions and concerns of expectant parents in a comprehensive way, the Nicklaus Children's Hospital Craniofacial Center has created a Prenatal Clinic in which families are evaluated by a team of specialists including nurses, plastic and reconstructive surgeons, and geneticists.
Families are provided information on the causes of craniofacial differences and what to expect when the baby is born. They are shown photographs of children before and after repair of craniofacial differences, and are given necessary contact information and supplies when the baby is born.
With this information, families feel more prepared for the birth of their baby. Further, the families leave knowing where to find support, which helps decrease anxiety and promotes a more enjoyable pregnancy and birth experience.
Care for a Full Spectrum of Craniofacial Anomalies
The Craniofacial Center at Nicklaus Children's Hospital, serves children with various craniofacial differences such as:
- Cleft lip and palate
- Pierre Robin sequence
- Hemifacial microsomia
- Treacher Collins
- Craniosynostosis
The Craniofacial Center conducts a multidisciplinary evaluation for affected children, and develops and coordinates a plan of care.
Additional Resources
Spinal Fusion Surgery
What is Spinal Fusion Surgery in Children?
Spinal fusion surgery helps to stop the progression of curving of the spine, known as scoliosis. The surgery helps to not only straighten the curve, but can improve children’s posture, fit of clothing, prevent back pain, and minimize other side effects of scoliosis.
The spinal fusion recovery process can be difficult, as children may experience pain and find it hard to sit up, stand, and walk while recovering. Nicklaus Children's Hospital, formerly Miami Children's Hospital, is here to help your child have a smooth recovery from spinal fusion surgery and answer any questions throughout the process.
Pediatric Spinal Fusion Surgery Program at Nicklaus Children's
Is spinal fusion surgery in your future? If so, you are probably feeling some uncertainty. The best thing you can do right now is to learn as much as possible about the procedure and share the information with friends and family. Knowledge will prepare you for what is ahead and help you feel more in control and less anxious. Here’s how to get started. First, ask your doctor every question that comes to mind and read all the materials you can find on the subject. We also urge you to attend the Spinal Fusion Program at Nicklaus Children's Hospital. The Spinal Fusion Program provides an opportunity for you and your family to learn about what to expect during spinal fusion recovery.
Read our guides for Spinal Fusion Surgery
Spinal Fusion Surgery
What is Spinal Fusion Surgery in Children?
Spinal fusion surgery helps to stop the progression of curving of the spine, known as scoliosis. The surgery helps to not only straighten the curve, but can improve children’s posture, fit of clothing, prevent back pain, and minimize other side effects of scoliosis.
The spinal fusion recovery process can be difficult, as children may experience pain and find it hard to sit up, stand, and walk while recovering. Nicklaus Children's Hospital, formerly Miami Children's Hospital, is here to help your child have a smooth recovery from spinal fusion surgery and answer any questions throughout the process.
Pediatric Spinal Fusion Surgery Program at Nicklaus Children's
Is spinal fusion surgery in your future? If so, you are probably feeling some uncertainty. The best thing you can do right now is to learn as much as possible about the procedure and share the information with friends and family. Knowledge will prepare you for what is ahead and help you feel more in control and less anxious. Here’s how to get started. First, ask your doctor every question that comes to mind and read all the materials you can find on the subject. We also urge you to attend the Spinal Fusion Program at Nicklaus Children's Hospital. The Spinal Fusion Program provides an opportunity for you and your family to learn about what to expect during spinal fusion recovery.
Read our guides for Spinal Fusion Surgery
ILIZAROV Technique
Your orthopedic surgeon has chosen to use the ILIZAROV (Ill-is-are-off) method of limb correction. The ILIZAROV treatment is a highly successful orthopedic surgical technique designed to lengthen or straighten bone and soft tissue. Additionally, the ILIZAROV technique and the innovative device can sometimes save limbs that might otherwise be amputated.
Although some form of fixation has been used in orthopedic medicine for hundreds of years, it was Russian-born Gavril Ilizarov who is considered the 'father' of circular external fixators and the ILIZAROV technique. In fact, all circular external fixators today are based on Dr. Ilizarov's work from the 1950s.
Taking advantage of the remarkable fact that bone heals itself by growing, or regenerating, the ILIZAROV technique can correct disfigured bones by separating two bone halves millimeter by millimeter. During this process, the body's natural ability to grow bone fills in the gap between the two bones, correcting deformities or increasing length.

Use of the ILIZAROV Method
Limb length inequality and limb deformity can be due to many causes. The treatment plan and use of the ILIZAROV method will depend on the degree of the discrepancy, the age of the patient, and the underlying reason for the deformity.
Limb correction and ILIZAROV treatment may be prescribed for a variety of conditions:
Trauma, including:
- Growth plate fractures
- Malunion (healing of bones in an incorrect position)
- Nonunion (incomplete healing of fractured bones)
- Shortening and deformity due to bone loss
Congenital limb length discrepancies, including:
- Congenital short Femur
- Fibular hemimelia
- Pseudarthrosis of the Tibia
- Hemiatrophy/Hemihypertrophy
- and other birth defects and deformities
Pediatric hip disorders
- Developmental Coxa Cara
- Perthes Disease
- Slipped Capital Femoral Epiphyses (SCFE)
Other conditions
- Joint stiffness secondary to neuromuscular disease or following injury
- Bow legs
- Knock-knees
- Short stature (achondroplasia and other skeletal dysplasias)
- Infection involving the bone (osteomyelitis) and joint (septic arthritis)
◊ Trademark of Smith & NephewILIZAROV Technique
Your orthopedic surgeon has chosen to use the ILIZAROV (Ill-is-are-off) method of limb correction. The ILIZAROV treatment is a highly successful orthopedic surgical technique designed to lengthen or straighten bone and soft tissue. Additionally, the ILIZAROV technique and the innovative device can sometimes save limbs that might otherwise be amputated.
Although some form of fixation has been used in orthopedic medicine for hundreds of years, it was Russian-born Gavril Ilizarov who is considered the 'father' of circular external fixators and the ILIZAROV technique. In fact, all circular external fixators today are based on Dr. Ilizarov's work from the 1950s.
Taking advantage of the remarkable fact that bone heals itself by growing, or regenerating, the ILIZAROV technique can correct disfigured bones by separating two bone halves millimeter by millimeter. During this process, the body's natural ability to grow bone fills in the gap between the two bones, correcting deformities or increasing length.

Use of the ILIZAROV Method
Limb length inequality and limb deformity can be due to many causes. The treatment plan and use of the ILIZAROV method will depend on the degree of the discrepancy, the age of the patient, and the underlying reason for the deformity.
Limb correction and ILIZAROV treatment may be prescribed for a variety of conditions:
Trauma, including:
- Growth plate fractures
- Malunion (healing of bones in an incorrect position)
- Nonunion (incomplete healing of fractured bones)
- Shortening and deformity due to bone loss
Congenital limb length discrepancies, including:
- Congenital short Femur
- Fibular hemimelia
- Pseudarthrosis of the Tibia
- Hemiatrophy/Hemihypertrophy
- and other birth defects and deformities
Pediatric hip disorders
- Developmental Coxa Cara
- Perthes Disease
- Slipped Capital Femoral Epiphyses (SCFE)
Other conditions
- Joint stiffness secondary to neuromuscular disease or following injury
- Bow legs
- Knock-knees
- Short stature (achondroplasia and other skeletal dysplasias)
- Infection involving the bone (osteomyelitis) and joint (septic arthritis)
◊ Trademark of Smith & NephewWhat to Do After Surgery
Each surgery is different and will require different care at home but we have put the more common questions together regarding recovery from surgery.
What should I do about pain?
After surgery, a prescription for pain medicine is given. Tylenol is usually sufficient to make your child comfortable during recovery from surgery. In case of excessive pain, please contact the surgeon's office.
What should I do with the wound?
In the absence of specific instructions for care after surgery, most surgical wounds in children take care of themselves. All you have to do is try to keep them clean and dry for the first week, after which you may resume bathing. Pediatric surgeons try as hard as possible to use only absorbable sutures so that there are usually no sutures to remove.
When should I call the surgeon?
Call the surgeon whenever you are in doubt or have a question about your child's recovery from surgery. But some things must bring you back for a visit. Call and return to visit your surgeon, if you see:
What can my child eat?
Unless specifically addressed, your child can return to a regular diet as soon as he/she wishes to after surgery.
Applications and Uses of fMRI
Presurgical Planning
 Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
In the left image there is a little cyst in the left hemisphere (seen at the right side of the brain as a round black shape). This lesion produced seizures. The surgeon needs to know the location of the cortex in charge of the movement of the hand. This fMRI shows in colors the area used for the movement of the right fingers in a tapping task. This enables the neurosurgeon to extract the lesion without removing the area needed to move the hand.
Language Mapping
Brain functions can be divided into basic and complex. Basic functions require few areas of the cortex, while complex functions could be spread over one hemisphere, or even in both. Basic brain functions are consistently represented in the same places across different people, while the complex functions tend to vary from person to person. Language is a typical complex function. In most people, language is represented in the left hemisphere, but it is completely normal to find representation in the right hemisphere or divided between them. Prior to brain surgery, it is quite important to know the side in which the language is represented.
In epilepsy surgery this has a crucial importance. Some times it is necessary to remove part of the temporal lobe involved in the generation of seizures. The extension of the surgery must be restricted if it is found that this lobe is involved in language processing.
Here at Nicklaus Children's Hospital we have started to perform Language Mapping with fMRI to assess the localization of language, in adults and children over 7 years old.
Non-Surgical Applications
 fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
These images are from a 2 year-old child. They are named coronal cuts. The head is seen on top and the neck is on the bottom. Inside you see the two hemishpheres of the brain, and below them the cerebellum. The patient was sedated for a regular procedure. Flashing lights were presented during 3 minutes. The visual cortex, located in the occipital lobes, is depicted in red and yellow colors.
Images of activation in sedated kids have been obtained by presenting sounds (such as the mother's voice), or tactile stimulation to the skin (such as rubbing the hand).
On of the future purposes of fMRI is to predict developmental disorders at very young ages in order to provide effective early treatment interventions.
Applications and Uses of fMRI
Presurgical Planning
 Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
In the left image there is a little cyst in the left hemisphere (seen at the right side of the brain as a round black shape). This lesion produced seizures. The surgeon needs to know the location of the cortex in charge of the movement of the hand. This fMRI shows in colors the area used for the movement of the right fingers in a tapping task. This enables the neurosurgeon to extract the lesion without removing the area needed to move the hand.
Language Mapping
Brain functions can be divided into basic and complex. Basic functions require few areas of the cortex, while complex functions could be spread over one hemisphere, or even in both. Basic brain functions are consistently represented in the same places across different people, while the complex functions tend to vary from person to person. Language is a typical complex function. In most people, language is represented in the left hemisphere, but it is completely normal to find representation in the right hemisphere or divided between them. Prior to brain surgery, it is quite important to know the side in which the language is represented.
In epilepsy surgery this has a crucial importance. Some times it is necessary to remove part of the temporal lobe involved in the generation of seizures. The extension of the surgery must be restricted if it is found that this lobe is involved in language processing.
Here at Nicklaus Children's Hospital we have started to perform Language Mapping with fMRI to assess the localization of language, in adults and children over 7 years old.
Non-Surgical Applications
 fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
These images are from a 2 year-old child. They are named coronal cuts. The head is seen on top and the neck is on the bottom. Inside you see the two hemishpheres of the brain, and below them the cerebellum. The patient was sedated for a regular procedure. Flashing lights were presented during 3 minutes. The visual cortex, located in the occipital lobes, is depicted in red and yellow colors.
Images of activation in sedated kids have been obtained by presenting sounds (such as the mother's voice), or tactile stimulation to the skin (such as rubbing the hand).
On of the future purposes of fMRI is to predict developmental disorders at very young ages in order to provide effective early treatment interventions.
Applications and Uses of fMRI
Presurgical Planning
 Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
In the left image there is a little cyst in the left hemisphere (seen at the right side of the brain as a round black shape). This lesion produced seizures. The surgeon needs to know the location of the cortex in charge of the movement of the hand. This fMRI shows in colors the area used for the movement of the right fingers in a tapping task. This enables the neurosurgeon to extract the lesion without removing the area needed to move the hand.
Language Mapping
Brain functions can be divided into basic and complex. Basic functions require few areas of the cortex, while complex functions could be spread over one hemisphere, or even in both. Basic brain functions are consistently represented in the same places across different people, while the complex functions tend to vary from person to person. Language is a typical complex function. In most people, language is represented in the left hemisphere, but it is completely normal to find representation in the right hemisphere or divided between them. Prior to brain surgery, it is quite important to know the side in which the language is represented.
In epilepsy surgery this has a crucial importance. Some times it is necessary to remove part of the temporal lobe involved in the generation of seizures. The extension of the surgery must be restricted if it is found that this lobe is involved in language processing.
Here at Nicklaus Children's Hospital we have started to perform Language Mapping with fMRI to assess the localization of language, in adults and children over 7 years old.
Non-Surgical Applications
 fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
These images are from a 2 year-old child. They are named coronal cuts. The head is seen on top and the neck is on the bottom. Inside you see the two hemishpheres of the brain, and below them the cerebellum. The patient was sedated for a regular procedure. Flashing lights were presented during 3 minutes. The visual cortex, located in the occipital lobes, is depicted in red and yellow colors.
Images of activation in sedated kids have been obtained by presenting sounds (such as the mother's voice), or tactile stimulation to the skin (such as rubbing the hand).
On of the future purposes of fMRI is to predict developmental disorders at very young ages in order to provide effective early treatment interventions.
Applications and Uses of fMRI
Presurgical Planning
 Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
In the left image there is a little cyst in the left hemisphere (seen at the right side of the brain as a round black shape). This lesion produced seizures. The surgeon needs to know the location of the cortex in charge of the movement of the hand. This fMRI shows in colors the area used for the movement of the right fingers in a tapping task. This enables the neurosurgeon to extract the lesion without removing the area needed to move the hand.
Language Mapping
Brain functions can be divided into basic and complex. Basic functions require few areas of the cortex, while complex functions could be spread over one hemisphere, or even in both. Basic brain functions are consistently represented in the same places across different people, while the complex functions tend to vary from person to person. Language is a typical complex function. In most people, language is represented in the left hemisphere, but it is completely normal to find representation in the right hemisphere or divided between them. Prior to brain surgery, it is quite important to know the side in which the language is represented.
In epilepsy surgery this has a crucial importance. Some times it is necessary to remove part of the temporal lobe involved in the generation of seizures. The extension of the surgery must be restricted if it is found that this lobe is involved in language processing.
Here at Nicklaus Children's Hospital we have started to perform Language Mapping with fMRI to assess the localization of language, in adults and children over 7 years old.
Non-Surgical Applications
 fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
These images are from a 2 year-old child. They are named coronal cuts. The head is seen on top and the neck is on the bottom. Inside you see the two hemishpheres of the brain, and below them the cerebellum. The patient was sedated for a regular procedure. Flashing lights were presented during 3 minutes. The visual cortex, located in the occipital lobes, is depicted in red and yellow colors.
Images of activation in sedated kids have been obtained by presenting sounds (such as the mother's voice), or tactile stimulation to the skin (such as rubbing the hand).
On of the future purposes of fMRI is to predict developmental disorders at very young ages in order to provide effective early treatment interventions.
Applications and Uses of fMRI
Presurgical Planning
 Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
Sometimes it is very important to know which brain functions are in the neighborhood of a lesion, particularly if that lesion is going to be removed by surgery. In lesions formed before birth, such as blood vessel abnormalities and some tumors, the areas of language and other mental process can be misplaced. fMRI shows the actual location of the functions and their spatial relationship with those lesions.
In the left image there is a little cyst in the left hemisphere (seen at the right side of the brain as a round black shape). This lesion produced seizures. The surgeon needs to know the location of the cortex in charge of the movement of the hand. This fMRI shows in colors the area used for the movement of the right fingers in a tapping task. This enables the neurosurgeon to extract the lesion without removing the area needed to move the hand.
Language Mapping
Brain functions can be divided into basic and complex. Basic functions require few areas of the cortex, while complex functions could be spread over one hemisphere, or even in both. Basic brain functions are consistently represented in the same places across different people, while the complex functions tend to vary from person to person. Language is a typical complex function. In most people, language is represented in the left hemisphere, but it is completely normal to find representation in the right hemisphere or divided between them. Prior to brain surgery, it is quite important to know the side in which the language is represented.
In epilepsy surgery this has a crucial importance. Some times it is necessary to remove part of the temporal lobe involved in the generation of seizures. The extension of the surgery must be restricted if it is found that this lobe is involved in language processing.
Here at Nicklaus Children's Hospital we have started to perform Language Mapping with fMRI to assess the localization of language, in adults and children over 7 years old.
Non-Surgical Applications
 fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
fMRI has a great potential to provide insight into neurologic and psychiatric disorders. fMRI has been used to assess childhood stroke, migraine and epilepsy. This procedure has also been applied to children with developmental disorders, including autism, dyslexia, and other learning disabilities. Currently we are conducting research in sedated children and infants. Our goal is to obtain activation of the brain regardless of the sedation.
These images are from a 2 year-old child. They are named coronal cuts. The head is seen on top and the neck is on the bottom. Inside you see the two hemishpheres of the brain, and below them the cerebellum. The patient was sedated for a regular procedure. Flashing lights were presented during 3 minutes. The visual cortex, located in the occipital lobes, is depicted in red and yellow colors.
Images of activation in sedated kids have been obtained by presenting sounds (such as the mother's voice), or tactile stimulation to the skin (such as rubbing the hand).
On of the future purposes of fMRI is to predict developmental disorders at very young ages in order to provide effective early treatment interventions.
How fMRI Works
In order to understand how functional magnetic resonance (fMRI) works it is important to know some basic things about brain anatomy and function. Also, it is necessary to know some magnetic resonance imaging (MRI) basic facts. Let's begin with the first part:
A very short course on Neuroanatomy
The brain is divided in two hemispheres, the right and the left. Each hemisphere is divided into lobes. And each lobe has different areas as is depicted in the next figure taken with permission from http://www.umich.edu/~cogneuro/home.html
 Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Areas 1,2,3, and 5 "feel" the sensations of touch, position and temperature. Areas 4, 6, and 8 move the muscles of the body. Areas like 44, 45 and 47 produce language. Areas 41 and 42 "hear", areas 17 to 19 "see".
Other areas like 37, 46, 10, 22, 38 are in charge of the complex process involving memory, internal language, comprehension and planning.
This is a regionalization of the function. Also, there is something called "lateralization" of the function. This means that a particular activity can be predominantly located in one hemisphere. That happens with language. In almost all right-handed people the left hemisphere is dominant for language.
Each thing we do, any thought, feeling or sensation is produced by the activity of cells localized in a specific area of the brain. For example, if you receive the credit card bill and you panic, that is because a group of cells in the inner part of the brain start to fire, increasing its electrical current, transmission, and metabolism. These cells need more blood since they need more fuel. And it happens that when an area of the brain becomes activated, that area receives more blood because in that region there is dilatation of the tiny blood vessels.
So, ultimately, any action of the brain occurs along with an increase of blood at the point of the cortex where that action is commanded.
Now, let's continue to the second part.
A very, very short course on MRI basics
MRI is a procedure to see the anatomy of the internal organs of the body. It is based on three things: magnetism, radiofrequency and computers.
Nevertheless, to understand how an MRI works and how these three things can show us the anatomy of the brain (and the whole body) it is important to know five other things:
- Our body contains large amounts of water.
- Water is formed by hydrogen and oxygen (The hydrogen is presented basically as protons).
- Protons are positive charges that spin.
- A charge that spins creates a magnetic field that can be oriented. In other words, these micro-magnets can be up or down, right or left.
- The spin of these micro-magnets have a specific frequency (or velocity).
And that is it. Let's return to the three things needed to perform an MRI: magnetism, radiofrequency and computers.
Magnetism
The magnetic resonance machine is a big and strong magnet. When the body is inside, every proton of the body is oriented in the same way (for instance, with the positive pole up). This means that the body becomes a magnet, but a non-homogeneous magnet, because the amount of water in each part of the body varies with the specific characteristics of the organ: the layer, the location, and even the types of cells. Therefore, the human body can be pictured as a 3D-map of changes of magnetic field with a human body form. If we knew the density of those changes we could obtain the images of the internal anatomy. And how do we know the density? By means of radiofrequency.
Radiofrequency
Radiofrequency gives energy to the spin of the protons, increasing the amplitude of their turns without changing the frequency. Now the 3D-magnetic map becomes a 3D-map of energy. Each particular point in the body has a particular energy (or intensity, in terms of radiofrequency). If radiofrequency is no longer applied to the body, the proton-spins return to their original state and in that moment release radiofrequency waves. Now we have a 3D-map of radiofrequency. And radiofrequency can be registered with coils.
Computers
The rest of the procedure is done by the computers that convert the signal intensity, the signal phase, and the signal location into a matrix of dots with different values. Each value is represented with a tone of gray. The minimum value is black, and the maximum value is white, and in between is a scale of gray. At this point WE HAVE THE MR IMAGE!
How the FMRI Works
In functional imaging we have two components: a task and a result. The task is an action or activity that the subject does in order to produce a particular activation of the brain. For example, moving the right hand fingers continuously is a motor task that "activates" the brain cortex in the left frontal lobe. The result in fMRI is an image which depicts this activation.
The task can be of any type. Motor, feeling a sensation, having a perception, thinking in abstract words, attending to a changing stimulus, listening to music, comprehending a story, and many others. The task will produce this sequence of events:
- Increases in metabolism of the brain area involved in the task
- Increases in volume of blood in that particular region
- Increases in oxygen level
- Changes in the local magnetic field (Do you remember the 3D-magnetic field map discussed earlier?)
- Changes in the intensity of the energy (radiofrequency) in the same area.
In brief, the task elicits activity of a region of the brain, and this activity changes the intensity of the radiofrequency coming from that part. This is a very small change. But, if we repeat the task several times we are able to sum the changes to get a significant result that can be registered.
We compare a person's brain activity during a particular task with their activity level during a resting state. However, the brain works continuously, even during the resting state. For that reason the resting state is a baseline of the background activity of the brain.
So we must know the value of the background signal activity and the value of the signal related to the task. To do this, hundreds of images of the region targeted are taken during a few minutes. Meanwhile, the subject is alternating between periods of activity (performing the task) and periods of rest. In this manner we have a group of images of a region taken during the task, and the same number of images of the same region during rest. Two averaged images are obtained corresponding to two conditions in which one is "activated".
As we have seen before, images are the result of the values of the signal intensity, encoded on a gray scale. These values can be added, subtracted, etc. Well, that is exactly the next step. Powerful computers subtract the baseline values from the activated ones. These values of activation are then transformed into a map of colors. Usually the scale of this map varies from blue to red in a increasing manner. Finally, the colors are overlaid upon anatomical images, in a similar way that the weather maps are overlaid upon geographical pictures.
How fMRI can be helpful in Medicine
fMRI has a particular terminology. The next images explain the must important terms used to describe one experiment.

One epoch is a period of time in which something is occurring.
- ON: The name of the epoch in which the task is performed
- OFF: The name of the epoch in which the subject is at rest
A scan is the image obtained in each unit of time
A level is the localization of the site to explore. Several levels can be explored at once.

In this graphic is shown: 5 epochs ON, in which the subject performs the task; 5 epochs OFF, in which the subject is at rest; each epoch lasts 30 seconds for a total length of the experiment of 5 minutes. Four levels of the brain are explored, with 120 images (or scans) divided in alternated groups of 12.
A Final Result

The areas in color depict the activation of the brain regions involved in hearing and comprehending the human voice. The left hemisphere shows greater activation.
How fMRI Works
In order to understand how functional magnetic resonance (fMRI) works it is important to know some basic things about brain anatomy and function. Also, it is necessary to know some magnetic resonance imaging (MRI) basic facts. Let's begin with the first part:
A very short course on Neuroanatomy
The brain is divided in two hemispheres, the right and the left. Each hemisphere is divided into lobes. And each lobe has different areas as is depicted in the next figure taken with permission from http://www.umich.edu/~cogneuro/home.html
 Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Areas 1,2,3, and 5 "feel" the sensations of touch, position and temperature. Areas 4, 6, and 8 move the muscles of the body. Areas like 44, 45 and 47 produce language. Areas 41 and 42 "hear", areas 17 to 19 "see".
Other areas like 37, 46, 10, 22, 38 are in charge of the complex process involving memory, internal language, comprehension and planning.
This is a regionalization of the function. Also, there is something called "lateralization" of the function. This means that a particular activity can be predominantly located in one hemisphere. That happens with language. In almost all right-handed people the left hemisphere is dominant for language.
Each thing we do, any thought, feeling or sensation is produced by the activity of cells localized in a specific area of the brain. For example, if you receive the credit card bill and you panic, that is because a group of cells in the inner part of the brain start to fire, increasing its electrical current, transmission, and metabolism. These cells need more blood since they need more fuel. And it happens that when an area of the brain becomes activated, that area receives more blood because in that region there is dilatation of the tiny blood vessels.
So, ultimately, any action of the brain occurs along with an increase of blood at the point of the cortex where that action is commanded.
Now, let's continue to the second part.
A very, very short course on MRI basics
MRI is a procedure to see the anatomy of the internal organs of the body. It is based on three things: magnetism, radiofrequency and computers.
Nevertheless, to understand how an MRI works and how these three things can show us the anatomy of the brain (and the whole body) it is important to know five other things:
- Our body contains large amounts of water.
- Water is formed by hydrogen and oxygen (The hydrogen is presented basically as protons).
- Protons are positive charges that spin.
- A charge that spins creates a magnetic field that can be oriented. In other words, these micro-magnets can be up or down, right or left.
- The spin of these micro-magnets have a specific frequency (or velocity).
And that is it. Let's return to the three things needed to perform an MRI: magnetism, radiofrequency and computers.
Magnetism
The magnetic resonance machine is a big and strong magnet. When the body is inside, every proton of the body is oriented in the same way (for instance, with the positive pole up). This means that the body becomes a magnet, but a non-homogeneous magnet, because the amount of water in each part of the body varies with the specific characteristics of the organ: the layer, the location, and even the types of cells. Therefore, the human body can be pictured as a 3D-map of changes of magnetic field with a human body form. If we knew the density of those changes we could obtain the images of the internal anatomy. And how do we know the density? By means of radiofrequency.
Radiofrequency
Radiofrequency gives energy to the spin of the protons, increasing the amplitude of their turns without changing the frequency. Now the 3D-magnetic map becomes a 3D-map of energy. Each particular point in the body has a particular energy (or intensity, in terms of radiofrequency). If radiofrequency is no longer applied to the body, the proton-spins return to their original state and in that moment release radiofrequency waves. Now we have a 3D-map of radiofrequency. And radiofrequency can be registered with coils.
Computers
The rest of the procedure is done by the computers that convert the signal intensity, the signal phase, and the signal location into a matrix of dots with different values. Each value is represented with a tone of gray. The minimum value is black, and the maximum value is white, and in between is a scale of gray. At this point WE HAVE THE MR IMAGE!
How the FMRI Works
In functional imaging we have two components: a task and a result. The task is an action or activity that the subject does in order to produce a particular activation of the brain. For example, moving the right hand fingers continuously is a motor task that "activates" the brain cortex in the left frontal lobe. The result in fMRI is an image which depicts this activation.
The task can be of any type. Motor, feeling a sensation, having a perception, thinking in abstract words, attending to a changing stimulus, listening to music, comprehending a story, and many others. The task will produce this sequence of events:
- Increases in metabolism of the brain area involved in the task
- Increases in volume of blood in that particular region
- Increases in oxygen level
- Changes in the local magnetic field (Do you remember the 3D-magnetic field map discussed earlier?)
- Changes in the intensity of the energy (radiofrequency) in the same area.
In brief, the task elicits activity of a region of the brain, and this activity changes the intensity of the radiofrequency coming from that part. This is a very small change. But, if we repeat the task several times we are able to sum the changes to get a significant result that can be registered.
We compare a person's brain activity during a particular task with their activity level during a resting state. However, the brain works continuously, even during the resting state. For that reason the resting state is a baseline of the background activity of the brain.
So we must know the value of the background signal activity and the value of the signal related to the task. To do this, hundreds of images of the region targeted are taken during a few minutes. Meanwhile, the subject is alternating between periods of activity (performing the task) and periods of rest. In this manner we have a group of images of a region taken during the task, and the same number of images of the same region during rest. Two averaged images are obtained corresponding to two conditions in which one is "activated".
As we have seen before, images are the result of the values of the signal intensity, encoded on a gray scale. These values can be added, subtracted, etc. Well, that is exactly the next step. Powerful computers subtract the baseline values from the activated ones. These values of activation are then transformed into a map of colors. Usually the scale of this map varies from blue to red in a increasing manner. Finally, the colors are overlaid upon anatomical images, in a similar way that the weather maps are overlaid upon geographical pictures.
How fMRI can be helpful in Medicine
fMRI has a particular terminology. The next images explain the must important terms used to describe one experiment.

One epoch is a period of time in which something is occurring.
- ON: The name of the epoch in which the task is performed
- OFF: The name of the epoch in which the subject is at rest
A scan is the image obtained in each unit of time
A level is the localization of the site to explore. Several levels can be explored at once.

In this graphic is shown: 5 epochs ON, in which the subject performs the task; 5 epochs OFF, in which the subject is at rest; each epoch lasts 30 seconds for a total length of the experiment of 5 minutes. Four levels of the brain are explored, with 120 images (or scans) divided in alternated groups of 12.
A Final Result

The areas in color depict the activation of the brain regions involved in hearing and comprehending the human voice. The left hemisphere shows greater activation.
How fMRI Works
In order to understand how functional magnetic resonance (fMRI) works it is important to know some basic things about brain anatomy and function. Also, it is necessary to know some magnetic resonance imaging (MRI) basic facts. Let's begin with the first part:
A very short course on Neuroanatomy
The brain is divided in two hemispheres, the right and the left. Each hemisphere is divided into lobes. And each lobe has different areas as is depicted in the next figure taken with permission from http://www.umich.edu/~cogneuro/home.html
 Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Areas 1,2,3, and 5 "feel" the sensations of touch, position and temperature. Areas 4, 6, and 8 move the muscles of the body. Areas like 44, 45 and 47 produce language. Areas 41 and 42 "hear", areas 17 to 19 "see".
Other areas like 37, 46, 10, 22, 38 are in charge of the complex process involving memory, internal language, comprehension and planning.
This is a regionalization of the function. Also, there is something called "lateralization" of the function. This means that a particular activity can be predominantly located in one hemisphere. That happens with language. In almost all right-handed people the left hemisphere is dominant for language.
Each thing we do, any thought, feeling or sensation is produced by the activity of cells localized in a specific area of the brain. For example, if you receive the credit card bill and you panic, that is because a group of cells in the inner part of the brain start to fire, increasing its electrical current, transmission, and metabolism. These cells need more blood since they need more fuel. And it happens that when an area of the brain becomes activated, that area receives more blood because in that region there is dilatation of the tiny blood vessels.
So, ultimately, any action of the brain occurs along with an increase of blood at the point of the cortex where that action is commanded.
Now, let's continue to the second part.
A very, very short course on MRI basics
MRI is a procedure to see the anatomy of the internal organs of the body. It is based on three things: magnetism, radiofrequency and computers.
Nevertheless, to understand how an MRI works and how these three things can show us the anatomy of the brain (and the whole body) it is important to know five other things:
- Our body contains large amounts of water.
- Water is formed by hydrogen and oxygen (The hydrogen is presented basically as protons).
- Protons are positive charges that spin.
- A charge that spins creates a magnetic field that can be oriented. In other words, these micro-magnets can be up or down, right or left.
- The spin of these micro-magnets have a specific frequency (or velocity).
And that is it. Let's return to the three things needed to perform an MRI: magnetism, radiofrequency and computers.
Magnetism
The magnetic resonance machine is a big and strong magnet. When the body is inside, every proton of the body is oriented in the same way (for instance, with the positive pole up). This means that the body becomes a magnet, but a non-homogeneous magnet, because the amount of water in each part of the body varies with the specific characteristics of the organ: the layer, the location, and even the types of cells. Therefore, the human body can be pictured as a 3D-map of changes of magnetic field with a human body form. If we knew the density of those changes we could obtain the images of the internal anatomy. And how do we know the density? By means of radiofrequency.
Radiofrequency
Radiofrequency gives energy to the spin of the protons, increasing the amplitude of their turns without changing the frequency. Now the 3D-magnetic map becomes a 3D-map of energy. Each particular point in the body has a particular energy (or intensity, in terms of radiofrequency). If radiofrequency is no longer applied to the body, the proton-spins return to their original state and in that moment release radiofrequency waves. Now we have a 3D-map of radiofrequency. And radiofrequency can be registered with coils.
Computers
The rest of the procedure is done by the computers that convert the signal intensity, the signal phase, and the signal location into a matrix of dots with different values. Each value is represented with a tone of gray. The minimum value is black, and the maximum value is white, and in between is a scale of gray. At this point WE HAVE THE MR IMAGE!
How the FMRI Works
In functional imaging we have two components: a task and a result. The task is an action or activity that the subject does in order to produce a particular activation of the brain. For example, moving the right hand fingers continuously is a motor task that "activates" the brain cortex in the left frontal lobe. The result in fMRI is an image which depicts this activation.
The task can be of any type. Motor, feeling a sensation, having a perception, thinking in abstract words, attending to a changing stimulus, listening to music, comprehending a story, and many others. The task will produce this sequence of events:
- Increases in metabolism of the brain area involved in the task
- Increases in volume of blood in that particular region
- Increases in oxygen level
- Changes in the local magnetic field (Do you remember the 3D-magnetic field map discussed earlier?)
- Changes in the intensity of the energy (radiofrequency) in the same area.
In brief, the task elicits activity of a region of the brain, and this activity changes the intensity of the radiofrequency coming from that part. This is a very small change. But, if we repeat the task several times we are able to sum the changes to get a significant result that can be registered.
We compare a person's brain activity during a particular task with their activity level during a resting state. However, the brain works continuously, even during the resting state. For that reason the resting state is a baseline of the background activity of the brain.
So we must know the value of the background signal activity and the value of the signal related to the task. To do this, hundreds of images of the region targeted are taken during a few minutes. Meanwhile, the subject is alternating between periods of activity (performing the task) and periods of rest. In this manner we have a group of images of a region taken during the task, and the same number of images of the same region during rest. Two averaged images are obtained corresponding to two conditions in which one is "activated".
As we have seen before, images are the result of the values of the signal intensity, encoded on a gray scale. These values can be added, subtracted, etc. Well, that is exactly the next step. Powerful computers subtract the baseline values from the activated ones. These values of activation are then transformed into a map of colors. Usually the scale of this map varies from blue to red in a increasing manner. Finally, the colors are overlaid upon anatomical images, in a similar way that the weather maps are overlaid upon geographical pictures.
How fMRI can be helpful in Medicine
fMRI has a particular terminology. The next images explain the must important terms used to describe one experiment.

One epoch is a period of time in which something is occurring.
- ON: The name of the epoch in which the task is performed
- OFF: The name of the epoch in which the subject is at rest
A scan is the image obtained in each unit of time
A level is the localization of the site to explore. Several levels can be explored at once.

In this graphic is shown: 5 epochs ON, in which the subject performs the task; 5 epochs OFF, in which the subject is at rest; each epoch lasts 30 seconds for a total length of the experiment of 5 minutes. Four levels of the brain are explored, with 120 images (or scans) divided in alternated groups of 12.
A Final Result

The areas in color depict the activation of the brain regions involved in hearing and comprehending the human voice. The left hemisphere shows greater activation.
How fMRI Works
In order to understand how functional magnetic resonance (fMRI) works it is important to know some basic things about brain anatomy and function. Also, it is necessary to know some magnetic resonance imaging (MRI) basic facts. Let's begin with the first part:
A very short course on Neuroanatomy
The brain is divided in two hemispheres, the right and the left. Each hemisphere is divided into lobes. And each lobe has different areas as is depicted in the next figure taken with permission from http://www.umich.edu/~cogneuro/home.html
 Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Areas 1,2,3, and 5 "feel" the sensations of touch, position and temperature. Areas 4, 6, and 8 move the muscles of the body. Areas like 44, 45 and 47 produce language. Areas 41 and 42 "hear", areas 17 to 19 "see".
Other areas like 37, 46, 10, 22, 38 are in charge of the complex process involving memory, internal language, comprehension and planning.
This is a regionalization of the function. Also, there is something called "lateralization" of the function. This means that a particular activity can be predominantly located in one hemisphere. That happens with language. In almost all right-handed people the left hemisphere is dominant for language.
Each thing we do, any thought, feeling or sensation is produced by the activity of cells localized in a specific area of the brain. For example, if you receive the credit card bill and you panic, that is because a group of cells in the inner part of the brain start to fire, increasing its electrical current, transmission, and metabolism. These cells need more blood since they need more fuel. And it happens that when an area of the brain becomes activated, that area receives more blood because in that region there is dilatation of the tiny blood vessels.
So, ultimately, any action of the brain occurs along with an increase of blood at the point of the cortex where that action is commanded.
Now, let's continue to the second part.
A very, very short course on MRI basics
MRI is a procedure to see the anatomy of the internal organs of the body. It is based on three things: magnetism, radiofrequency and computers.
Nevertheless, to understand how an MRI works and how these three things can show us the anatomy of the brain (and the whole body) it is important to know five other things:
- Our body contains large amounts of water.
- Water is formed by hydrogen and oxygen (The hydrogen is presented basically as protons).
- Protons are positive charges that spin.
- A charge that spins creates a magnetic field that can be oriented. In other words, these micro-magnets can be up or down, right or left.
- The spin of these micro-magnets have a specific frequency (or velocity).
And that is it. Let's return to the three things needed to perform an MRI: magnetism, radiofrequency and computers.
Magnetism
The magnetic resonance machine is a big and strong magnet. When the body is inside, every proton of the body is oriented in the same way (for instance, with the positive pole up). This means that the body becomes a magnet, but a non-homogeneous magnet, because the amount of water in each part of the body varies with the specific characteristics of the organ: the layer, the location, and even the types of cells. Therefore, the human body can be pictured as a 3D-map of changes of magnetic field with a human body form. If we knew the density of those changes we could obtain the images of the internal anatomy. And how do we know the density? By means of radiofrequency.
Radiofrequency
Radiofrequency gives energy to the spin of the protons, increasing the amplitude of their turns without changing the frequency. Now the 3D-magnetic map becomes a 3D-map of energy. Each particular point in the body has a particular energy (or intensity, in terms of radiofrequency). If radiofrequency is no longer applied to the body, the proton-spins return to their original state and in that moment release radiofrequency waves. Now we have a 3D-map of radiofrequency. And radiofrequency can be registered with coils.
Computers
The rest of the procedure is done by the computers that convert the signal intensity, the signal phase, and the signal location into a matrix of dots with different values. Each value is represented with a tone of gray. The minimum value is black, and the maximum value is white, and in between is a scale of gray. At this point WE HAVE THE MR IMAGE!
How the FMRI Works
In functional imaging we have two components: a task and a result. The task is an action or activity that the subject does in order to produce a particular activation of the brain. For example, moving the right hand fingers continuously is a motor task that "activates" the brain cortex in the left frontal lobe. The result in fMRI is an image which depicts this activation.
The task can be of any type. Motor, feeling a sensation, having a perception, thinking in abstract words, attending to a changing stimulus, listening to music, comprehending a story, and many others. The task will produce this sequence of events:
- Increases in metabolism of the brain area involved in the task
- Increases in volume of blood in that particular region
- Increases in oxygen level
- Changes in the local magnetic field (Do you remember the 3D-magnetic field map discussed earlier?)
- Changes in the intensity of the energy (radiofrequency) in the same area.
In brief, the task elicits activity of a region of the brain, and this activity changes the intensity of the radiofrequency coming from that part. This is a very small change. But, if we repeat the task several times we are able to sum the changes to get a significant result that can be registered.
We compare a person's brain activity during a particular task with their activity level during a resting state. However, the brain works continuously, even during the resting state. For that reason the resting state is a baseline of the background activity of the brain.
So we must know the value of the background signal activity and the value of the signal related to the task. To do this, hundreds of images of the region targeted are taken during a few minutes. Meanwhile, the subject is alternating between periods of activity (performing the task) and periods of rest. In this manner we have a group of images of a region taken during the task, and the same number of images of the same region during rest. Two averaged images are obtained corresponding to two conditions in which one is "activated".
As we have seen before, images are the result of the values of the signal intensity, encoded on a gray scale. These values can be added, subtracted, etc. Well, that is exactly the next step. Powerful computers subtract the baseline values from the activated ones. These values of activation are then transformed into a map of colors. Usually the scale of this map varies from blue to red in a increasing manner. Finally, the colors are overlaid upon anatomical images, in a similar way that the weather maps are overlaid upon geographical pictures.
How fMRI can be helpful in Medicine
fMRI has a particular terminology. The next images explain the must important terms used to describe one experiment.

One epoch is a period of time in which something is occurring.
- ON: The name of the epoch in which the task is performed
- OFF: The name of the epoch in which the subject is at rest
A scan is the image obtained in each unit of time
A level is the localization of the site to explore. Several levels can be explored at once.

In this graphic is shown: 5 epochs ON, in which the subject performs the task; 5 epochs OFF, in which the subject is at rest; each epoch lasts 30 seconds for a total length of the experiment of 5 minutes. Four levels of the brain are explored, with 120 images (or scans) divided in alternated groups of 12.
A Final Result

The areas in color depict the activation of the brain regions involved in hearing and comprehending the human voice. The left hemisphere shows greater activation.
How fMRI Works
In order to understand how functional magnetic resonance (fMRI) works it is important to know some basic things about brain anatomy and function. Also, it is necessary to know some magnetic resonance imaging (MRI) basic facts. Let's begin with the first part:
A very short course on Neuroanatomy
The brain is divided in two hemispheres, the right and the left. Each hemisphere is divided into lobes. And each lobe has different areas as is depicted in the next figure taken with permission from http://www.umich.edu/~cogneuro/home.html
 Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Each region in a different color is a lobe. In yellow the frontal lobe; in green, the parietal lobe; the occipital lobe appears blue, while the temporal lobe is red.
Areas 1,2,3, and 5 "feel" the sensations of touch, position and temperature. Areas 4, 6, and 8 move the muscles of the body. Areas like 44, 45 and 47 produce language. Areas 41 and 42 "hear", areas 17 to 19 "see".
Other areas like 37, 46, 10, 22, 38 are in charge of the complex process involving memory, internal language, comprehension and planning.
This is a regionalization of the function. Also, there is something called "lateralization" of the function. This means that a particular activity can be predominantly located in one hemisphere. That happens with language. In almost all right-handed people the left hemisphere is dominant for language.
Each thing we do, any thought, feeling or sensation is produced by the activity of cells localized in a specific area of the brain. For example, if you receive the credit card bill and you panic, that is because a group of cells in the inner part of the brain start to fire, increasing its electrical current, transmission, and metabolism. These cells need more blood since they need more fuel. And it happens that when an area of the brain becomes activated, that area receives more blood because in that region there is dilatation of the tiny blood vessels.
So, ultimately, any action of the brain occurs along with an increase of blood at the point of the cortex where that action is commanded.
Now, let's continue to the second part.
A very, very short course on MRI basics
MRI is a procedure to see the anatomy of the internal organs of the body. It is based on three things: magnetism, radiofrequency and computers.
Nevertheless, to understand how an MRI works and how these three things can show us the anatomy of the brain (and the whole body) it is important to know five other things:
- Our body contains large amounts of water.
- Water is formed by hydrogen and oxygen (The hydrogen is presented basically as protons).
- Protons are positive charges that spin.
- A charge that spins creates a magnetic field that can be oriented. In other words, these micro-magnets can be up or down, right or left.
- The spin of these micro-magnets have a specific frequency (or velocity).
And that is it. Let's return to the three things needed to perform an MRI: magnetism, radiofrequency and computers.
Magnetism
The magnetic resonance machine is a big and strong magnet. When the body is inside, every proton of the body is oriented in the same way (for instance, with the positive pole up). This means that the body becomes a magnet, but a non-homogeneous magnet, because the amount of water in each part of the body varies with the specific characteristics of the organ: the layer, the location, and even the types of cells. Therefore, the human body can be pictured as a 3D-map of changes of magnetic field with a human body form. If we knew the density of those changes we could obtain the images of the internal anatomy. And how do we know the density? By means of radiofrequency.
Radiofrequency
Radiofrequency gives energy to the spin of the protons, increasing the amplitude of their turns without changing the frequency. Now the 3D-magnetic map becomes a 3D-map of energy. Each particular point in the body has a particular energy (or intensity, in terms of radiofrequency). If radiofrequency is no longer applied to the body, the proton-spins return to their original state and in that moment release radiofrequency waves. Now we have a 3D-map of radiofrequency. And radiofrequency can be registered with coils.
Computers
The rest of the procedure is done by the computers that convert the signal intensity, the signal phase, and the signal location into a matrix of dots with different values. Each value is represented with a tone of gray. The minimum value is black, and the maximum value is white, and in between is a scale of gray. At this point WE HAVE THE MR IMAGE!
How the FMRI Works
In functional imaging we have two components: a task and a result. The task is an action or activity that the subject does in order to produce a particular activation of the brain. For example, moving the right hand fingers continuously is a motor task that "activates" the brain cortex in the left frontal lobe. The result in fMRI is an image which depicts this activation.
The task can be of any type. Motor, feeling a sensation, having a perception, thinking in abstract words, attending to a changing stimulus, listening to music, comprehending a story, and many others. The task will produce this sequence of events:
- Increases in metabolism of the brain area involved in the task
- Increases in volume of blood in that particular region
- Increases in oxygen level
- Changes in the local magnetic field (Do you remember the 3D-magnetic field map discussed earlier?)
- Changes in the intensity of the energy (radiofrequency) in the same area.
In brief, the task elicits activity of a region of the brain, and this activity changes the intensity of the radiofrequency coming from that part. This is a very small change. But, if we repeat the task several times we are able to sum the changes to get a significant result that can be registered.
We compare a person's brain activity during a particular task with their activity level during a resting state. However, the brain works continuously, even during the resting state. For that reason the resting state is a baseline of the background activity of the brain.
So we must know the value of the background signal activity and the value of the signal related to the task. To do this, hundreds of images of the region targeted are taken during a few minutes. Meanwhile, the subject is alternating between periods of activity (performing the task) and periods of rest. In this manner we have a group of images of a region taken during the task, and the same number of images of the same region during rest. Two averaged images are obtained corresponding to two conditions in which one is "activated".
As we have seen before, images are the result of the values of the signal intensity, encoded on a gray scale. These values can be added, subtracted, etc. Well, that is exactly the next step. Powerful computers subtract the baseline values from the activated ones. These values of activation are then transformed into a map of colors. Usually the scale of this map varies from blue to red in a increasing manner. Finally, the colors are overlaid upon anatomical images, in a similar way that the weather maps are overlaid upon geographical pictures.
How fMRI can be helpful in Medicine
fMRI has a particular terminology. The next images explain the must important terms used to describe one experiment.

One epoch is a period of time in which something is occurring.
- ON: The name of the epoch in which the task is performed
- OFF: The name of the epoch in which the subject is at rest
A scan is the image obtained in each unit of time
A level is the localization of the site to explore. Several levels can be explored at once.

In this graphic is shown: 5 epochs ON, in which the subject performs the task; 5 epochs OFF, in which the subject is at rest; each epoch lasts 30 seconds for a total length of the experiment of 5 minutes. Four levels of the brain are explored, with 120 images (or scans) divided in alternated groups of 12.
A Final Result

The areas in color depict the activation of the brain regions involved in hearing and comprehending the human voice. The left hemisphere shows greater activation.
Screenings and Events Calendar
Page re-directs to victorcenter.org
Screenings and Events Calendar
Page re-directs to victorcenter.org
Donate to the Victor Center
Funding for the Victor Center for Prevention of Jewish Genetic Diseases at Nicklaus Children's is supported by the Nicklaus Children's Hospital Foundation.
Donate to the Victor Center
Funding for the Victor Center for Prevention of Jewish Genetic Diseases at Nicklaus Children's is supported by the Nicklaus Children's Hospital Foundation.
News
News
fMRI Clinical Cases
Case 1
| Patient |
Female patient, age 19. Presurgical demonstration of eloquent areas |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Activation of middle and inferior left frontal gyri, precentral left cortex, left angular gyri, and scattered areas in the parietal lobes. |
| Comments |
The main activated area in this phonetic fluency task is the superior aspect of the left inferior frontal gyrus. In contrast, the main area of activation on tasks requiring generation of verbs is the inferior aspect of Broca's area, along with the anterior insula. |
Case 2
| Patient |
Male patient, age 13. Presurgical mapping of eloquent areas. |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Strong activation in left middle and inferior frontal gyri, and left postcentral sulcus. There is no significant activation in the right hemisphere |
Case 3
| Patient |
Male patient, age 14, with seizures |
| Paradigm |
Tapping task
ON: Alternating Finger Tapping with the right hand
OFF: Think of nothing |
| Results |
Cortex of the left central sulcus was strongly activated. The relation to the tumor is clearly depicted by the images. |
| Comments |
The tumor was resected without postoperatory motor deficit |
Case 4
| Patient |
Male patient, 9 years old with a neoplastic lesion in the left sylvian fissure. No language deficit |
| Paradigm |
Verbal fluency task
ON: Think of actions related to given nouns
OFF: Think of nothing |
| Results |
Obvious left language dominance.
Broca's area is well depicted along with left superior frontal gyrus.
Activation in the right cerebellum has been described associated with expressive language tasks.
A Case of Acalculia.
|
fMRI Clinical Cases
Case 1
| Patient |
Female patient, age 19. Presurgical demonstration of eloquent areas |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Activation of middle and inferior left frontal gyri, precentral left cortex, left angular gyri, and scattered areas in the parietal lobes. |
| Comments |
The main activated area in this phonetic fluency task is the superior aspect of the left inferior frontal gyrus. In contrast, the main area of activation on tasks requiring generation of verbs is the inferior aspect of Broca's area, along with the anterior insula. |
Case 2
| Patient |
Male patient, age 13. Presurgical mapping of eloquent areas. |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Strong activation in left middle and inferior frontal gyri, and left postcentral sulcus. There is no significant activation in the right hemisphere |
Case 3
| Patient |
Male patient, age 14, with seizures |
| Paradigm |
Tapping task
ON: Alternating Finger Tapping with the right hand
OFF: Think of nothing |
| Results |
Cortex of the left central sulcus was strongly activated. The relation to the tumor is clearly depicted by the images. |
| Comments |
The tumor was resected without postoperatory motor deficit |
Case 4
| Patient |
Male patient, 9 years old with a neoplastic lesion in the left sylvian fissure. No language deficit |
| Paradigm |
Verbal fluency task
ON: Think of actions related to given nouns
OFF: Think of nothing |
| Results |
Obvious left language dominance.
Broca's area is well depicted along with left superior frontal gyrus.
Activation in the right cerebellum has been described associated with expressive language tasks.
A Case of Acalculia.
|
fMRI Clinical Cases
Case 1
| Patient |
Female patient, age 19. Presurgical demonstration of eloquent areas |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Activation of middle and inferior left frontal gyri, precentral left cortex, left angular gyri, and scattered areas in the parietal lobes. |
| Comments |
The main activated area in this phonetic fluency task is the superior aspect of the left inferior frontal gyrus. In contrast, the main area of activation on tasks requiring generation of verbs is the inferior aspect of Broca's area, along with the anterior insula. |
Case 2
| Patient |
Male patient, age 13. Presurgical mapping of eloquent areas. |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Strong activation in left middle and inferior frontal gyri, and left postcentral sulcus. There is no significant activation in the right hemisphere |
Case 3
| Patient |
Male patient, age 14, with seizures |
| Paradigm |
Tapping task
ON: Alternating Finger Tapping with the right hand
OFF: Think of nothing |
| Results |
Cortex of the left central sulcus was strongly activated. The relation to the tumor is clearly depicted by the images. |
| Comments |
The tumor was resected without postoperatory motor deficit |
Case 4
| Patient |
Male patient, 9 years old with a neoplastic lesion in the left sylvian fissure. No language deficit |
| Paradigm |
Verbal fluency task
ON: Think of actions related to given nouns
OFF: Think of nothing |
| Results |
Obvious left language dominance.
Broca's area is well depicted along with left superior frontal gyrus.
Activation in the right cerebellum has been described associated with expressive language tasks.
A Case of Acalculia.
|
fMRI Clinical Cases
Case 1
| Patient |
Female patient, age 19. Presurgical demonstration of eloquent areas |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Activation of middle and inferior left frontal gyri, precentral left cortex, left angular gyri, and scattered areas in the parietal lobes. |
| Comments |
The main activated area in this phonetic fluency task is the superior aspect of the left inferior frontal gyrus. In contrast, the main area of activation on tasks requiring generation of verbs is the inferior aspect of Broca's area, along with the anterior insula. |
Case 2
| Patient |
Male patient, age 13. Presurgical mapping of eloquent areas. |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Strong activation in left middle and inferior frontal gyri, and left postcentral sulcus. There is no significant activation in the right hemisphere |
Case 3
| Patient |
Male patient, age 14, with seizures |
| Paradigm |
Tapping task
ON: Alternating Finger Tapping with the right hand
OFF: Think of nothing |
| Results |
Cortex of the left central sulcus was strongly activated. The relation to the tumor is clearly depicted by the images. |
| Comments |
The tumor was resected without postoperatory motor deficit |
Case 4
| Patient |
Male patient, 9 years old with a neoplastic lesion in the left sylvian fissure. No language deficit |
| Paradigm |
Verbal fluency task
ON: Think of actions related to given nouns
OFF: Think of nothing |
| Results |
Obvious left language dominance.
Broca's area is well depicted along with left superior frontal gyrus.
Activation in the right cerebellum has been described associated with expressive language tasks.
A Case of Acalculia.
|
fMRI Clinical Cases
Case 1
| Patient |
Female patient, age 19. Presurgical demonstration of eloquent areas |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Activation of middle and inferior left frontal gyri, precentral left cortex, left angular gyri, and scattered areas in the parietal lobes. |
| Comments |
The main activated area in this phonetic fluency task is the superior aspect of the left inferior frontal gyrus. In contrast, the main area of activation on tasks requiring generation of verbs is the inferior aspect of Broca's area, along with the anterior insula. |
Case 2
| Patient |
Male patient, age 13. Presurgical mapping of eloquent areas. |
| Paradigm |
Phonetic fluency
ON: Silent word generation starting with a given letter
OFF: Think of nothing |
| Results |
Strong activation in left middle and inferior frontal gyri, and left postcentral sulcus. There is no significant activation in the right hemisphere |
Case 3
| Patient |
Male patient, age 14, with seizures |
| Paradigm |
Tapping task
ON: Alternating Finger Tapping with the right hand
OFF: Think of nothing |
| Results |
Cortex of the left central sulcus was strongly activated. The relation to the tumor is clearly depicted by the images. |
| Comments |
The tumor was resected without postoperatory motor deficit |
Case 4
| Patient |
Male patient, 9 years old with a neoplastic lesion in the left sylvian fissure. No language deficit |
| Paradigm |
Verbal fluency task
ON: Think of actions related to given nouns
OFF: Think of nothing |
| Results |
Obvious left language dominance.
Broca's area is well depicted along with left superior frontal gyrus.
Activation in the right cerebellum has been described associated with expressive language tasks.
A Case of Acalculia.
|
fMRI Auditory Mapping
Case 1
| Subject |
Right handed 20 year-old-man |
| Paradigm |
ON: Passive hearing music (single notes, unfamiliar tune), in binaural-monophonic presentation
OFF: Hearing the background noise
|
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Activation |
There is assymetric activation which is greater on the left in Heschl's gyrus and more extensive on the right supramarginal gyrus. |
fMRI Auditory Mapping
Case 1
| Subject |
Right handed 20 year-old-man |
| Paradigm |
ON: Passive hearing music (single notes, unfamiliar tune), in binaural-monophonic presentation
OFF: Hearing the background noise
|
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Activation |
There is assymetric activation which is greater on the left in Heschl's gyrus and more extensive on the right supramarginal gyrus. |
fMRI Auditory Mapping
Case 1
| Subject |
Right handed 20 year-old-man |
| Paradigm |
ON: Passive hearing music (single notes, unfamiliar tune), in binaural-monophonic presentation
OFF: Hearing the background noise
|
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Activation |
There is assymetric activation which is greater on the left in Heschl's gyrus and more extensive on the right supramarginal gyrus. |
fMRI Auditory Mapping
Case 1
| Subject |
Right handed 20 year-old-man |
| Paradigm |
ON: Passive hearing music (single notes, unfamiliar tune), in binaural-monophonic presentation
OFF: Hearing the background noise
|
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Activation |
There is assymetric activation which is greater on the left in Heschl's gyrus and more extensive on the right supramarginal gyrus. |
fMRI Auditory Mapping
Case 1
| Subject |
Right handed 20 year-old-man |
| Paradigm |
ON: Passive hearing music (single notes, unfamiliar tune), in binaural-monophonic presentation
OFF: Hearing the background noise
|
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Activation |
There is assymetric activation which is greater on the left in Heschl's gyrus and more extensive on the right supramarginal gyrus. |
3D Functional Magnetic Resonance
Conventional MR images are two-dimensional representation of intensities occurring at a given level or slice.
These images may be presented in axial, coronal and sagittal planes.
The most frequent plane used in fMR is the axial plane which shows the localization of structures or activation in a X (right to left) and a Y (anterior to posterior) axes. Since these images are usually obtained in oblique planes it is difficult to know the precise level in the remaining Z (cranio-caudal) axis.
3D MRI scans allow us to present images with a volumetric appearance. These 3D MRI images have proven to be useful to guide surgical resections.
Types of 3D MRI scans
Orthogonal Views
Orthogonal views refer to a set of mutually perpendicular images. This localizes a given region of activation to the three axes that define the volumetric shape of the brain.
Case 1

Adult volunteer generating verbs. On the axial view the exact location of activation in the temporal lobe is difficult to determine. The black lines in the axial view correspond to the location of the coronal and sagittal views. These three views allow us to determine the location of activation in the middle temporal gyrus.
Case 2

Right handed adult male patient with intractable seizures coming from the left temporal pole, performing a language task consisting of listening to a story. No structural lesion was found in this region. A left temporal resection is planned. The orthogonal views permit evaluating of the extent of the language areas and the distance between its anterior border and the temporal pole (orange line). The neurosurgeon may use these findings as a guide to tailor the temporal resection.
Surface Rendering
Surface rendering is a computer post processing method that removes the skin and the skull to allow us to see the brain surface. The anatomy of gyri and sulci are displayed in the same way the neurosurgeon sees the brain. Functional maps can be superimposed on these images. Some activation may take place deep in the sulci which may be presented on these images bleeding through the cortical surface.
Case 1

Right handed 15 year-old-boy with intractable epilepsy performing a verbal "repetition task." The surface rendition beautifully depicts the activation occurring in the posterior third of the right superior temporal gyrus and extending toward supramarginal gyrus and Brodmann's area 7. The areas of activation are better displayed than with conventional 2D MR images.
Case 2

Right handed 11 year-old-girl with intractable epilepsy who had a left frontal resection two years ago for control of seizures. Persistence of the seizures prompted this fMR exam for re-evaluation. The images demonstrated activation obtained from a "Verb Generation Task." The study depicted Broca's area and part of Wernicke's (Brodmann's area 37), which is believed to be a repository for words. A second resection was performed based on these findings. The patient experienced no post-operative aphasia and remains seizure free.
3D Rendering + Orthogonal View
Surface rendering and orthogonal views can be combined in one procedure. This allows us to see activation (or lesions) of the cortex and deep structures of the brain. The bleeding through of activation is obviated. External landmarks of the head and face may also help in surgical navigation.
Surface and orthogonal rendering of the brain is viewed in natural anatomical orientation. This means that the structures appear as if they were under direct sight. For that reason the left hemisphere appears on the right side of the left-top-rostral view, and on the left side on the left-top-posterior view. The fMR image presented here depicts activation of the angular gyrus observed in a right-left laterality decision task. The hemi-axial plane shows the activation placed in the deep portion of the left parietal sulcus.
Case 1
11-year-old right handed boy with intractable epilepsy and left hemiparesis. Patient was mapped for language as part of his work up for epilepsy surgery with a "Semantic Fluency Task."

3D-surface rendering and orthogonal views. The images show activation of Broca's area along pars orbitales, triangularis and opercularis in the left hemisphere. Activation is also observed in visual areas likely related to visual strategies. Activation of the basal ganglia is occasionally seen as in this case. Activation can be localized on one image including the cortex, the sylvian fissure, the calcarine fissure, the lateral ventricles and along the midline.
Case 2
Right handed 11 year-old-girl with persistent intractable epilepsy who had a partial left frontal resection . Patient underwent language mapping with fMR.
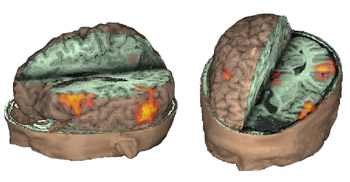
These images complement case 2 presented in "Surface Rendering." Activation is obtained with a "verb generation" task in Wernicke's area not only along the cortical surface but deep along the gyri.
Case 3
13 year old right handed-boy, with temporal lobe epilepsy. A multicystic oligodendroglioma was found in the left temporal lobe (black arrows). Functional MRI was prescribed to map language areas, prior to surgical resection.

A 3D-fMRI depicts the mass in the left temporal pole. The activation was obtained utilizing a "Repetition Task" paradigm (bubbles in yellow, orange, and red). The relationship between the lesion and the speech areas are beautifully displayed.
Case 4
Right handed 19 year-old female volunteer, performing a Stroop-like paradigm. This task involves inhibition, potentially useful in ADHD evaluation.

Activation is located in the cingulate gyrus, right inferior frontal, and supramarginal gyrus (red bubbles). The blue bubble located in the right frontal pole corresponds to inhibited areas. The combination of orthogonal axial and sagittal planes allow simultaneous presentation.
Triple Rendering
The neurosurgeon has a restricted view of the brain through the small window of the craniotomy. Modern neuroimaging can provide anatomy in three dimensions, and a much wider window.
Case 1
27-year-old right handed woman who underwent MRI and MRV to rule out a structural lesion. The patient volunteered to perform a verb generation task.

The image shows the fusion of three different procedures. In gray scale is the volumetric rendition of the brain obtained from the MRI sequence. In blue are depicted the surface veins and sinus of the left hemisphere from the MR-venogram. In yellow and red appears activation obtained from the echo-planar sequence used for functional MRI.
Case 2
17 year-old right handed boy with intractable epilepsy of partial motor type. MRI showed signal abnormality in the left middle frontal gyrus consistent with cortical dysplasia.

MRI of the head with partial exposure of the brain and skull. An axial view located at the superior third of the inferior frontal gyrus demonstrates in red the activation obtained with a verb generation task. The yellow spot represents the lesion and is derived from a fluid attenuated inversion recovery (FLAIR) sequence, and rendered with the rest of images, revealing the relationship between the lesion and the eloquent areas.
Case 3
15 year-old right handed girl with sensory-motor partial seizures involving the left hand since the age of 5. MRI showed a focal signal abnormality in the right postcentral gyrus consistent with a developmental tumor without changes over 2 years.

MRI of the brain appears in gray scale, functional MR activation is in yellow and red, the tumor is purple (light blue arrow), and the veins are blue. The tumor appears located in the post-central gyrus lateral and rostral to the functional activation. The relationship between the tumor and the functional activation was confirmed during awake intraoperative mapping. The venous landmarks provided useful information to the operating surgeon. The patient's tumor was removed without residual monoplegia. The patient had only transient loss of stereognosis and proprioception involving the 3rd, 4th, and 5th fingers, post-operatively.
3D Functional Magnetic Resonance
Conventional MR images are two-dimensional representation of intensities occurring at a given level or slice.
These images may be presented in axial, coronal and sagittal planes.
The most frequent plane used in fMR is the axial plane which shows the localization of structures or activation in a X (right to left) and a Y (anterior to posterior) axes. Since these images are usually obtained in oblique planes it is difficult to know the precise level in the remaining Z (cranio-caudal) axis.
3D MRI scans allow us to present images with a volumetric appearance. These 3D MRI images have proven to be useful to guide surgical resections.
Types of 3D MRI scans
Orthogonal Views
Orthogonal views refer to a set of mutually perpendicular images. This localizes a given region of activation to the three axes that define the volumetric shape of the brain.
Case 1

Adult volunteer generating verbs. On the axial view the exact location of activation in the temporal lobe is difficult to determine. The black lines in the axial view correspond to the location of the coronal and sagittal views. These three views allow us to determine the location of activation in the middle temporal gyrus.
Case 2

Right handed adult male patient with intractable seizures coming from the left temporal pole, performing a language task consisting of listening to a story. No structural lesion was found in this region. A left temporal resection is planned. The orthogonal views permit evaluating of the extent of the language areas and the distance between its anterior border and the temporal pole (orange line). The neurosurgeon may use these findings as a guide to tailor the temporal resection.
Surface Rendering
Surface rendering is a computer post processing method that removes the skin and the skull to allow us to see the brain surface. The anatomy of gyri and sulci are displayed in the same way the neurosurgeon sees the brain. Functional maps can be superimposed on these images. Some activation may take place deep in the sulci which may be presented on these images bleeding through the cortical surface.
Case 1

Right handed 15 year-old-boy with intractable epilepsy performing a verbal "repetition task." The surface rendition beautifully depicts the activation occurring in the posterior third of the right superior temporal gyrus and extending toward supramarginal gyrus and Brodmann's area 7. The areas of activation are better displayed than with conventional 2D MR images.
Case 2

Right handed 11 year-old-girl with intractable epilepsy who had a left frontal resection two years ago for control of seizures. Persistence of the seizures prompted this fMR exam for re-evaluation. The images demonstrated activation obtained from a "Verb Generation Task." The study depicted Broca's area and part of Wernicke's (Brodmann's area 37), which is believed to be a repository for words. A second resection was performed based on these findings. The patient experienced no post-operative aphasia and remains seizure free.
3D Rendering + Orthogonal View
Surface rendering and orthogonal views can be combined in one procedure. This allows us to see activation (or lesions) of the cortex and deep structures of the brain. The bleeding through of activation is obviated. External landmarks of the head and face may also help in surgical navigation.
Surface and orthogonal rendering of the brain is viewed in natural anatomical orientation. This means that the structures appear as if they were under direct sight. For that reason the left hemisphere appears on the right side of the left-top-rostral view, and on the left side on the left-top-posterior view. The fMR image presented here depicts activation of the angular gyrus observed in a right-left laterality decision task. The hemi-axial plane shows the activation placed in the deep portion of the left parietal sulcus.
Case 1
11-year-old right handed boy with intractable epilepsy and left hemiparesis. Patient was mapped for language as part of his work up for epilepsy surgery with a "Semantic Fluency Task."

3D-surface rendering and orthogonal views. The images show activation of Broca's area along pars orbitales, triangularis and opercularis in the left hemisphere. Activation is also observed in visual areas likely related to visual strategies. Activation of the basal ganglia is occasionally seen as in this case. Activation can be localized on one image including the cortex, the sylvian fissure, the calcarine fissure, the lateral ventricles and along the midline.
Case 2
Right handed 11 year-old-girl with persistent intractable epilepsy who had a partial left frontal resection . Patient underwent language mapping with fMR.
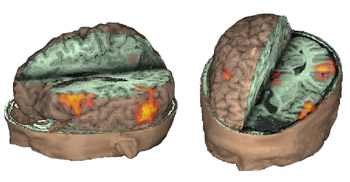
These images complement case 2 presented in "Surface Rendering." Activation is obtained with a "verb generation" task in Wernicke's area not only along the cortical surface but deep along the gyri.
Case 3
13 year old right handed-boy, with temporal lobe epilepsy. A multicystic oligodendroglioma was found in the left temporal lobe (black arrows). Functional MRI was prescribed to map language areas, prior to surgical resection.

A 3D-fMRI depicts the mass in the left temporal pole. The activation was obtained utilizing a "Repetition Task" paradigm (bubbles in yellow, orange, and red). The relationship between the lesion and the speech areas are beautifully displayed.
Case 4
Right handed 19 year-old female volunteer, performing a Stroop-like paradigm. This task involves inhibition, potentially useful in ADHD evaluation.

Activation is located in the cingulate gyrus, right inferior frontal, and supramarginal gyrus (red bubbles). The blue bubble located in the right frontal pole corresponds to inhibited areas. The combination of orthogonal axial and sagittal planes allow simultaneous presentation.
Triple Rendering
The neurosurgeon has a restricted view of the brain through the small window of the craniotomy. Modern neuroimaging can provide anatomy in three dimensions, and a much wider window.
Case 1
27-year-old right handed woman who underwent MRI and MRV to rule out a structural lesion. The patient volunteered to perform a verb generation task.

The image shows the fusion of three different procedures. In gray scale is the volumetric rendition of the brain obtained from the MRI sequence. In blue are depicted the surface veins and sinus of the left hemisphere from the MR-venogram. In yellow and red appears activation obtained from the echo-planar sequence used for functional MRI.
Case 2
17 year-old right handed boy with intractable epilepsy of partial motor type. MRI showed signal abnormality in the left middle frontal gyrus consistent with cortical dysplasia.

MRI of the head with partial exposure of the brain and skull. An axial view located at the superior third of the inferior frontal gyrus demonstrates in red the activation obtained with a verb generation task. The yellow spot represents the lesion and is derived from a fluid attenuated inversion recovery (FLAIR) sequence, and rendered with the rest of images, revealing the relationship between the lesion and the eloquent areas.
Case 3
15 year-old right handed girl with sensory-motor partial seizures involving the left hand since the age of 5. MRI showed a focal signal abnormality in the right postcentral gyrus consistent with a developmental tumor without changes over 2 years.

MRI of the brain appears in gray scale, functional MR activation is in yellow and red, the tumor is purple (light blue arrow), and the veins are blue. The tumor appears located in the post-central gyrus lateral and rostral to the functional activation. The relationship between the tumor and the functional activation was confirmed during awake intraoperative mapping. The venous landmarks provided useful information to the operating surgeon. The patient's tumor was removed without residual monoplegia. The patient had only transient loss of stereognosis and proprioception involving the 3rd, 4th, and 5th fingers, post-operatively.
3D Functional Magnetic Resonance
Conventional MR images are two-dimensional representation of intensities occurring at a given level or slice.
These images may be presented in axial, coronal and sagittal planes.
The most frequent plane used in fMR is the axial plane which shows the localization of structures or activation in a X (right to left) and a Y (anterior to posterior) axes. Since these images are usually obtained in oblique planes it is difficult to know the precise level in the remaining Z (cranio-caudal) axis.
3D MRI scans allow us to present images with a volumetric appearance. These 3D MRI images have proven to be useful to guide surgical resections.
Types of 3D MRI scans
Orthogonal Views
Orthogonal views refer to a set of mutually perpendicular images. This localizes a given region of activation to the three axes that define the volumetric shape of the brain.
Case 1

Adult volunteer generating verbs. On the axial view the exact location of activation in the temporal lobe is difficult to determine. The black lines in the axial view correspond to the location of the coronal and sagittal views. These three views allow us to determine the location of activation in the middle temporal gyrus.
Case 2

Right handed adult male patient with intractable seizures coming from the left temporal pole, performing a language task consisting of listening to a story. No structural lesion was found in this region. A left temporal resection is planned. The orthogonal views permit evaluating of the extent of the language areas and the distance between its anterior border and the temporal pole (orange line). The neurosurgeon may use these findings as a guide to tailor the temporal resection.
Surface Rendering
Surface rendering is a computer post processing method that removes the skin and the skull to allow us to see the brain surface. The anatomy of gyri and sulci are displayed in the same way the neurosurgeon sees the brain. Functional maps can be superimposed on these images. Some activation may take place deep in the sulci which may be presented on these images bleeding through the cortical surface.
Case 1

Right handed 15 year-old-boy with intractable epilepsy performing a verbal "repetition task." The surface rendition beautifully depicts the activation occurring in the posterior third of the right superior temporal gyrus and extending toward supramarginal gyrus and Brodmann's area 7. The areas of activation are better displayed than with conventional 2D MR images.
Case 2

Right handed 11 year-old-girl with intractable epilepsy who had a left frontal resection two years ago for control of seizures. Persistence of the seizures prompted this fMR exam for re-evaluation. The images demonstrated activation obtained from a "Verb Generation Task." The study depicted Broca's area and part of Wernicke's (Brodmann's area 37), which is believed to be a repository for words. A second resection was performed based on these findings. The patient experienced no post-operative aphasia and remains seizure free.
3D Rendering + Orthogonal View
Surface rendering and orthogonal views can be combined in one procedure. This allows us to see activation (or lesions) of the cortex and deep structures of the brain. The bleeding through of activation is obviated. External landmarks of the head and face may also help in surgical navigation.
Surface and orthogonal rendering of the brain is viewed in natural anatomical orientation. This means that the structures appear as if they were under direct sight. For that reason the left hemisphere appears on the right side of the left-top-rostral view, and on the left side on the left-top-posterior view. The fMR image presented here depicts activation of the angular gyrus observed in a right-left laterality decision task. The hemi-axial plane shows the activation placed in the deep portion of the left parietal sulcus.
Case 1
11-year-old right handed boy with intractable epilepsy and left hemiparesis. Patient was mapped for language as part of his work up for epilepsy surgery with a "Semantic Fluency Task."

3D-surface rendering and orthogonal views. The images show activation of Broca's area along pars orbitales, triangularis and opercularis in the left hemisphere. Activation is also observed in visual areas likely related to visual strategies. Activation of the basal ganglia is occasionally seen as in this case. Activation can be localized on one image including the cortex, the sylvian fissure, the calcarine fissure, the lateral ventricles and along the midline.
Case 2
Right handed 11 year-old-girl with persistent intractable epilepsy who had a partial left frontal resection . Patient underwent language mapping with fMR.
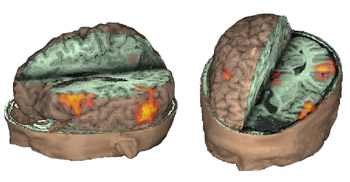
These images complement case 2 presented in "Surface Rendering." Activation is obtained with a "verb generation" task in Wernicke's area not only along the cortical surface but deep along the gyri.
Case 3
13 year old right handed-boy, with temporal lobe epilepsy. A multicystic oligodendroglioma was found in the left temporal lobe (black arrows). Functional MRI was prescribed to map language areas, prior to surgical resection.

A 3D-fMRI depicts the mass in the left temporal pole. The activation was obtained utilizing a "Repetition Task" paradigm (bubbles in yellow, orange, and red). The relationship between the lesion and the speech areas are beautifully displayed.
Case 4
Right handed 19 year-old female volunteer, performing a Stroop-like paradigm. This task involves inhibition, potentially useful in ADHD evaluation.

Activation is located in the cingulate gyrus, right inferior frontal, and supramarginal gyrus (red bubbles). The blue bubble located in the right frontal pole corresponds to inhibited areas. The combination of orthogonal axial and sagittal planes allow simultaneous presentation.
Triple Rendering
The neurosurgeon has a restricted view of the brain through the small window of the craniotomy. Modern neuroimaging can provide anatomy in three dimensions, and a much wider window.
Case 1
27-year-old right handed woman who underwent MRI and MRV to rule out a structural lesion. The patient volunteered to perform a verb generation task.

The image shows the fusion of three different procedures. In gray scale is the volumetric rendition of the brain obtained from the MRI sequence. In blue are depicted the surface veins and sinus of the left hemisphere from the MR-venogram. In yellow and red appears activation obtained from the echo-planar sequence used for functional MRI.
Case 2
17 year-old right handed boy with intractable epilepsy of partial motor type. MRI showed signal abnormality in the left middle frontal gyrus consistent with cortical dysplasia.

MRI of the head with partial exposure of the brain and skull. An axial view located at the superior third of the inferior frontal gyrus demonstrates in red the activation obtained with a verb generation task. The yellow spot represents the lesion and is derived from a fluid attenuated inversion recovery (FLAIR) sequence, and rendered with the rest of images, revealing the relationship between the lesion and the eloquent areas.
Case 3
15 year-old right handed girl with sensory-motor partial seizures involving the left hand since the age of 5. MRI showed a focal signal abnormality in the right postcentral gyrus consistent with a developmental tumor without changes over 2 years.

MRI of the brain appears in gray scale, functional MR activation is in yellow and red, the tumor is purple (light blue arrow), and the veins are blue. The tumor appears located in the post-central gyrus lateral and rostral to the functional activation. The relationship between the tumor and the functional activation was confirmed during awake intraoperative mapping. The venous landmarks provided useful information to the operating surgeon. The patient's tumor was removed without residual monoplegia. The patient had only transient loss of stereognosis and proprioception involving the 3rd, 4th, and 5th fingers, post-operatively.
3D Functional Magnetic Resonance
Conventional MR images are two-dimensional representation of intensities occurring at a given level or slice.
These images may be presented in axial, coronal and sagittal planes.
The most frequent plane used in fMR is the axial plane which shows the localization of structures or activation in a X (right to left) and a Y (anterior to posterior) axes. Since these images are usually obtained in oblique planes it is difficult to know the precise level in the remaining Z (cranio-caudal) axis.
3D MRI scans allow us to present images with a volumetric appearance. These 3D MRI images have proven to be useful to guide surgical resections.
Types of 3D MRI scans
Orthogonal Views
Orthogonal views refer to a set of mutually perpendicular images. This localizes a given region of activation to the three axes that define the volumetric shape of the brain.
Case 1

Adult volunteer generating verbs. On the axial view the exact location of activation in the temporal lobe is difficult to determine. The black lines in the axial view correspond to the location of the coronal and sagittal views. These three views allow us to determine the location of activation in the middle temporal gyrus.
Case 2

Right handed adult male patient with intractable seizures coming from the left temporal pole, performing a language task consisting of listening to a story. No structural lesion was found in this region. A left temporal resection is planned. The orthogonal views permit evaluating of the extent of the language areas and the distance between its anterior border and the temporal pole (orange line). The neurosurgeon may use these findings as a guide to tailor the temporal resection.
Surface Rendering
Surface rendering is a computer post processing method that removes the skin and the skull to allow us to see the brain surface. The anatomy of gyri and sulci are displayed in the same way the neurosurgeon sees the brain. Functional maps can be superimposed on these images. Some activation may take place deep in the sulci which may be presented on these images bleeding through the cortical surface.
Case 1

Right handed 15 year-old-boy with intractable epilepsy performing a verbal "repetition task." The surface rendition beautifully depicts the activation occurring in the posterior third of the right superior temporal gyrus and extending toward supramarginal gyrus and Brodmann's area 7. The areas of activation are better displayed than with conventional 2D MR images.
Case 2

Right handed 11 year-old-girl with intractable epilepsy who had a left frontal resection two years ago for control of seizures. Persistence of the seizures prompted this fMR exam for re-evaluation. The images demonstrated activation obtained from a "Verb Generation Task." The study depicted Broca's area and part of Wernicke's (Brodmann's area 37), which is believed to be a repository for words. A second resection was performed based on these findings. The patient experienced no post-operative aphasia and remains seizure free.
3D Rendering + Orthogonal View
Surface rendering and orthogonal views can be combined in one procedure. This allows us to see activation (or lesions) of the cortex and deep structures of the brain. The bleeding through of activation is obviated. External landmarks of the head and face may also help in surgical navigation.
Surface and orthogonal rendering of the brain is viewed in natural anatomical orientation. This means that the structures appear as if they were under direct sight. For that reason the left hemisphere appears on the right side of the left-top-rostral view, and on the left side on the left-top-posterior view. The fMR image presented here depicts activation of the angular gyrus observed in a right-left laterality decision task. The hemi-axial plane shows the activation placed in the deep portion of the left parietal sulcus.
Case 1
11-year-old right handed boy with intractable epilepsy and left hemiparesis. Patient was mapped for language as part of his work up for epilepsy surgery with a "Semantic Fluency Task."

3D-surface rendering and orthogonal views. The images show activation of Broca's area along pars orbitales, triangularis and opercularis in the left hemisphere. Activation is also observed in visual areas likely related to visual strategies. Activation of the basal ganglia is occasionally seen as in this case. Activation can be localized on one image including the cortex, the sylvian fissure, the calcarine fissure, the lateral ventricles and along the midline.
Case 2
Right handed 11 year-old-girl with persistent intractable epilepsy who had a partial left frontal resection . Patient underwent language mapping with fMR.
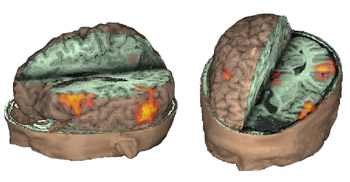
These images complement case 2 presented in "Surface Rendering." Activation is obtained with a "verb generation" task in Wernicke's area not only along the cortical surface but deep along the gyri.
Case 3
13 year old right handed-boy, with temporal lobe epilepsy. A multicystic oligodendroglioma was found in the left temporal lobe (black arrows). Functional MRI was prescribed to map language areas, prior to surgical resection.

A 3D-fMRI depicts the mass in the left temporal pole. The activation was obtained utilizing a "Repetition Task" paradigm (bubbles in yellow, orange, and red). The relationship between the lesion and the speech areas are beautifully displayed.
Case 4
Right handed 19 year-old female volunteer, performing a Stroop-like paradigm. This task involves inhibition, potentially useful in ADHD evaluation.

Activation is located in the cingulate gyrus, right inferior frontal, and supramarginal gyrus (red bubbles). The blue bubble located in the right frontal pole corresponds to inhibited areas. The combination of orthogonal axial and sagittal planes allow simultaneous presentation.
Triple Rendering
The neurosurgeon has a restricted view of the brain through the small window of the craniotomy. Modern neuroimaging can provide anatomy in three dimensions, and a much wider window.
Case 1
27-year-old right handed woman who underwent MRI and MRV to rule out a structural lesion. The patient volunteered to perform a verb generation task.

The image shows the fusion of three different procedures. In gray scale is the volumetric rendition of the brain obtained from the MRI sequence. In blue are depicted the surface veins and sinus of the left hemisphere from the MR-venogram. In yellow and red appears activation obtained from the echo-planar sequence used for functional MRI.
Case 2
17 year-old right handed boy with intractable epilepsy of partial motor type. MRI showed signal abnormality in the left middle frontal gyrus consistent with cortical dysplasia.

MRI of the head with partial exposure of the brain and skull. An axial view located at the superior third of the inferior frontal gyrus demonstrates in red the activation obtained with a verb generation task. The yellow spot represents the lesion and is derived from a fluid attenuated inversion recovery (FLAIR) sequence, and rendered with the rest of images, revealing the relationship between the lesion and the eloquent areas.
Case 3
15 year-old right handed girl with sensory-motor partial seizures involving the left hand since the age of 5. MRI showed a focal signal abnormality in the right postcentral gyrus consistent with a developmental tumor without changes over 2 years.

MRI of the brain appears in gray scale, functional MR activation is in yellow and red, the tumor is purple (light blue arrow), and the veins are blue. The tumor appears located in the post-central gyrus lateral and rostral to the functional activation. The relationship between the tumor and the functional activation was confirmed during awake intraoperative mapping. The venous landmarks provided useful information to the operating surgeon. The patient's tumor was removed without residual monoplegia. The patient had only transient loss of stereognosis and proprioception involving the 3rd, 4th, and 5th fingers, post-operatively.
3D Functional Magnetic Resonance
Conventional MR images are two-dimensional representation of intensities occurring at a given level or slice.
These images may be presented in axial, coronal and sagittal planes.
The most frequent plane used in fMR is the axial plane which shows the localization of structures or activation in a X (right to left) and a Y (anterior to posterior) axes. Since these images are usually obtained in oblique planes it is difficult to know the precise level in the remaining Z (cranio-caudal) axis.
3D MRI scans allow us to present images with a volumetric appearance. These 3D MRI images have proven to be useful to guide surgical resections.
Types of 3D MRI scans
Orthogonal Views
Orthogonal views refer to a set of mutually perpendicular images. This localizes a given region of activation to the three axes that define the volumetric shape of the brain.
Case 1

Adult volunteer generating verbs. On the axial view the exact location of activation in the temporal lobe is difficult to determine. The black lines in the axial view correspond to the location of the coronal and sagittal views. These three views allow us to determine the location of activation in the middle temporal gyrus.
Case 2

Right handed adult male patient with intractable seizures coming from the left temporal pole, performing a language task consisting of listening to a story. No structural lesion was found in this region. A left temporal resection is planned. The orthogonal views permit evaluating of the extent of the language areas and the distance between its anterior border and the temporal pole (orange line). The neurosurgeon may use these findings as a guide to tailor the temporal resection.
Surface Rendering
Surface rendering is a computer post processing method that removes the skin and the skull to allow us to see the brain surface. The anatomy of gyri and sulci are displayed in the same way the neurosurgeon sees the brain. Functional maps can be superimposed on these images. Some activation may take place deep in the sulci which may be presented on these images bleeding through the cortical surface.
Case 1

Right handed 15 year-old-boy with intractable epilepsy performing a verbal "repetition task." The surface rendition beautifully depicts the activation occurring in the posterior third of the right superior temporal gyrus and extending toward supramarginal gyrus and Brodmann's area 7. The areas of activation are better displayed than with conventional 2D MR images.
Case 2

Right handed 11 year-old-girl with intractable epilepsy who had a left frontal resection two years ago for control of seizures. Persistence of the seizures prompted this fMR exam for re-evaluation. The images demonstrated activation obtained from a "Verb Generation Task." The study depicted Broca's area and part of Wernicke's (Brodmann's area 37), which is believed to be a repository for words. A second resection was performed based on these findings. The patient experienced no post-operative aphasia and remains seizure free.
3D Rendering + Orthogonal View
Surface rendering and orthogonal views can be combined in one procedure. This allows us to see activation (or lesions) of the cortex and deep structures of the brain. The bleeding through of activation is obviated. External landmarks of the head and face may also help in surgical navigation.
Surface and orthogonal rendering of the brain is viewed in natural anatomical orientation. This means that the structures appear as if they were under direct sight. For that reason the left hemisphere appears on the right side of the left-top-rostral view, and on the left side on the left-top-posterior view. The fMR image presented here depicts activation of the angular gyrus observed in a right-left laterality decision task. The hemi-axial plane shows the activation placed in the deep portion of the left parietal sulcus.
Case 1
11-year-old right handed boy with intractable epilepsy and left hemiparesis. Patient was mapped for language as part of his work up for epilepsy surgery with a "Semantic Fluency Task."

3D-surface rendering and orthogonal views. The images show activation of Broca's area along pars orbitales, triangularis and opercularis in the left hemisphere. Activation is also observed in visual areas likely related to visual strategies. Activation of the basal ganglia is occasionally seen as in this case. Activation can be localized on one image including the cortex, the sylvian fissure, the calcarine fissure, the lateral ventricles and along the midline.
Case 2
Right handed 11 year-old-girl with persistent intractable epilepsy who had a partial left frontal resection . Patient underwent language mapping with fMR.
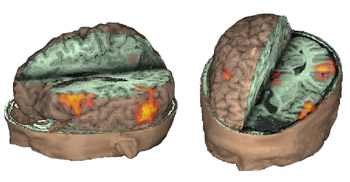
These images complement case 2 presented in "Surface Rendering." Activation is obtained with a "verb generation" task in Wernicke's area not only along the cortical surface but deep along the gyri.
Case 3
13 year old right handed-boy, with temporal lobe epilepsy. A multicystic oligodendroglioma was found in the left temporal lobe (black arrows). Functional MRI was prescribed to map language areas, prior to surgical resection.

A 3D-fMRI depicts the mass in the left temporal pole. The activation was obtained utilizing a "Repetition Task" paradigm (bubbles in yellow, orange, and red). The relationship between the lesion and the speech areas are beautifully displayed.
Case 4
Right handed 19 year-old female volunteer, performing a Stroop-like paradigm. This task involves inhibition, potentially useful in ADHD evaluation.

Activation is located in the cingulate gyrus, right inferior frontal, and supramarginal gyrus (red bubbles). The blue bubble located in the right frontal pole corresponds to inhibited areas. The combination of orthogonal axial and sagittal planes allow simultaneous presentation.
Triple Rendering
The neurosurgeon has a restricted view of the brain through the small window of the craniotomy. Modern neuroimaging can provide anatomy in three dimensions, and a much wider window.
Case 1
27-year-old right handed woman who underwent MRI and MRV to rule out a structural lesion. The patient volunteered to perform a verb generation task.

The image shows the fusion of three different procedures. In gray scale is the volumetric rendition of the brain obtained from the MRI sequence. In blue are depicted the surface veins and sinus of the left hemisphere from the MR-venogram. In yellow and red appears activation obtained from the echo-planar sequence used for functional MRI.
Case 2
17 year-old right handed boy with intractable epilepsy of partial motor type. MRI showed signal abnormality in the left middle frontal gyrus consistent with cortical dysplasia.

MRI of the head with partial exposure of the brain and skull. An axial view located at the superior third of the inferior frontal gyrus demonstrates in red the activation obtained with a verb generation task. The yellow spot represents the lesion and is derived from a fluid attenuated inversion recovery (FLAIR) sequence, and rendered with the rest of images, revealing the relationship between the lesion and the eloquent areas.
Case 3
15 year-old right handed girl with sensory-motor partial seizures involving the left hand since the age of 5. MRI showed a focal signal abnormality in the right postcentral gyrus consistent with a developmental tumor without changes over 2 years.

MRI of the brain appears in gray scale, functional MR activation is in yellow and red, the tumor is purple (light blue arrow), and the veins are blue. The tumor appears located in the post-central gyrus lateral and rostral to the functional activation. The relationship between the tumor and the functional activation was confirmed during awake intraoperative mapping. The venous landmarks provided useful information to the operating surgeon. The patient's tumor was removed without residual monoplegia. The patient had only transient loss of stereognosis and proprioception involving the 3rd, 4th, and 5th fingers, post-operatively.
fMRI Studies in Sedated Children
Case 1
| Patient |
2 month-old-girl with hydrocephalus |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words
OFF: Nothing. Patient sedated with chloral hydrate |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0007 |
3.4 |
|
| Activation |
There is bilateral activation of the precentral gyri and the right superior temporal gyrus. The activation of the motor strip occurs at the level of oral-facial representation. This is supposed to be related with the habituation-dishabituation of high-amplitude sucking in response to lingustic stimuli. This response is of great importance in the preservation of our species. |
Case 2
| Patient |
18 month-old-boy with mild cerebral palsy |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words and sounds
OFF: Nothing. Patient sedated with propofol |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0005 |
3.2 |
|
| Activation |
Activation of auditory areas are well depicted. There is bithalamic activation. The strong activation of the right parasagital frontal lobe is not well understood. |
Case 3
| Patient |
4 year-old-boy with autism |
| Paradigm |
ON: Presentation of flashing lights at 8 Hz, using special goggles
OFF: Nothing. Patient sedated with nembutal |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.000002 |
4.0 |
|
| Activation |
Coronal cuts. The colored areas in the figure were obtained subtracting ON from OFF. Thus, the result shows "deactivation", which represent hyper extraction of oxygen occurring in the primary visual areas (V1). This finding is consistently found in young children either awake or under sedation. |
Case 4
fMRI Studies in Sedated Children
Case 1
| Patient |
2 month-old-girl with hydrocephalus |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words
OFF: Nothing. Patient sedated with chloral hydrate |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0007 |
3.4 |
|
| Activation |
There is bilateral activation of the precentral gyri and the right superior temporal gyrus. The activation of the motor strip occurs at the level of oral-facial representation. This is supposed to be related with the habituation-dishabituation of high-amplitude sucking in response to lingustic stimuli. This response is of great importance in the preservation of our species. |
Case 2
| Patient |
18 month-old-boy with mild cerebral palsy |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words and sounds
OFF: Nothing. Patient sedated with propofol |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0005 |
3.2 |
|
| Activation |
Activation of auditory areas are well depicted. There is bithalamic activation. The strong activation of the right parasagital frontal lobe is not well understood. |
Case 3
| Patient |
4 year-old-boy with autism |
| Paradigm |
ON: Presentation of flashing lights at 8 Hz, using special goggles
OFF: Nothing. Patient sedated with nembutal |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.000002 |
4.0 |
|
| Activation |
Coronal cuts. The colored areas in the figure were obtained subtracting ON from OFF. Thus, the result shows "deactivation", which represent hyper extraction of oxygen occurring in the primary visual areas (V1). This finding is consistently found in young children either awake or under sedation. |
Case 4
fMRI Studies in Sedated Children
Case 1
| Patient |
2 month-old-girl with hydrocephalus |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words
OFF: Nothing. Patient sedated with chloral hydrate |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0007 |
3.4 |
|
| Activation |
There is bilateral activation of the precentral gyri and the right superior temporal gyrus. The activation of the motor strip occurs at the level of oral-facial representation. This is supposed to be related with the habituation-dishabituation of high-amplitude sucking in response to lingustic stimuli. This response is of great importance in the preservation of our species. |
Case 2
| Patient |
18 month-old-boy with mild cerebral palsy |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words and sounds
OFF: Nothing. Patient sedated with propofol |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0005 |
3.2 |
|
| Activation |
Activation of auditory areas are well depicted. There is bithalamic activation. The strong activation of the right parasagital frontal lobe is not well understood. |
Case 3
| Patient |
4 year-old-boy with autism |
| Paradigm |
ON: Presentation of flashing lights at 8 Hz, using special goggles
OFF: Nothing. Patient sedated with nembutal |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.000002 |
4.0 |
|
| Activation |
Coronal cuts. The colored areas in the figure were obtained subtracting ON from OFF. Thus, the result shows "deactivation", which represent hyper extraction of oxygen occurring in the primary visual areas (V1). This finding is consistently found in young children either awake or under sedation. |
Case 4
fMRI Studies in Sedated Children
Case 1
| Patient |
2 month-old-girl with hydrocephalus |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words
OFF: Nothing. Patient sedated with chloral hydrate |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0007 |
3.4 |
|
| Activation |
There is bilateral activation of the precentral gyri and the right superior temporal gyrus. The activation of the motor strip occurs at the level of oral-facial representation. This is supposed to be related with the habituation-dishabituation of high-amplitude sucking in response to lingustic stimuli. This response is of great importance in the preservation of our species. |
Case 2
| Patient |
18 month-old-boy with mild cerebral palsy |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words and sounds
OFF: Nothing. Patient sedated with propofol |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0005 |
3.2 |
|
| Activation |
Activation of auditory areas are well depicted. There is bithalamic activation. The strong activation of the right parasagital frontal lobe is not well understood. |
Case 3
| Patient |
4 year-old-boy with autism |
| Paradigm |
ON: Presentation of flashing lights at 8 Hz, using special goggles
OFF: Nothing. Patient sedated with nembutal |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.000002 |
4.0 |
|
| Activation |
Coronal cuts. The colored areas in the figure were obtained subtracting ON from OFF. Thus, the result shows "deactivation", which represent hyper extraction of oxygen occurring in the primary visual areas (V1). This finding is consistently found in young children either awake or under sedation. |
Case 4
fMRI Studies in Sedated Children
Case 1
| Patient |
2 month-old-girl with hydrocephalus |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words
OFF: Nothing. Patient sedated with chloral hydrate |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0007 |
3.4 |
|
| Activation |
There is bilateral activation of the precentral gyri and the right superior temporal gyrus. The activation of the motor strip occurs at the level of oral-facial representation. This is supposed to be related with the habituation-dishabituation of high-amplitude sucking in response to lingustic stimuli. This response is of great importance in the preservation of our species. |
Case 2
| Patient |
18 month-old-boy with mild cerebral palsy |
| Paradigm |
ON: Presentation of mother's voice, pre-recorded, using familiar words and sounds
OFF: Nothing. Patient sedated with propofol |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0005 |
3.2 |
|
| Activation |
Activation of auditory areas are well depicted. There is bithalamic activation. The strong activation of the right parasagital frontal lobe is not well understood. |
Case 3
| Patient |
4 year-old-boy with autism |
| Paradigm |
ON: Presentation of flashing lights at 8 Hz, using special goggles
OFF: Nothing. Patient sedated with nembutal |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.000002 |
4.0 |
|
| Activation |
Coronal cuts. The colored areas in the figure were obtained subtracting ON from OFF. Thus, the result shows "deactivation", which represent hyper extraction of oxygen occurring in the primary visual areas (V1). This finding is consistently found in young children either awake or under sedation. |
Case 4
fMRI Language Mapping
Please follow the links below to learn more about Language Mapping.
Auditory Verbal Activation
Passive listening to a story
Activation

Left supramarginal gyrus
Left > Right Heschl's gyri
Auditory Non-Verbal Activation
Passive hearing of plain music (Same technical settings)

Activation
Right > left Heschl's gyri
Phonological Fluency
| Subject |
Right handed, 37 year-old woman |
| Paradigm |
ON: Retrieving words starting with a given letter
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Images |
  |
| Activation |
This paradigm elicits activation of the superior aspect of Broca's and Brodman's 37 areas. Some activation appears in parasagital parietal areas. The color in the left pterional fossa is due to vascular inflow. |
Semantic Fluency
| Subject |
Right handed, 25 year-old woman |
| Paradigm |
ON: Retrieving words within a given category
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.00005 |
4.2 |
|
| Images |
 |
| Activation |
The left hemisphere shows predominant activation. The following areas were activated: Broca's, left posterior portion of middle and inferior temporal gyri (Brodman's 37), left parietal and left premotor strip. Wide activation is seen in the inferior aspect of the occipital lobes. The main activation on the right is located in the inferior aspect of the frontal lobe (Brodman's 11), a finding consistently seen in this paradigm. |
Fluency of Verbs
| Subject |
Right handed, 24 year-old woman |
| Paradigm |
ON: Generate verbs related to nouns (objects)
OFF: Count the letters of presented words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Broca's area and left SMA are depicted. Some activation appears in the left hippocampal formation and visual areas. This last activation could be explained as the effect of picturing the objects given during the "ON" condition. There is also activation in the right cerebellum and left inferior temporal gyrus.
|
Automatic Speech
| Subject |
25 year-old woman. Right-handed Volunteer |
| Paradigm |
ON: Saying mentally the pledge of allegiance
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0002 |
3.7 |
|
| Images |
 |
| Activation |
Oral and facial motor strip, greater on the right. Right parietal lobe. No activation is seen in Broca's area |
Verbal Comprehension
| Subject |
Right-handed volunteer, 32 year-old-man |
| Paradigm |
ON: Listening to a story
OFF: Concentrate on the back ground noise |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Left hemisphere activation is clearly greater. The activation is in the following areas: Broca's (image 5), Wernike's (images 4 and 5), left supramarginal gyrus (heteromodal associative area, in image 5), left motor and premotor strip. The primary auditory areas are also activated predominantly on the left. |
Studies in Late Bilinguals
| Subject |
Right handed 34 year-old-woman. Native language: Spanish
|
| Paradigm |
Type: Verbal fluency task
ON: Retrieve verbs related to presented nouns
OFF Spell given words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
Spanish

|
English

|
|
| Activation |
There is activation of Broca's area in both languages. The right thalamic activation is noted only in the second language. There is also greater activation of the right inferior frontal gyrus in the second language than in the mother language. SMA is more pronounced on the right in both languages. |
fMRI Language Mapping
Please follow the links below to learn more about Language Mapping.
Auditory Verbal Activation
Passive listening to a story
Activation

Left supramarginal gyrus
Left > Right Heschl's gyri
Auditory Non-Verbal Activation
Passive hearing of plain music (Same technical settings)

Activation
Right > left Heschl's gyri
Phonological Fluency
| Subject |
Right handed, 37 year-old woman |
| Paradigm |
ON: Retrieving words starting with a given letter
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Images |
  |
| Activation |
This paradigm elicits activation of the superior aspect of Broca's and Brodman's 37 areas. Some activation appears in parasagital parietal areas. The color in the left pterional fossa is due to vascular inflow. |
Semantic Fluency
| Subject |
Right handed, 25 year-old woman |
| Paradigm |
ON: Retrieving words within a given category
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.00005 |
4.2 |
|
| Images |
 |
| Activation |
The left hemisphere shows predominant activation. The following areas were activated: Broca's, left posterior portion of middle and inferior temporal gyri (Brodman's 37), left parietal and left premotor strip. Wide activation is seen in the inferior aspect of the occipital lobes. The main activation on the right is located in the inferior aspect of the frontal lobe (Brodman's 11), a finding consistently seen in this paradigm. |
Fluency of Verbs
| Subject |
Right handed, 24 year-old woman |
| Paradigm |
ON: Generate verbs related to nouns (objects)
OFF: Count the letters of presented words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Broca's area and left SMA are depicted. Some activation appears in the left hippocampal formation and visual areas. This last activation could be explained as the effect of picturing the objects given during the "ON" condition. There is also activation in the right cerebellum and left inferior temporal gyrus.
|
Automatic Speech
| Subject |
25 year-old woman. Right-handed Volunteer |
| Paradigm |
ON: Saying mentally the pledge of allegiance
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0002 |
3.7 |
|
| Images |
 |
| Activation |
Oral and facial motor strip, greater on the right. Right parietal lobe. No activation is seen in Broca's area |
Verbal Comprehension
| Subject |
Right-handed volunteer, 32 year-old-man |
| Paradigm |
ON: Listening to a story
OFF: Concentrate on the back ground noise |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Left hemisphere activation is clearly greater. The activation is in the following areas: Broca's (image 5), Wernike's (images 4 and 5), left supramarginal gyrus (heteromodal associative area, in image 5), left motor and premotor strip. The primary auditory areas are also activated predominantly on the left. |
Studies in Late Bilinguals
| Subject |
Right handed 34 year-old-woman. Native language: Spanish
|
| Paradigm |
Type: Verbal fluency task
ON: Retrieve verbs related to presented nouns
OFF Spell given words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
Spanish

|
English

|
|
| Activation |
There is activation of Broca's area in both languages. The right thalamic activation is noted only in the second language. There is also greater activation of the right inferior frontal gyrus in the second language than in the mother language. SMA is more pronounced on the right in both languages. |
fMRI Language Mapping
Please follow the links below to learn more about Language Mapping.
Auditory Verbal Activation
Passive listening to a story
Activation

Left supramarginal gyrus
Left > Right Heschl's gyri
Auditory Non-Verbal Activation
Passive hearing of plain music (Same technical settings)

Activation
Right > left Heschl's gyri
Phonological Fluency
| Subject |
Right handed, 37 year-old woman |
| Paradigm |
ON: Retrieving words starting with a given letter
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Images |
  |
| Activation |
This paradigm elicits activation of the superior aspect of Broca's and Brodman's 37 areas. Some activation appears in parasagital parietal areas. The color in the left pterional fossa is due to vascular inflow. |
Semantic Fluency
| Subject |
Right handed, 25 year-old woman |
| Paradigm |
ON: Retrieving words within a given category
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.00005 |
4.2 |
|
| Images |
 |
| Activation |
The left hemisphere shows predominant activation. The following areas were activated: Broca's, left posterior portion of middle and inferior temporal gyri (Brodman's 37), left parietal and left premotor strip. Wide activation is seen in the inferior aspect of the occipital lobes. The main activation on the right is located in the inferior aspect of the frontal lobe (Brodman's 11), a finding consistently seen in this paradigm. |
Fluency of Verbs
| Subject |
Right handed, 24 year-old woman |
| Paradigm |
ON: Generate verbs related to nouns (objects)
OFF: Count the letters of presented words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Broca's area and left SMA are depicted. Some activation appears in the left hippocampal formation and visual areas. This last activation could be explained as the effect of picturing the objects given during the "ON" condition. There is also activation in the right cerebellum and left inferior temporal gyrus.
|
Automatic Speech
| Subject |
25 year-old woman. Right-handed Volunteer |
| Paradigm |
ON: Saying mentally the pledge of allegiance
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0002 |
3.7 |
|
| Images |
 |
| Activation |
Oral and facial motor strip, greater on the right. Right parietal lobe. No activation is seen in Broca's area |
Verbal Comprehension
| Subject |
Right-handed volunteer, 32 year-old-man |
| Paradigm |
ON: Listening to a story
OFF: Concentrate on the back ground noise |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Left hemisphere activation is clearly greater. The activation is in the following areas: Broca's (image 5), Wernike's (images 4 and 5), left supramarginal gyrus (heteromodal associative area, in image 5), left motor and premotor strip. The primary auditory areas are also activated predominantly on the left. |
Studies in Late Bilinguals
| Subject |
Right handed 34 year-old-woman. Native language: Spanish
|
| Paradigm |
Type: Verbal fluency task
ON: Retrieve verbs related to presented nouns
OFF Spell given words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
Spanish

|
English

|
|
| Activation |
There is activation of Broca's area in both languages. The right thalamic activation is noted only in the second language. There is also greater activation of the right inferior frontal gyrus in the second language than in the mother language. SMA is more pronounced on the right in both languages. |
fMRI Language Mapping
Please follow the links below to learn more about Language Mapping.
Auditory Verbal Activation
Passive listening to a story
Activation

Left supramarginal gyrus
Left > Right Heschl's gyri
Auditory Non-Verbal Activation
Passive hearing of plain music (Same technical settings)

Activation
Right > left Heschl's gyri
Phonological Fluency
| Subject |
Right handed, 37 year-old woman |
| Paradigm |
ON: Retrieving words starting with a given letter
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Images |
  |
| Activation |
This paradigm elicits activation of the superior aspect of Broca's and Brodman's 37 areas. Some activation appears in parasagital parietal areas. The color in the left pterional fossa is due to vascular inflow. |
Semantic Fluency
| Subject |
Right handed, 25 year-old woman |
| Paradigm |
ON: Retrieving words within a given category
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.00005 |
4.2 |
|
| Images |
 |
| Activation |
The left hemisphere shows predominant activation. The following areas were activated: Broca's, left posterior portion of middle and inferior temporal gyri (Brodman's 37), left parietal and left premotor strip. Wide activation is seen in the inferior aspect of the occipital lobes. The main activation on the right is located in the inferior aspect of the frontal lobe (Brodman's 11), a finding consistently seen in this paradigm. |
Fluency of Verbs
| Subject |
Right handed, 24 year-old woman |
| Paradigm |
ON: Generate verbs related to nouns (objects)
OFF: Count the letters of presented words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Broca's area and left SMA are depicted. Some activation appears in the left hippocampal formation and visual areas. This last activation could be explained as the effect of picturing the objects given during the "ON" condition. There is also activation in the right cerebellum and left inferior temporal gyrus.
|
Automatic Speech
| Subject |
25 year-old woman. Right-handed Volunteer |
| Paradigm |
ON: Saying mentally the pledge of allegiance
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0002 |
3.7 |
|
| Images |
 |
| Activation |
Oral and facial motor strip, greater on the right. Right parietal lobe. No activation is seen in Broca's area |
Verbal Comprehension
| Subject |
Right-handed volunteer, 32 year-old-man |
| Paradigm |
ON: Listening to a story
OFF: Concentrate on the back ground noise |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Left hemisphere activation is clearly greater. The activation is in the following areas: Broca's (image 5), Wernike's (images 4 and 5), left supramarginal gyrus (heteromodal associative area, in image 5), left motor and premotor strip. The primary auditory areas are also activated predominantly on the left. |
Studies in Late Bilinguals
| Subject |
Right handed 34 year-old-woman. Native language: Spanish
|
| Paradigm |
Type: Verbal fluency task
ON: Retrieve verbs related to presented nouns
OFF Spell given words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
Spanish

|
English

|
|
| Activation |
There is activation of Broca's area in both languages. The right thalamic activation is noted only in the second language. There is also greater activation of the right inferior frontal gyrus in the second language than in the mother language. SMA is more pronounced on the right in both languages. |
fMRI Language Mapping
Please follow the links below to learn more about Language Mapping.
Auditory Verbal Activation
Passive listening to a story
Activation

Left supramarginal gyrus
Left > Right Heschl's gyri
Auditory Non-Verbal Activation
Passive hearing of plain music (Same technical settings)

Activation
Right > left Heschl's gyri
Phonological Fluency
| Subject |
Right handed, 37 year-old woman |
| Paradigm |
ON: Retrieving words starting with a given letter
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| Correlation coeficient |
0.0001 |
N/A |
|
| Images |
  |
| Activation |
This paradigm elicits activation of the superior aspect of Broca's and Brodman's 37 areas. Some activation appears in parasagital parietal areas. The color in the left pterional fossa is due to vascular inflow. |
Semantic Fluency
| Subject |
Right handed, 25 year-old woman |
| Paradigm |
ON: Retrieving words within a given category
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.00005 |
4.2 |
|
| Images |
 |
| Activation |
The left hemisphere shows predominant activation. The following areas were activated: Broca's, left posterior portion of middle and inferior temporal gyri (Brodman's 37), left parietal and left premotor strip. Wide activation is seen in the inferior aspect of the occipital lobes. The main activation on the right is located in the inferior aspect of the frontal lobe (Brodman's 11), a finding consistently seen in this paradigm. |
Fluency of Verbs
| Subject |
Right handed, 24 year-old woman |
| Paradigm |
ON: Generate verbs related to nouns (objects)
OFF: Count the letters of presented words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Broca's area and left SMA are depicted. Some activation appears in the left hippocampal formation and visual areas. This last activation could be explained as the effect of picturing the objects given during the "ON" condition. There is also activation in the right cerebellum and left inferior temporal gyrus.
|
Automatic Speech
| Subject |
25 year-old woman. Right-handed Volunteer |
| Paradigm |
ON: Saying mentally the pledge of allegiance
OFF: Think of a dark sky |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0002 |
3.7 |
|
| Images |
 |
| Activation |
Oral and facial motor strip, greater on the right. Right parietal lobe. No activation is seen in Broca's area |
Verbal Comprehension
| Subject |
Right-handed volunteer, 32 year-old-man |
| Paradigm |
ON: Listening to a story
OFF: Concentrate on the back ground noise |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
 |
| Activation |
Left hemisphere activation is clearly greater. The activation is in the following areas: Broca's (image 5), Wernike's (images 4 and 5), left supramarginal gyrus (heteromodal associative area, in image 5), left motor and premotor strip. The primary auditory areas are also activated predominantly on the left. |
Studies in Late Bilinguals
| Subject |
Right handed 34 year-old-woman. Native language: Spanish
|
| Paradigm |
Type: Verbal fluency task
ON: Retrieve verbs related to presented nouns
OFF Spell given words |
| Statistics |
| Statistical method |
P Value |
Z score |
| T-Test |
0.0001 |
3.8 |
|
| Images |
Spanish

|
English

|
|
| Activation |
There is activation of Broca's area in both languages. The right thalamic activation is noted only in the second language. There is also greater activation of the right inferior frontal gyrus in the second language than in the mother language. SMA is more pronounced on the right in both languages. |
Understanding the process
Limb restoration is a gradual process that helps to restore a patient's bone and soft tissue to normal alignment, length and function. While there are many reasons a patient would choose to have this type of procedure, the primary indications include trauma, congenital deformities and bone or joint infection.
Your orthopedis uses ILIZAROV surgery to provide limb restoration. This remarkable technique uses a device called the TAYLOR SPATIAL FRAME TM to take advantage of the body's natural ability to grow healthy new bone tissue.
There are two main phases to the ILIZAROV procedure: limb lengthening/correction and consolidation.

ILIZAROV lengthening/correction refers to the period of time it takes to 'grow the bone.' This initial phase begins after the surgeon cuts the bone and attaches the TAYLOR SPATIAL FRAME fixator. During this time, you will be working with the physician and your team to make gradual adjustments to the device, which increases the gap between the bone segments, adding 'length' to the total limb. Over a period of months, new bone tissue will grow in the gap, ultimately hardening the area between the segments of the original bone.
When your surgeon is satisfied with the length and position of the new bone, the consolidation phase begins. During this phase, the bone tissue matures and becomes solid. You still wear the TAYLOR SPATIAL FRAME fixator, but you will not make adjustments. The consolidation phase is the longest part of the ILIZAROV process.
◊ Trademark of Smith & Nephew
Understanding the process
Limb restoration is a gradual process that helps to restore a patient's bone and soft tissue to normal alignment, length and function. While there are many reasons a patient would choose to have this type of procedure, the primary indications include trauma, congenital deformities and bone or joint infection.
Your orthopedis uses ILIZAROV surgery to provide limb restoration. This remarkable technique uses a device called the TAYLOR SPATIAL FRAME TM to take advantage of the body's natural ability to grow healthy new bone tissue.
There are two main phases to the ILIZAROV procedure: limb lengthening/correction and consolidation.

ILIZAROV lengthening/correction refers to the period of time it takes to 'grow the bone.' This initial phase begins after the surgeon cuts the bone and attaches the TAYLOR SPATIAL FRAME fixator. During this time, you will be working with the physician and your team to make gradual adjustments to the device, which increases the gap between the bone segments, adding 'length' to the total limb. Over a period of months, new bone tissue will grow in the gap, ultimately hardening the area between the segments of the original bone.
When your surgeon is satisfied with the length and position of the new bone, the consolidation phase begins. During this phase, the bone tissue matures and becomes solid. You still wear the TAYLOR SPATIAL FRAME fixator, but you will not make adjustments. The consolidation phase is the longest part of the ILIZAROV process.
◊ Trademark of Smith & Nephew
Conditions treated
There are many different pediatric orthopedic conditions where use of the TAYLOR SPATIAL FRAME◊ device is prescribed. The external fixator can be used to correct arm and leg length discrepancies and deformities including:
- Injury and trauma including growth plate fractures, malunion (where the bones heal crookedly), non-union (where the bone doesn't heal together), shortening and deformity due to bone loss.
- Congenital limb length discrepancies. These conditions are associated with many birth defects and deformities including a short femur (thigh bone), otherwise known as fibular hemimelia. Pseudoarthritis in which the bone fails to fuse together such as in a fracture healing site. And hemiatrophy, where the bones of one side of a child's body may grow smaller than the other side.
- Short stature including achondroplasia and other skeletal dysplasias and Constitutional Short Stature. External fixators can be effective in treating limb length discrepancies linked to dwarfism. Treatment may be appropriate in some cases in order to allow the patient to function more independently.
- Infection involving the bone (osteomyelitis) and joint (septic or infectious arthritis). Treatment of bone infection often requires removal of bone segment which may result in angular deformities and limb length discrepancies.
- Developmental causes which are related to the slowing of growth and limb deformities caused by illnesses such as Blount's Disease, which typically affects the bone development of overweight toddlers and adolescents.
- External fixators are also used in the treatment of pediatric hip disorders such as Developmental Coxa Vara (DCV), Perthes Disease and Slipped Capital Femoral Epiphyses.
- Joint stiffness following injury, infection or other causes can sometimes be addressed by controlled joint distraction (arthodiatasis), with the use of external fixators.
- Clubfoot (talipes equinovarus – TEV), a congenital defect where bones of the foot and ankle are not in alignment can be corrected with external fixation.
- Bone fractures in conjunction with soft tissue damage such as burns can be addressed with external fixation because it is a minimally-invasive external device that allows for skin tissue healing while correcting bone fractures at the same time.

◊ Trademark of Smith & Nephew
Conditions treated
There are many different pediatric orthopedic conditions where use of the TAYLOR SPATIAL FRAME◊ device is prescribed. The external fixator can be used to correct arm and leg length discrepancies and deformities including:
- Injury and trauma including growth plate fractures, malunion (where the bones heal crookedly), non-union (where the bone doesn't heal together), shortening and deformity due to bone loss.
- Congenital limb length discrepancies. These conditions are associated with many birth defects and deformities including a short femur (thigh bone), otherwise known as fibular hemimelia. Pseudoarthritis in which the bone fails to fuse together such as in a fracture healing site. And hemiatrophy, where the bones of one side of a child's body may grow smaller than the other side.
- Short stature including achondroplasia and other skeletal dysplasias and Constitutional Short Stature. External fixators can be effective in treating limb length discrepancies linked to dwarfism. Treatment may be appropriate in some cases in order to allow the patient to function more independently.
- Infection involving the bone (osteomyelitis) and joint (septic or infectious arthritis). Treatment of bone infection often requires removal of bone segment which may result in angular deformities and limb length discrepancies.
- Developmental causes which are related to the slowing of growth and limb deformities caused by illnesses such as Blount's Disease, which typically affects the bone development of overweight toddlers and adolescents.
- External fixators are also used in the treatment of pediatric hip disorders such as Developmental Coxa Vara (DCV), Perthes Disease and Slipped Capital Femoral Epiphyses.
- Joint stiffness following injury, infection or other causes can sometimes be addressed by controlled joint distraction (arthodiatasis), with the use of external fixators.
- Clubfoot (talipes equinovarus – TEV), a congenital defect where bones of the foot and ankle are not in alignment can be corrected with external fixation.
- Bone fractures in conjunction with soft tissue damage such as burns can be addressed with external fixation because it is a minimally-invasive external device that allows for skin tissue healing while correcting bone fractures at the same time.

◊ Trademark of Smith & Nephew
What is the TAYLOR SPATIAL FRAME- External Fixator?
The TAYLOR SPATIAL FRAME fixator is an external fixation device for limb correction, lengthening and/or straightening that is based on the ILIZAROV method. This ILIZAROV apparatus takes advantage of the body's natural ability to grow healthy new bone tissue and gives the surgeon the ability to accurately move bones to their correct anatomic alignment.
The TAYLOR SPATIAL FRAME device fits around your limb and is attached to the bone with pins or wires that extend from the rings, through the skin and bone to the other side.
The TAYLOR SPATIAL FRAME device is a circular, metal frame with two rings that connect with six telescopic struts that can be independently lengthened or shortened relative to the rest of the frame. This allows for six different axes of movement, which gives the TAYLOR SPATIAL FRAME device the ability to correct even the most difficult congenital deformities and trauma cases.

When using the TAYLOR SPATIAL FRAME device, your surgeon inputs information about your original bone deformity into an advanced web-based computer application. This information is then interpreted by the software and a day-by-day treatment plan is created. The software also creates an image of your deformity on screen and shows how the bones should be moving each day, until the bones are completely set in proper alignment.
You then make daily adjustments to the struts, depending on your prescribed course of treatment. As the adjustments are made, the rings of the external fixation device are repositioned with respect to each other, moving bones in the directions necessary for treatment.
Your surgeon is able to make a side-by-side comparison of current X-Rays and the projected plan of treatment graphics created by the TAYLOR SPATIAL FRAME device software. This comparison ensures that your bones are healing in the correct alignment and at the appropriate pace.
The TAYLOR SPATIAL FRAME External Fixator is a winner of the Medical Device Excellence Award.
◊ Trademark of Smith & Nephew
What is the TAYLOR SPATIAL FRAME- External Fixator?
The TAYLOR SPATIAL FRAME fixator is an external fixation device for limb correction, lengthening and/or straightening that is based on the ILIZAROV method. This ILIZAROV apparatus takes advantage of the body's natural ability to grow healthy new bone tissue and gives the surgeon the ability to accurately move bones to their correct anatomic alignment.
The TAYLOR SPATIAL FRAME device fits around your limb and is attached to the bone with pins or wires that extend from the rings, through the skin and bone to the other side.
The TAYLOR SPATIAL FRAME device is a circular, metal frame with two rings that connect with six telescopic struts that can be independently lengthened or shortened relative to the rest of the frame. This allows for six different axes of movement, which gives the TAYLOR SPATIAL FRAME device the ability to correct even the most difficult congenital deformities and trauma cases.

When using the TAYLOR SPATIAL FRAME device, your surgeon inputs information about your original bone deformity into an advanced web-based computer application. This information is then interpreted by the software and a day-by-day treatment plan is created. The software also creates an image of your deformity on screen and shows how the bones should be moving each day, until the bones are completely set in proper alignment.
You then make daily adjustments to the struts, depending on your prescribed course of treatment. As the adjustments are made, the rings of the external fixation device are repositioned with respect to each other, moving bones in the directions necessary for treatment.
Your surgeon is able to make a side-by-side comparison of current X-Rays and the projected plan of treatment graphics created by the TAYLOR SPATIAL FRAME device software. This comparison ensures that your bones are healing in the correct alignment and at the appropriate pace.
The TAYLOR SPATIAL FRAME External Fixator is a winner of the Medical Device Excellence Award.
◊ Trademark of Smith & Nephew
Planning ahead
As other TAYLOR SPATIAL FRAME device patients might tell you, the limb restoration process takes a great deal of preparation and personal commitment. One of the best ways to understand the process is to speak with someone who has gone through the process. Ask your surgeon to introduce you to someone who would be willing to talk to you about their experience and help you prepare for this temporary lifestyle.
Here are some points to consider before you receive the TAYLOR SPATIAL FRAME device:
- Hospitalization: You should plan for a hospital stay of at least three to four days. Ask your surgeon for help in planning what to bring with you and what to expect.
- External Fixator Adjustments: Make the commitment now to follow a schedule of fixator adjustments, which are needed daily during the lengthening/correction phase. Your prescribed course of treatment will be determined by your surgeon.
- Scheduling Considerations: Plan ahead now for the amount of time away from school or work, frequency of clinic visits, time of year and transportation issues you'll face. Your surgeon's clinic can assist you with making these plans.
- Physical Limitations: Understand ahead of time what you will be able to and won't be able to do. Talk to your surgeon about what to expect.
- Changes to Normal Activities: Preparation, more time, energy and rest will be needed to perform daily activities.
- Clothing Adaptations: Make arrangements to wear loose clothing, which will fit over the fixator.
- Insurance Coverage: Know your insurance plan and make sure to secure all approvals prior to surgery. Find out what your insurance will cover for medical equipment as you will need several medical items during your external fixator treatment time. Your surgeon's clinic can give you a list of items that you may need to give to your insurance company.
- Household Furniture and Linens: Your furniture and linens can be protected from damage caused by the fixator by wearing a protective covering over it.

◊ Trademark of Smith & Nephew
Planning ahead
As other TAYLOR SPATIAL FRAME device patients might tell you, the limb restoration process takes a great deal of preparation and personal commitment. One of the best ways to understand the process is to speak with someone who has gone through the process. Ask your surgeon to introduce you to someone who would be willing to talk to you about their experience and help you prepare for this temporary lifestyle.
Here are some points to consider before you receive the TAYLOR SPATIAL FRAME device:
- Hospitalization: You should plan for a hospital stay of at least three to four days. Ask your surgeon for help in planning what to bring with you and what to expect.
- External Fixator Adjustments: Make the commitment now to follow a schedule of fixator adjustments, which are needed daily during the lengthening/correction phase. Your prescribed course of treatment will be determined by your surgeon.
- Scheduling Considerations: Plan ahead now for the amount of time away from school or work, frequency of clinic visits, time of year and transportation issues you'll face. Your surgeon's clinic can assist you with making these plans.
- Physical Limitations: Understand ahead of time what you will be able to and won't be able to do. Talk to your surgeon about what to expect.
- Changes to Normal Activities: Preparation, more time, energy and rest will be needed to perform daily activities.
- Clothing Adaptations: Make arrangements to wear loose clothing, which will fit over the fixator.
- Insurance Coverage: Know your insurance plan and make sure to secure all approvals prior to surgery. Find out what your insurance will cover for medical equipment as you will need several medical items during your external fixator treatment time. Your surgeon's clinic can give you a list of items that you may need to give to your insurance company.
- Household Furniture and Linens: Your furniture and linens can be protected from damage caused by the fixator by wearing a protective covering over it.

◊ Trademark of Smith & Nephew
Your core team
You will need a special team of loved ones and specialists to guide you through the process of wearing the TAYLOR SPATIAL FRAME device.
Since your orthopaedic surgeon has chosen you as a candidate for limb restoration, you should know that your surgeon already has confidence in your potential for success. Knowing and utilizing your core team will help you set realistic goals so you will know what to expect at the end of the process.
Be sure to write down the names and telephone numbers of your core team to have on hand at any time that you need them during your journey with the TAYLOR SPATIAL FRAME device.

You
You are the most crucial team member because your active participation is valuable to the success of the limb correction process. You will be required to assist with external fixator adjustments, as instructed. Without your dedicated commitment and important feedback along the way, other team members cannot operate as effectively in their roles.
Significant Other
It is important that a parent, sibling, spouse or close friend – someone dedicated to your well-being – be involved in the process from beginning to end. They need to understand the procedure and what to expect as well as you do. They also need to participate in the planning process.
Orthopaedic Surgeon
Unlike some areas of medicine, limb correction requires that your surgeon be involved in every phase of the process. He or she makes the initial evaluation, performs the operation to apply the TAYLOR SPATIAL FRAME device, plans your recovery goal and closely follows your progress. The surgeon may have an orthopaedic resident, nurse or physician's assistant specifically trained to help with the surgery, and frame construction and modification.
Orthopaedic Clinic Nursing Staff
Your clinic nurse will coordinate the work of the entire team through each phase of your treatment. Your nurse is often the first person to answer questions, listen to concerns and advise you about problems as they arise.
Physical Therapist
Your physical or occupational therapist will conduct a preoperative assessment of your movement ability and will work with you throughout the process to help you stay as active and independent as possible.
Home Care Discharge Planner
A home care discharge planner will be available before and after surgery to talk about your concerns. They can also help you solve logistical problems such as transportation, temporary housing and rental of medical equipment such as wheelchairs and/or crutches.
◊ Trademark of Smith & Nephew
Your core team
You will need a special team of loved ones and specialists to guide you through the process of wearing the TAYLOR SPATIAL FRAME device.
Since your orthopaedic surgeon has chosen you as a candidate for limb restoration, you should know that your surgeon already has confidence in your potential for success. Knowing and utilizing your core team will help you set realistic goals so you will know what to expect at the end of the process.
Be sure to write down the names and telephone numbers of your core team to have on hand at any time that you need them during your journey with the TAYLOR SPATIAL FRAME device.

You
You are the most crucial team member because your active participation is valuable to the success of the limb correction process. You will be required to assist with external fixator adjustments, as instructed. Without your dedicated commitment and important feedback along the way, other team members cannot operate as effectively in their roles.
Significant Other
It is important that a parent, sibling, spouse or close friend – someone dedicated to your well-being – be involved in the process from beginning to end. They need to understand the procedure and what to expect as well as you do. They also need to participate in the planning process.
Orthopaedic Surgeon
Unlike some areas of medicine, limb correction requires that your surgeon be involved in every phase of the process. He or she makes the initial evaluation, performs the operation to apply the TAYLOR SPATIAL FRAME device, plans your recovery goal and closely follows your progress. The surgeon may have an orthopaedic resident, nurse or physician's assistant specifically trained to help with the surgery, and frame construction and modification.
Orthopaedic Clinic Nursing Staff
Your clinic nurse will coordinate the work of the entire team through each phase of your treatment. Your nurse is often the first person to answer questions, listen to concerns and advise you about problems as they arise.
Physical Therapist
Your physical or occupational therapist will conduct a preoperative assessment of your movement ability and will work with you throughout the process to help you stay as active and independent as possible.
Home Care Discharge Planner
A home care discharge planner will be available before and after surgery to talk about your concerns. They can also help you solve logistical problems such as transportation, temporary housing and rental of medical equipment such as wheelchairs and/or crutches.
◊ Trademark of Smith & Nephew
Your well-being
 Although you will have a great deal of support available during the process, you are your own strongest support system. Your most important job is to take care of yourself. Wearing an external fixator can be stressful.
Although you will have a great deal of support available during the process, you are your own strongest support system. Your most important job is to take care of yourself. Wearing an external fixator can be stressful.
Keep these factors in mind while you're going through the process:
- Know that the discomfort associated with wearing an external fixator is usually mild.
- Anticipate early mobility.
- Keep thinking about the vastly improved quality of life you will have at the end of your treatment.
Actively participate in your care.
- Normal activities of daily living may be more time consuming so allow enough time for these activities to avoid frustration.
- Keep active. Go to the movies, go out to eat, attend football and baseball games, and visit with family and friends.
- Keep your mind busy by reading books, listening to music, exercising, relaxing, crossword puzzles, etc.
Your well-being
 Although you will have a great deal of support available during the process, you are your own strongest support system. Your most important job is to take care of yourself. Wearing an external fixator can be stressful.
Although you will have a great deal of support available during the process, you are your own strongest support system. Your most important job is to take care of yourself. Wearing an external fixator can be stressful.
Keep these factors in mind while you're going through the process:
- Know that the discomfort associated with wearing an external fixator is usually mild.
- Anticipate early mobility.
- Keep thinking about the vastly improved quality of life you will have at the end of your treatment.
Actively participate in your care.
- Normal activities of daily living may be more time consuming so allow enough time for these activities to avoid frustration.
- Keep active. Go to the movies, go out to eat, attend football and baseball games, and visit with family and friends.
- Keep your mind busy by reading books, listening to music, exercising, relaxing, crossword puzzles, etc.
Adjusting the TAYLOR SPATIAL FRAME device

If you are having a limb lengthened or corrected with a TAYLOR SPATIAL FRAME device, you will be required to assist in the process by making external fixator adjustments to the struts at home. This adjustment is made daily. An adjustment plan will be tailored specifically for you and it is imperative that you follow the adjustment schedule exactly.
Your surgeon will make sure that you are trained and understand how and how often to make the adjustments. Your frame adjustment schedule may change at each clinic visit depending on how you progress according to analysis by your surgeon and the TAYLOR SPATIAL FRAME web-based software.
There may be times when you experience some failure of the mechanics of the external fixator, such as broken or bent wires or pins or when you are unable to turn the strut(s). If this happens, call your clinic promptly.
◊ Trademark of Smith & Nephew
Adjusting the TAYLOR SPATIAL FRAME device

If you are having a limb lengthened or corrected with a TAYLOR SPATIAL FRAME device, you will be required to assist in the process by making external fixator adjustments to the struts at home. This adjustment is made daily. An adjustment plan will be tailored specifically for you and it is imperative that you follow the adjustment schedule exactly.
Your surgeon will make sure that you are trained and understand how and how often to make the adjustments. Your frame adjustment schedule may change at each clinic visit depending on how you progress according to analysis by your surgeon and the TAYLOR SPATIAL FRAME web-based software.
There may be times when you experience some failure of the mechanics of the external fixator, such as broken or bent wires or pins or when you are unable to turn the strut(s). If this happens, call your clinic promptly.
◊ Trademark of Smith & Nephew
Clothing modifications
Depending on where your TAYLOR SPATIAL FRAME device is placed, you will have to make clothing modifications and adjustments to your wardrobe.
If the external fixator is on your leg:
- Snap-on sports pants or shorts may be the most comfortable articles of clothing to wear. Some snap all the way up to the waistband, making them easy to get on and off.
- Pants can be altered by cutting the inside seam, up to the crotch, or the outside seam, up to the waistband, and inserting triangular pieces of fabric to widen the leg. You can secure the extra fabric inserts with hooks and loops or with buttons.
- Consider pants with many pockets for carrying multiple items throughout the day.
- During warm weather, you may wish to wear shorts or cut off pants above the external fixator.
For women, loose-fitting dresses or skirts may be your best option. Underwear that ties on both sides at the hip can be used.
- Underwear can be altered by cutting the side seam and using hooks, loops or Velcro® to secure the cut seam.
If the external fixator is on your arm:
- Shirts can be altered by cutting the inside seam of the arm of your shirt and inserting triangular pieces of fabric to widen the arm hole.
- You can secure the extra fabric inserts with hooks and loops or with buttons.
- You can use a shawl or cape to keep warm during colder weather.
- You can cut the cuff off sweaters and shirts to enable the shirt to fit over your arm.
If the external fixator is on your foot:
- You may need to modify a pair of shoes.
- A foot ring with a rubber sole can be added to the fixator. Ask your surgeon about this.
◊ Trademark of Smith & Nephew
Clothing modifications
Depending on where your TAYLOR SPATIAL FRAME device is placed, you will have to make clothing modifications and adjustments to your wardrobe.
If the external fixator is on your leg:
- Snap-on sports pants or shorts may be the most comfortable articles of clothing to wear. Some snap all the way up to the waistband, making them easy to get on and off.
- Pants can be altered by cutting the inside seam, up to the crotch, or the outside seam, up to the waistband, and inserting triangular pieces of fabric to widen the leg. You can secure the extra fabric inserts with hooks and loops or with buttons.
- Consider pants with many pockets for carrying multiple items throughout the day.
- During warm weather, you may wish to wear shorts or cut off pants above the external fixator.
For women, loose-fitting dresses or skirts may be your best option. Underwear that ties on both sides at the hip can be used.
- Underwear can be altered by cutting the side seam and using hooks, loops or Velcro® to secure the cut seam.
If the external fixator is on your arm:
- Shirts can be altered by cutting the inside seam of the arm of your shirt and inserting triangular pieces of fabric to widen the arm hole.
- You can secure the extra fabric inserts with hooks and loops or with buttons.
- You can use a shawl or cape to keep warm during colder weather.
- You can cut the cuff off sweaters and shirts to enable the shirt to fit over your arm.
If the external fixator is on your foot:
- You may need to modify a pair of shoes.
- A foot ring with a rubber sole can be added to the fixator. Ask your surgeon about this.
◊ Trademark of Smith & Nephew
Clinic Visits

You will have a significant number of surgeon clinic visits during your TAYLOR SPATIAL FRAME device treatment. Be sure to discuss this with the home-based team member who is helping you during treatment.
During the lengthening/correction phase, you may visit the clinic every two weeks so that your surgeon can monitor how you are progressing.
During the consolidation phase, you may visit the clinic once a month. Office visits may range from 30 minutes to two hours, depending on what work or evaluations need to be performed.
Follow-up visits may include:
- Measuring the distraction amount since your last visit.
- Assessing the range of motion of the joints above and below the external fixator for contractures. Contractures occur when the joint is not exercised. Without exercise the tendons and muscles shorten causing joint deformity, stiffness, limited mobility and pain.
- Checking the pin sites for inflammation or infection.
- Checking the external fixator frame for loose wires, nuts and bolts.
- Taking X-Rays to check the rate and progress of the lengthening/correction and assess the quality of the new bone growth.
◊ Trademark of Smith & Nephew
Clinic Visits

You will have a significant number of surgeon clinic visits during your TAYLOR SPATIAL FRAME device treatment. Be sure to discuss this with the home-based team member who is helping you during treatment.
During the lengthening/correction phase, you may visit the clinic every two weeks so that your surgeon can monitor how you are progressing.
During the consolidation phase, you may visit the clinic once a month. Office visits may range from 30 minutes to two hours, depending on what work or evaluations need to be performed.
Follow-up visits may include:
- Measuring the distraction amount since your last visit.
- Assessing the range of motion of the joints above and below the external fixator for contractures. Contractures occur when the joint is not exercised. Without exercise the tendons and muscles shorten causing joint deformity, stiffness, limited mobility and pain.
- Checking the pin sites for inflammation or infection.
- Checking the external fixator frame for loose wires, nuts and bolts.
- Taking X-Rays to check the rate and progress of the lengthening/correction and assess the quality of the new bone growth.
◊ Trademark of Smith & Nephew
Getting around with the external fixator
Immediately after surgery, the affected extremity should be elevated above the level of the heart until there are no concerns about swelling. To elevate the affected extremity properly, place a pillow under the heel of your foot so your knee is extended fully.
To move the affected extremity, the leg external fixator must be moved together as a unit. The amount of assistance needed depends on your ability to control the leg during the move. Make sure not to place your hands under the fracture site during movement. This may cause you to apply stress and even slightly manipulate the fracture site.

Standing up and sitting down
When standing up with a leg in a TAYLOR SPATIAL FRAME device, you must use caution so that you do not fall. Always be very careful when sitting down or getting up from a chair if the external fixator is on your leg.
To stand up, move forward to the edge of the chair. Push off against the seat using the hand on the affected side. Push down on the hand piece of your crutch while raising your body to a standing position.
To sit down, back up to the edge of the chair. Hold on to the hand piece of your crutch on your unaffected side. Lower the hand on your affected side to the arm of the chair to lower your body to a sitting position.
Using the toilet
Again, while performing some daily activities with a leg in the TAYLOR SPATIAL FRAME device, you must use caution to prevent falling.
Follow the same steps used in sitting and standing for getting on and off the toilet. You may consider using an elevated toilet seat. For safety, you may consider placing a handrail beside the toilet.
Sleeping
Your body may require more sleep during the treatment process with your TAYLOR SPATIAL FRAME device, due to increased demands in ambulation. The fixator adds extra weight and increased time to maneuver as you go about your day.
Your sleep will be limited to one position – your back. Elevate the limb with the external device for comfort and security. You may want to sleep with the fixator frame cover on to avoid ripping the sheets.
◊ Trademark of Smith & Nephew
Getting around with the external fixator
Immediately after surgery, the affected extremity should be elevated above the level of the heart until there are no concerns about swelling. To elevate the affected extremity properly, place a pillow under the heel of your foot so your knee is extended fully.
To move the affected extremity, the leg external fixator must be moved together as a unit. The amount of assistance needed depends on your ability to control the leg during the move. Make sure not to place your hands under the fracture site during movement. This may cause you to apply stress and even slightly manipulate the fracture site.

Standing up and sitting down
When standing up with a leg in a TAYLOR SPATIAL FRAME device, you must use caution so that you do not fall. Always be very careful when sitting down or getting up from a chair if the external fixator is on your leg.
To stand up, move forward to the edge of the chair. Push off against the seat using the hand on the affected side. Push down on the hand piece of your crutch while raising your body to a standing position.
To sit down, back up to the edge of the chair. Hold on to the hand piece of your crutch on your unaffected side. Lower the hand on your affected side to the arm of the chair to lower your body to a sitting position.
Using the toilet
Again, while performing some daily activities with a leg in the TAYLOR SPATIAL FRAME device, you must use caution to prevent falling.
Follow the same steps used in sitting and standing for getting on and off the toilet. You may consider using an elevated toilet seat. For safety, you may consider placing a handrail beside the toilet.
Sleeping
Your body may require more sleep during the treatment process with your TAYLOR SPATIAL FRAME device, due to increased demands in ambulation. The fixator adds extra weight and increased time to maneuver as you go about your day.
Your sleep will be limited to one position – your back. Elevate the limb with the external device for comfort and security. You may want to sleep with the fixator frame cover on to avoid ripping the sheets.
◊ Trademark of Smith & Nephew
Physical therapy
Within several days of your surgery, you will begin a thorough and on-going orthopedic rehabilitation program designed to improve the blood supply to the limb and promote healing.
If you are having a leg lengthened or corrected, you will begin physical therapy in the hospital until you can walk. Your physical therapist may teach you exercises to help you develop sitting and standing balance, stability and coordination to prepare you for mobilization and ambulation.
If you are having an arm lengthened or corrected, you will begin physical therapy in the hospital until you are able to use the arm for a range of daily care.
Learning to walk with balance and stability or using your arm with coordination after the external fixator is attached usually takes three to four days.
Your therapist will design a home-exercise program encouraging you to maintain the limb's range of motion and strength. Their objective is to help you become as independent as possible to cope with the external fixator and promote healing.
Your exercise program is your surgeon's prescription. The exercise program designed for you will depend on the type of correction or lengthening treatment you are undergoing.
Aerobic activities increase blood flow and strengthen bones. It burns calories, increases resistance to disease and decreases tension. It also releases endorphins – the body's own pain-control system.
To avoid complications, your exercise program should be followed with commitment and discipline. You may be able to walk, ride a stationary bike and swim in a chlorinated, clean pool (after your sutures are out).
You must bear weight on the limb being treated with the external fixator, after you've been released by your surgeon to do so, or you may not heal properly. You must exercise your affected extremity to increase blood flow and grow healthy bone tissue. For a leg fitted with the TAYLOR SPATIAL FRAME device, that means walking. For an arm fitted with an external fixator, that means using small weights. Putting weight on the treated extremity promotes healing.
Whatever the method, exercise is critical for a speedy recovery. Check with your surgeon and your physical therapist for specific instructions.
Learn more about pediatric orthopedic physical therapy and rehabilitation services at Nicklaus Children's Hospital.
◊ Trademark of Smith & Nephew
Physical therapy
Within several days of your surgery, you will begin a thorough and on-going orthopedic rehabilitation program designed to improve the blood supply to the limb and promote healing.
If you are having a leg lengthened or corrected, you will begin physical therapy in the hospital until you can walk. Your physical therapist may teach you exercises to help you develop sitting and standing balance, stability and coordination to prepare you for mobilization and ambulation.
If you are having an arm lengthened or corrected, you will begin physical therapy in the hospital until you are able to use the arm for a range of daily care.
Learning to walk with balance and stability or using your arm with coordination after the external fixator is attached usually takes three to four days.
Your therapist will design a home-exercise program encouraging you to maintain the limb's range of motion and strength. Their objective is to help you become as independent as possible to cope with the external fixator and promote healing.
Your exercise program is your surgeon's prescription. The exercise program designed for you will depend on the type of correction or lengthening treatment you are undergoing.
Aerobic activities increase blood flow and strengthen bones. It burns calories, increases resistance to disease and decreases tension. It also releases endorphins – the body's own pain-control system.
To avoid complications, your exercise program should be followed with commitment and discipline. You may be able to walk, ride a stationary bike and swim in a chlorinated, clean pool (after your sutures are out).
You must bear weight on the limb being treated with the external fixator, after you've been released by your surgeon to do so, or you may not heal properly. You must exercise your affected extremity to increase blood flow and grow healthy bone tissue. For a leg fitted with the TAYLOR SPATIAL FRAME device, that means walking. For an arm fitted with an external fixator, that means using small weights. Putting weight on the treated extremity promotes healing.
Whatever the method, exercise is critical for a speedy recovery. Check with your surgeon and your physical therapist for specific instructions.
Learn more about pediatric orthopedic physical therapy and rehabilitation services at Nicklaus Children's Hospital.
◊ Trademark of Smith & Nephew
Pain management
Pain management is essential to your well-being and recovery. Pain may decrease your desire and ability to walk or move your arm and actively participate in physical therapy.
Pain may also cause the adoption of protective postures, which may lead to joint stiffness and decreased joint mobility. Although the process of the bones moving should not be painful, poor pin care may cause the skin around the pin sites to become taut, causing pain at the level of the skin.
Your positive attitude through the ILIZAROV process is important to its success. This means you will have to find ways to cope with discomfort, pain and frustration – in addition the natural ups and downs of your emotions during this long process.
Whenever possible, tell your surgeon or nurse what is troubling you, and be prepared to experience some degree of pain from the beginning. The pain should, however, always be manageable. Each individual experiences pain differently. Whatever the degree of your pain in the beginning, it should get progressively better.
The first few days after the initial surgery, it is likely that you will feel considerable pain or discomfort. Your surgeon has planned for this and will administer pain medication as needed. You may receive pain medication intravenously for a few days.

Tips for Pain Management in Children
- Follow your doctor's instructions regarding exercises. Do not allow your knee, ankle or elbow to become stiff.
- Keep the pin sites clean.
- Elevate the affected extremity while at rest, securing position and proper alignment to decrease pain and swelling.
- Practice relaxation, distraction and imagery techniques to calm yourself and relax your muscles.
- Contact your physician promptly if you experience increased pain, discomfort or swelling not relieved by rest.
◊ Trademark of Smith & Nephew
Pain management
Pain management is essential to your well-being and recovery. Pain may decrease your desire and ability to walk or move your arm and actively participate in physical therapy.
Pain may also cause the adoption of protective postures, which may lead to joint stiffness and decreased joint mobility. Although the process of the bones moving should not be painful, poor pin care may cause the skin around the pin sites to become taut, causing pain at the level of the skin.
Your positive attitude through the ILIZAROV process is important to its success. This means you will have to find ways to cope with discomfort, pain and frustration – in addition the natural ups and downs of your emotions during this long process.
Whenever possible, tell your surgeon or nurse what is troubling you, and be prepared to experience some degree of pain from the beginning. The pain should, however, always be manageable. Each individual experiences pain differently. Whatever the degree of your pain in the beginning, it should get progressively better.
The first few days after the initial surgery, it is likely that you will feel considerable pain or discomfort. Your surgeon has planned for this and will administer pain medication as needed. You may receive pain medication intravenously for a few days.

Tips for Pain Management in Children
- Follow your doctor's instructions regarding exercises. Do not allow your knee, ankle or elbow to become stiff.
- Keep the pin sites clean.
- Elevate the affected extremity while at rest, securing position and proper alignment to decrease pain and swelling.
- Practice relaxation, distraction and imagery techniques to calm yourself and relax your muscles.
- Contact your physician promptly if you experience increased pain, discomfort or swelling not relieved by rest.
◊ Trademark of Smith & Nephew
Pin tract sites
The TAYLOR SPATIAL FRAME device is attached to the outside of your limb with pins and wires that penetrate your skin through your bone and out the other side. Pin tract sites are where the pins and wires go through your skin.
Pin-tract infections are a common problem around these pin sites, but may be avoided with proper pin care. You will have a major responsibility to make sure that the pin site areas are cleaned daily - you must take vigilant care to keep the pint tract sites clean and free of infection.
Pin site care
Your surgeon will guide you in the proper care and cleaning of the pin sites. You will need to learn how to remove dried blood and scabs from the pin sites to keep your skin from adhering to the pins and allow free drainage of your pin site. Gentle massage around the pin sites may also help to keep your skin from adhering to the pins. Be gentle when you massage around your pin sites as excessive skin motion on the pins may cause infection. If you have difficulty reaching or seeing all the pin sites, have a family member or friend help, or you can use a mirror.
Make sure that you follow your surgeon's recommendations for proper pin site care to avoid infection.

Showers with the external fixator
You may not be allowed to shower for approximately five to seven days after initial placement of the TAYLOR SPATIAL FRAME™ device. Until you are allowed to shower, your surgeon may have you clean the pin sites with cotton swabs and normal saline or other topical cleaner or antibiotic that your surgeon prescribes. During the first few days after the external fixator is placed, expect a clear yellow or slightly bloody drainage from the pin sites.
As long as there are no open wounds and your surgeon allows it, you can shower with the TAYLOR SPATIAL FRAME device in place. You may consider placing a rubber mat in the tub or utilizing a shower chair or installing handrails in your shower for safety. When you are released to take showers, cleaning the pin sites with an antibacterial liquid soap and water while in the shower has proven to be a simple and effective external fixator pin care method. Allow the soap and water to run down the extremity that the external fixator is attached to. Do not scrub. Rinse and dry the fixator and the extremity thoroughly. You can dry using a hair dryer on a cool setting.
Any activities that involve soaking the external fixator in potentially contaminated water are discouraged. That means no natural ocean waters, rivers, etc. Your surgeon may, however, allow you to swim in a clean, chlorinated pool after your sutures are removed.
Pin-tract infections
Because you will have pins and wires going through your skin into your bone, there is a risk for pin-tract infections. With proper cleaning, protection and care of your pin sites, you may never have an infection – which is the goal. Call your surgeon if you experience any of the following symptoms:
- Redness, warmth and swelling at the pin sites. A small amount of redness is normal.
- Extrememly tender pin sites.
- Persistant fever of 100.5 farenheit or higher- taken orally.
- Thick, cloudy, white, yellow or green drainage from the pin sites. Clear yellow or slightly bloody drainage is normal.
- Odor at the pin sites.
Nerve problems
If you experience pain in a place where there are no pins, this may be the first sign of a nerve problem. This is called 'referred pain.' The next sign is an increased or decreased feeling in the area of your foot or hand, depending on where your external fixator is located. You could experience these symptoms during the initial correction phase of your treatment with the TAYLOR SPATIAL FRAME fixator. Report these symptoms to your surgeon as soon as possible. They may be indications of nerve irritation.
Smith & Nephew
Pin tract sites
The TAYLOR SPATIAL FRAME device is attached to the outside of your limb with pins and wires that penetrate your skin through your bone and out the other side. Pin tract sites are where the pins and wires go through your skin.
Pin-tract infections are a common problem around these pin sites, but may be avoided with proper pin care. You will have a major responsibility to make sure that the pin site areas are cleaned daily - you must take vigilant care to keep the pint tract sites clean and free of infection.
Pin site care
Your surgeon will guide you in the proper care and cleaning of the pin sites. You will need to learn how to remove dried blood and scabs from the pin sites to keep your skin from adhering to the pins and allow free drainage of your pin site. Gentle massage around the pin sites may also help to keep your skin from adhering to the pins. Be gentle when you massage around your pin sites as excessive skin motion on the pins may cause infection. If you have difficulty reaching or seeing all the pin sites, have a family member or friend help, or you can use a mirror.
Make sure that you follow your surgeon's recommendations for proper pin site care to avoid infection.

Showers with the external fixator
You may not be allowed to shower for approximately five to seven days after initial placement of the TAYLOR SPATIAL FRAME™ device. Until you are allowed to shower, your surgeon may have you clean the pin sites with cotton swabs and normal saline or other topical cleaner or antibiotic that your surgeon prescribes. During the first few days after the external fixator is placed, expect a clear yellow or slightly bloody drainage from the pin sites.
As long as there are no open wounds and your surgeon allows it, you can shower with the TAYLOR SPATIAL FRAME device in place. You may consider placing a rubber mat in the tub or utilizing a shower chair or installing handrails in your shower for safety. When you are released to take showers, cleaning the pin sites with an antibacterial liquid soap and water while in the shower has proven to be a simple and effective external fixator pin care method. Allow the soap and water to run down the extremity that the external fixator is attached to. Do not scrub. Rinse and dry the fixator and the extremity thoroughly. You can dry using a hair dryer on a cool setting.
Any activities that involve soaking the external fixator in potentially contaminated water are discouraged. That means no natural ocean waters, rivers, etc. Your surgeon may, however, allow you to swim in a clean, chlorinated pool after your sutures are removed.
Pin-tract infections
Because you will have pins and wires going through your skin into your bone, there is a risk for pin-tract infections. With proper cleaning, protection and care of your pin sites, you may never have an infection – which is the goal. Call your surgeon if you experience any of the following symptoms:
- Redness, warmth and swelling at the pin sites. A small amount of redness is normal.
- Extrememly tender pin sites.
- Persistant fever of 100.5 farenheit or higher- taken orally.
- Thick, cloudy, white, yellow or green drainage from the pin sites. Clear yellow or slightly bloody drainage is normal.
- Odor at the pin sites.
Nerve problems
If you experience pain in a place where there are no pins, this may be the first sign of a nerve problem. This is called 'referred pain.' The next sign is an increased or decreased feeling in the area of your foot or hand, depending on where your external fixator is located. You could experience these symptoms during the initial correction phase of your treatment with the TAYLOR SPATIAL FRAME fixator. Report these symptoms to your surgeon as soon as possible. They may be indications of nerve irritation.
Smith & Nephew
After treatment
After the TAYLOR SPATIAL FRAME device is removed, you may have to wear a cast or a brace on the limb that was lengthened or corrected for a period of time. This will give your bones a little longer to heal and consolidate (strengthen). The length of time that you may have to wear a brace or a cast is dependent on how well your bone has consolidated. Your surgeon will make the determination whether you will require a brace or a cast.
Your surgeon will likely recommend that you continue your exercises and increase your activity level. Motion and bearing weight on your affected limb promotes bone healing and strengthening.
◊ Trademark of Smith & Nephew
After treatment
After the TAYLOR SPATIAL FRAME device is removed, you may have to wear a cast or a brace on the limb that was lengthened or corrected for a period of time. This will give your bones a little longer to heal and consolidate (strengthen). The length of time that you may have to wear a brace or a cast is dependent on how well your bone has consolidated. Your surgeon will make the determination whether you will require a brace or a cast.
Your surgeon will likely recommend that you continue your exercises and increase your activity level. Motion and bearing weight on your affected limb promotes bone healing and strengthening.
◊ Trademark of Smith & Nephew
Frequently asked questions
How fast can bone grow?
Your bone can grow up to one millimeter per day.
How long do I have to wear the external fixator?
Typical external fixator patients wear the device from four to twelve months. The severity of the problem you need reconstructed, your health, weight and other factors play a role in the length of time you will need to wear the external fixator. Your surgeon will be able to provide you with a timeline for your specific case.

What are the stages of lengthening/correction?
- Correction/Distraction – This begins a few days postoperatively when you will begin the process of moving the struts as directed to create a space between your bones to promote bone growth. Typically, you will adjust the struts four times a day, every six hours, approximately 0.25mm each time, for a total of 1mm in a 24-hour period.
- Consolidation – During this time period you will wear the external fixator, but you will not adjust the struts. This allows time for the new bone growth to consolidate (strengthen) and prepare for removal of the external fixator.
How is the TAYLOR SPATIAL FRAME device attached and removed?
You will have at least two surgeries related to the TAYLOR SPATIAL FRAME device. Both the installation and the removal of the device will require a surgical procedure.
There is the possibility of serious complications with any surgery. Your surgeon will not schedule you for surgery unless he feels that you are healthy enough to have the procedure. Discuss possible complications and what to expect with your surgeon.
Only after X-Ray exams of the consolidated bone show it is completely healed will the TAYLOR SPATIAL FRAME device be removed. This will be performed under general anesthesia, usually as an outpatient surgical procedure. Afterwards, you may have to wear a brace or a cast, to give the bone more time to heal.
You may have certain physical limitations at first, depending on your bone healing progress and specific situation. Consult your surgeon about your limitations.
◊ Trademark of Smith & Nephew
Frequently asked questions
How fast can bone grow?
Your bone can grow up to one millimeter per day.
How long do I have to wear the external fixator?
Typical external fixator patients wear the device from four to twelve months. The severity of the problem you need reconstructed, your health, weight and other factors play a role in the length of time you will need to wear the external fixator. Your surgeon will be able to provide you with a timeline for your specific case.

What are the stages of lengthening/correction?
- Correction/Distraction – This begins a few days postoperatively when you will begin the process of moving the struts as directed to create a space between your bones to promote bone growth. Typically, you will adjust the struts four times a day, every six hours, approximately 0.25mm each time, for a total of 1mm in a 24-hour period.
- Consolidation – During this time period you will wear the external fixator, but you will not adjust the struts. This allows time for the new bone growth to consolidate (strengthen) and prepare for removal of the external fixator.
How is the TAYLOR SPATIAL FRAME device attached and removed?
You will have at least two surgeries related to the TAYLOR SPATIAL FRAME device. Both the installation and the removal of the device will require a surgical procedure.
There is the possibility of serious complications with any surgery. Your surgeon will not schedule you for surgery unless he feels that you are healthy enough to have the procedure. Discuss possible complications and what to expect with your surgeon.
Only after X-Ray exams of the consolidated bone show it is completely healed will the TAYLOR SPATIAL FRAME device be removed. This will be performed under general anesthesia, usually as an outpatient surgical procedure. Afterwards, you may have to wear a brace or a cast, to give the bone more time to heal.
You may have certain physical limitations at first, depending on your bone healing progress and specific situation. Consult your surgeon about your limitations.
◊ Trademark of Smith & Nephew
Ambulation with crutches
During the correction phase while wearing the TAYLOR SPATIAL FRAME device, you may be required to use crutches if your leg is the affected limb. Your surgeon will prescribe a weight-bearing status for you to walk, either partial weight bearing or full weight bearing, which will determine whether or not you will be required to use crutches.
Before walking with crutches, it is important that you are fit properly for them and that you know how to use crutches correctly and safely. Your physical therapist will teach you techniques for standing, walking and maneuvering yourself with crutches. With a little time, practice and patience, you will learn how to walk with crutches.
Tips for Using Crutches
- Crutches should be custom adjusted to your body size.
- Make sure you have a thick foam rubber pad on the underarm piece to relieve pressure of the crutch on the upper arm and thoracic cage (ribs). Never put pressure in the axilla (armpit) when using crutches.
- Weight should be supported on the hand pieces to avoid damage to the nerves under the armpits (brachial plexus nerves), which can cause 'crutch paralysis.
- Walking with crutches can take a toll on the hands. Protect your hands from pain and calluses by using hand-piece pads in good condition.
- Long-term crutch users may benefit from new shock absorbing crutches.
- If you are getting numbness in the hands, have your physical therapist check your crutch length and crutch technique. Ask about Canadian Crutches.
- Keep your body weight down.
- Make sure your crutches have large rubber suction tips.
- Good balance and erect posture are essential for crutch walking. Learn to balance by standing next to a chair on the unaffected leg. Wear well-fitting shoes with firm soles to prevent falls.
- Stay away from wet, slippery surfaces, freshly waxed floors and rough, uneven surfaces.
- Going up and down stairs requires both strength and flexibility. Make sure someone is by your side until you have regained your strength and mobility.
- To go up and down stairs, remember – up with the good leg, down with the affected leg.
◊ Trademark of Smith & Nephew
Ambulation with crutches
During the correction phase while wearing the TAYLOR SPATIAL FRAME device, you may be required to use crutches if your leg is the affected limb. Your surgeon will prescribe a weight-bearing status for you to walk, either partial weight bearing or full weight bearing, which will determine whether or not you will be required to use crutches.
Before walking with crutches, it is important that you are fit properly for them and that you know how to use crutches correctly and safely. Your physical therapist will teach you techniques for standing, walking and maneuvering yourself with crutches. With a little time, practice and patience, you will learn how to walk with crutches.
Tips for Using Crutches
- Crutches should be custom adjusted to your body size.
- Make sure you have a thick foam rubber pad on the underarm piece to relieve pressure of the crutch on the upper arm and thoracic cage (ribs). Never put pressure in the axilla (armpit) when using crutches.
- Weight should be supported on the hand pieces to avoid damage to the nerves under the armpits (brachial plexus nerves), which can cause 'crutch paralysis.
- Walking with crutches can take a toll on the hands. Protect your hands from pain and calluses by using hand-piece pads in good condition.
- Long-term crutch users may benefit from new shock absorbing crutches.
- If you are getting numbness in the hands, have your physical therapist check your crutch length and crutch technique. Ask about Canadian Crutches.
- Keep your body weight down.
- Make sure your crutches have large rubber suction tips.
- Good balance and erect posture are essential for crutch walking. Learn to balance by standing next to a chair on the unaffected leg. Wear well-fitting shoes with firm soles to prevent falls.
- Stay away from wet, slippery surfaces, freshly waxed floors and rough, uneven surfaces.
- Going up and down stairs requires both strength and flexibility. Make sure someone is by your side until you have regained your strength and mobility.
- To go up and down stairs, remember – up with the good leg, down with the affected leg.
◊ Trademark of Smith & Nephew
6. Medical Equipment after Spinal Fusion Surgery
Your child will be groggy and sleep a lot during the first few days after surgery, and he/she might not remember much. Gradually, your child will be more alert and will begin to feel better. Improvement will be evident each day.
The following information is about some of the equipment you can expect to see after surgery.
- A cardiac monitor gives information about your heart rate, breathing, and blood pressure via stickers placed on the chest. The monitor is used during the first 48 hours after surgery.
- A pulse oximeter fits like a clip Band-Aid® or bandage on a fingertip and measures how much oxygen is in the blood. This is usually worn for the first two to three days post operation.
- An IV is usually placed in the arm or hand and sometimes in the neck. This is how your child will receive fluids and medicines until he/she is drinking enough on his/her own. One IV will stay in place for most or all of the hospital stay.
- Your child will have a PCA pump, this unit will be connected to your child’s IV. The PCA pump is the method through which your child will receive pain medication for the first two to three days after surgery. There is a button attached to the pump that your child can push to get medicine when he/she needs it. The PCA pump is programmed so your child cannot receive too much medicine. Make sure you contact the nursing staff immediately if your child does not seem comfortable enough with the current pain management plan. Your child’s nurse or doctor may have other options available.
- A urinary or foley catheter is inserted in your child’s bladder during surgery. This will drain urine until your child is able to use the restroom on his/her own. The catheter is taped to the leg and will not fall out when your child moves. The catheter will be removed three days after surgery.
- Patients will have a Jackson-Pratt, a drain placed in the incision during surgery, to help remove extra fluid from the back. This drain is normally removed the day after surgery. This does not hurt!!!
6. Medical Equipment after Spinal Fusion Surgery
Your child will be groggy and sleep a lot during the first few days after surgery, and he/she might not remember much. Gradually, your child will be more alert and will begin to feel better. Improvement will be evident each day.
The following information is about some of the equipment you can expect to see after surgery.
- A cardiac monitor gives information about your heart rate, breathing, and blood pressure via stickers placed on the chest. The monitor is used during the first 48 hours after surgery.
- A pulse oximeter fits like a clip Band-Aid® or bandage on a fingertip and measures how much oxygen is in the blood. This is usually worn for the first two to three days post operation.
- An IV is usually placed in the arm or hand and sometimes in the neck. This is how your child will receive fluids and medicines until he/she is drinking enough on his/her own. One IV will stay in place for most or all of the hospital stay.
- Your child will have a PCA pump, this unit will be connected to your child’s IV. The PCA pump is the method through which your child will receive pain medication for the first two to three days after surgery. There is a button attached to the pump that your child can push to get medicine when he/she needs it. The PCA pump is programmed so your child cannot receive too much medicine. Make sure you contact the nursing staff immediately if your child does not seem comfortable enough with the current pain management plan. Your child’s nurse or doctor may have other options available.
- A urinary or foley catheter is inserted in your child’s bladder during surgery. This will drain urine until your child is able to use the restroom on his/her own. The catheter is taped to the leg and will not fall out when your child moves. The catheter will be removed three days after surgery.
- Patients will have a Jackson-Pratt, a drain placed in the incision during surgery, to help remove extra fluid from the back. This drain is normally removed the day after surgery. This does not hurt!!!
9. Tips for Parents After Spinal Fusion
The following are suggestions from families of children or teens who have undergone spinal fusion:
- Bring a pad of paper and a pen to take notes and list questions you may have for the doctor. Doctors usually visit in the morning and during the course of a day, you may forget some of your questions.
- Bring a journal to record what happens during the hospital stay and your thoughts. This is a great stress reliever and opportunity for your child to look back on his or her experience.
- If your child has long hair, braid it before surgery.
- Bring a camera.
- Bring all needed phone numbers to the hospital.
- Set up a "calling tree" to help you update others about your child’s progress. For example, you might make one phone call to a friend or family member and then have that person call others.
- Limit all visitors until at least the third day after surgery.
- Bring comfortable clothes for you to sleep in during your hospital stay. There is little privacy.
- Bring a water bottle for yourself.
- For your child, bring button-front pajamas/shirts and loose-fitting clothing.
- Bring lip balm for your child.
- It is common for girls to menstruate during their hospital stay, so be sure to bring your own personal hygiene supplies.
- Your child may have swelling of the face, arms, hands or other areas after surgery. This is common and will decrease within a day or two.
- In the first few days after surgery, your child will receive a significant amount of medication to help him/her be comfortable. It is helpful to tell your child the date and time every time that he/she is awake.
- Do not allow visitors to sit on or bump your child’s bed. Instruct visitors to be gentle when they touch.
- Be prepared for your child to exhibit a wide range of emotions you may not be accustomed to seeing. This is very common after spinal fusion surgery.
- Limit perfumes and colognes as your child may be sensitive to even familiar scents.
- Bring several pillows for the car ride home.
- It may be helpful to use a baby monitor to help your child communicate at home.


9. Tips for Parents After Spinal Fusion
The following are suggestions from families of children or teens who have undergone spinal fusion:
- Bring a pad of paper and a pen to take notes and list questions you may have for the doctor. Doctors usually visit in the morning and during the course of a day, you may forget some of your questions.
- Bring a journal to record what happens during the hospital stay and your thoughts. This is a great stress reliever and opportunity for your child to look back on his or her experience.
- If your child has long hair, braid it before surgery.
- Bring a camera.
- Bring all needed phone numbers to the hospital.
- Set up a "calling tree" to help you update others about your child’s progress. For example, you might make one phone call to a friend or family member and then have that person call others.
- Limit all visitors until at least the third day after surgery.
- Bring comfortable clothes for you to sleep in during your hospital stay. There is little privacy.
- Bring a water bottle for yourself.
- For your child, bring button-front pajamas/shirts and loose-fitting clothing.
- Bring lip balm for your child.
- It is common for girls to menstruate during their hospital stay, so be sure to bring your own personal hygiene supplies.
- Your child may have swelling of the face, arms, hands or other areas after surgery. This is common and will decrease within a day or two.
- In the first few days after surgery, your child will receive a significant amount of medication to help him/her be comfortable. It is helpful to tell your child the date and time every time that he/she is awake.
- Do not allow visitors to sit on or bump your child’s bed. Instruct visitors to be gentle when they touch.
- Be prepared for your child to exhibit a wide range of emotions you may not be accustomed to seeing. This is very common after spinal fusion surgery.
- Limit perfumes and colognes as your child may be sensitive to even familiar scents.
- Bring several pillows for the car ride home.
- It may be helpful to use a baby monitor to help your child communicate at home.


1. What Exactly is Scoliosis and Spinal Fusion Surgery?
Everyone’s spine has curves. These curves produce the normal rounding of the shoulders and the sway of the lower back. Scoliosis is a condition that causes the spine to bend sideways and twist.
Scoliosis can occur in:
- he upper back (thoracic)
- lower back (lumbar)
- or in the neck area (cervical)
You may also have curvature in more than one area. Scoliosis is more commonly seen in girls than in boys. Uneven shoulders or a shoulder blade that protrudes when a child bends over are often the first indicators of the condition. The most common form of scoliosis is idiopathic scoliosis, which means the cause is unknown. Your doctor may recommend surgery if the spinal curve continues to progress despite treatments, such as bracing.
The goal of spinal fusion surgery is to stop the progression of the curve. During the surgery, the doctor attaches screws and rods to both sides of the spine and the curve is gently straightened. Small bone grafts taken from the spine and ribs are placed next to the spine. These bone grafts act like cement. As the bone grafts heal, the spine will become solid and the curve will not progress. Until the bones have healed, they need support to keep them from curving again. The rods attached to the spine hold everything in place and support the spine until the bones fuse together.
Your spinal fusion surgery may be performed from the back (posterior), the side (anterior) or both. Your surgeon will determine which is best for you.
Why do it?
Some of the reasons teens say they are glad they had this surgery are:
- Less back pain
- Better posture
- Clothing fits better
- Prevention of a larger curve with larger side effects.
1. What Exactly is Scoliosis and Spinal Fusion Surgery?
Everyone’s spine has curves. These curves produce the normal rounding of the shoulders and the sway of the lower back. Scoliosis is a condition that causes the spine to bend sideways and twist.
Scoliosis can occur in:
- he upper back (thoracic)
- lower back (lumbar)
- or in the neck area (cervical)
You may also have curvature in more than one area. Scoliosis is more commonly seen in girls than in boys. Uneven shoulders or a shoulder blade that protrudes when a child bends over are often the first indicators of the condition. The most common form of scoliosis is idiopathic scoliosis, which means the cause is unknown. Your doctor may recommend surgery if the spinal curve continues to progress despite treatments, such as bracing.
The goal of spinal fusion surgery is to stop the progression of the curve. During the surgery, the doctor attaches screws and rods to both sides of the spine and the curve is gently straightened. Small bone grafts taken from the spine and ribs are placed next to the spine. These bone grafts act like cement. As the bone grafts heal, the spine will become solid and the curve will not progress. Until the bones have healed, they need support to keep them from curving again. The rods attached to the spine hold everything in place and support the spine until the bones fuse together.
Your spinal fusion surgery may be performed from the back (posterior), the side (anterior) or both. Your surgeon will determine which is best for you.
Why do it?
Some of the reasons teens say they are glad they had this surgery are:
- Less back pain
- Better posture
- Clothing fits better
- Prevention of a larger curve with larger side effects.
2. Preparing for Spinal Fusion Surgery
What can you do to prepare for a back surgery?
You can do yourself a huge favor by exercising and being physically active before your surgery. Daily stretches, stomach crunches, and leg stretches are all examples of exercises that help you heal faster and recover more easily. Exercising is also a great way to relieve the stress that may be building up inside you.
In the months or weeks before your surgery, it is very important to maintain a positive attitude. Try not to dwell on what is ahead. Have as much fun as you can, safely. Stay active, keep busy, and most of all, don't feel sorry for yourself! Try to think of things to do that you may not be able to do right after your surgery. Some suggestions include swimming, horseback riding, water park slides, roller coaster rides, rollerblading, ice skating, dancing, golfing, and driving. The night before your procedure, you may want to spend some time by yourself. It will be awhile before anyone lets you do something by yourself again.
Donating Blood Before Your Surgery
It is normal to lose blood during surgery. The surgeons will use multiple advances in medicine to reduce the blood loss during surgery, despite the use of this technology, some patients will require blood transfusions during hospitalizations. There are different ways of preparing blood donations for your surgery:
- You may donate your own blood before your surgery (lots of kids and teens do this!).
- Your family or friends can donate their blood for you.
- You may get blood from the blood bank here at the hospital.
To donate blood prior to the surgery, please refer to OneBlood at www.oneblood.org or call 954-777-264 for locations, hours of operation and to schedule an appointment online. As a reminder, please take the prescription for blood donation with you to the donor center.
Medications
To decrease the risk of excessive bleeding during surgery, you will be asked to avoid taking aspirin-containing medications or non-steroidal anti-inflammatory medications (Advil, Ibuprofen, Motrin, Aleeve) starting at two weeks prior to surgery. You may not resume taking these medications again until instructed by the surgeon.
2. Preparing for Spinal Fusion Surgery
What can you do to prepare for a back surgery?
You can do yourself a huge favor by exercising and being physically active before your surgery. Daily stretches, stomach crunches, and leg stretches are all examples of exercises that help you heal faster and recover more easily. Exercising is also a great way to relieve the stress that may be building up inside you.
In the months or weeks before your surgery, it is very important to maintain a positive attitude. Try not to dwell on what is ahead. Have as much fun as you can, safely. Stay active, keep busy, and most of all, don't feel sorry for yourself! Try to think of things to do that you may not be able to do right after your surgery. Some suggestions include swimming, horseback riding, water park slides, roller coaster rides, rollerblading, ice skating, dancing, golfing, and driving. The night before your procedure, you may want to spend some time by yourself. It will be awhile before anyone lets you do something by yourself again.
Donating Blood Before Your Surgery
It is normal to lose blood during surgery. The surgeons will use multiple advances in medicine to reduce the blood loss during surgery, despite the use of this technology, some patients will require blood transfusions during hospitalizations. There are different ways of preparing blood donations for your surgery:
- You may donate your own blood before your surgery (lots of kids and teens do this!).
- Your family or friends can donate their blood for you.
- You may get blood from the blood bank here at the hospital.
To donate blood prior to the surgery, please refer to OneBlood at www.oneblood.org or call 954-777-264 for locations, hours of operation and to schedule an appointment online. As a reminder, please take the prescription for blood donation with you to the donor center.
Medications
To decrease the risk of excessive bleeding during surgery, you will be asked to avoid taking aspirin-containing medications or non-steroidal anti-inflammatory medications (Advil, Ibuprofen, Motrin, Aleeve) starting at two weeks prior to surgery. You may not resume taking these medications again until instructed by the surgeon.
3. Preparing for your Hospital Stay
Your Hospital Room
In the hospital, you will be assigned to a room where you will stay throughout the duration of your admission at Nicklaus Children's Hospital. This is your room and you can bring items with you to make it feel "like home." In addition to essentials, you may want to bring some sources of entertainment, as well as special items that make you feel comfortable. Here is a list to get you started:
- Pillow
- Favorite blanket or comforter
- Personal items:
- toothbrush, toothpaste, lotion, deodorant, hair ties, hair brush or comb, sanitary pads, etc (Yes, the hospital provides these, but it is nice to have your own)
- Stuffed animals, toys
- Books
- Pictures of your friends, family and pets
- Laptop/tablets/cell phones and battery charger
- Lip balm
- Slippers with a non-slip bottom
What Clothing Should you Bring?
The clothing you bring should be very loose, comfortable, and very easy to put on and take off. Here are a few suggestions:
- Choose shorts or pants with a loose waistband. Boxers work great!
- Button-up or oversized shirts are good choices that will eliminate the need to lift your arms over your head when changing.
- You may also wear hospital gowns the entire time, if you prefer. It’s your choice!
More Helpful Hints
- Do not wear any jewelry the day of surgery.
- If you have long hair, try to avoid leaving it loose. A good way to prevent the tangles associated with lying in bed for several days is to part your hair down the middle and put it into two French braids. Regular braids also will work.
- Bring things to help pass the time (music/headphones, magazines, card games, etc).
- If you want to keep a journal, this is a great time and place to work on it.



3. Preparing for your Hospital Stay
Your Hospital Room
In the hospital, you will be assigned to a room where you will stay throughout the duration of your admission at Nicklaus Children's Hospital. This is your room and you can bring items with you to make it feel "like home." In addition to essentials, you may want to bring some sources of entertainment, as well as special items that make you feel comfortable. Here is a list to get you started:
- Pillow
- Favorite blanket or comforter
- Personal items:
- toothbrush, toothpaste, lotion, deodorant, hair ties, hair brush or comb, sanitary pads, etc (Yes, the hospital provides these, but it is nice to have your own)
- Stuffed animals, toys
- Books
- Pictures of your friends, family and pets
- Laptop/tablets/cell phones and battery charger
- Lip balm
- Slippers with a non-slip bottom
What Clothing Should you Bring?
The clothing you bring should be very loose, comfortable, and very easy to put on and take off. Here are a few suggestions:
- Choose shorts or pants with a loose waistband. Boxers work great!
- Button-up or oversized shirts are good choices that will eliminate the need to lift your arms over your head when changing.
- You may also wear hospital gowns the entire time, if you prefer. It’s your choice!
More Helpful Hints
- Do not wear any jewelry the day of surgery.
- If you have long hair, try to avoid leaving it loose. A good way to prevent the tangles associated with lying in bed for several days is to part your hair down the middle and put it into two French braids. Regular braids also will work.
- Bring things to help pass the time (music/headphones, magazines, card games, etc).
- If you want to keep a journal, this is a great time and place to work on it.



7. Pain After Spinal Fusion Surgery
The first two or three days are the most difficult. After that, each day gets better.
You probably won’t have as much privacy as you are accustomed to during the first few days. Not being able to do some things for yourself may be embarrassing or it may not bother you as much as you think. Remember, you have more important things to be concerned about.
There are a lot of things you may have to do that you may not want to do or may not feel like doing. You may feel agitated because so many people are telling you what to do. Because you are frustrated and uncomfortable, you may feel emotionally explosive. Try not to take it out on the people around you.
Remember, they are doing everything they can to help you feel better and get you home faster. When you are feeling frustrated, try to think about what you can do today that you were unable to do yesterday. You have already come a long way!
The best way to make this an easier experience is to work together with the nurses, therapists, doctors and your family. Communicating with the care team will greatly benefit you and will help them take better care of you.
Everyone’s experience with pain after spinal fusion surgery is different. Your doctors, nurses and family all have the same goal: to help you be as comfortable as possible. Tension in your body and tightening of your muscles can make you hurt more, so it is very important to help yourself relax and stay as calm as possible. It is okay to ask for medicine for your pain when you need it. In fact, the medicine works best if you receive it before the pain becomes unbearable!
Pain After Spinal Fusion Surgery
Your nurse will frequently ask you the level of your pain. He or she will use what we call a "pain scale" from 0-10. The 0 represents no pain, while the 10 signifies pain that is the worst you’ve ever experienced. Your nurse may ask you to describe your pain with words such as sharp, burning, throbbing or dull. Please be honest with your nurses at all times. They are here to help keep you comfortable.
Here are some suggestions that have helped other kids and teens relieve pain after scoliosis surgery:
- Change your position.
- Channel your pain. Think about the pain moving out of your body or concentrate on another part of your body such as your thumb or elbow.
- Listen to relaxing music.
- Have someone wash your face or hair. Feeling calm and fresh makes a world of difference.
- Have someone read to you.
- Change the look and feel of your room. For example, turn off the lights, close the blinds and turn on a fan to cool you.
- Use breathing techniques. Taking slow deep breaths sometimes helps your body to relax.
- Get up and move around.
- Go for a short walk (with help of course!).
The most important thing you can do is to identify what helps you relax and then make a plan for yourself. Share your plan with a family member who will be at the hospital with you or write it down. Always keep a positive attitude; each day will get better!
7. Pain After Spinal Fusion Surgery
The first two or three days are the most difficult. After that, each day gets better.
You probably won’t have as much privacy as you are accustomed to during the first few days. Not being able to do some things for yourself may be embarrassing or it may not bother you as much as you think. Remember, you have more important things to be concerned about.
There are a lot of things you may have to do that you may not want to do or may not feel like doing. You may feel agitated because so many people are telling you what to do. Because you are frustrated and uncomfortable, you may feel emotionally explosive. Try not to take it out on the people around you.
Remember, they are doing everything they can to help you feel better and get you home faster. When you are feeling frustrated, try to think about what you can do today that you were unable to do yesterday. You have already come a long way!
The best way to make this an easier experience is to work together with the nurses, therapists, doctors and your family. Communicating with the care team will greatly benefit you and will help them take better care of you.
Everyone’s experience with pain after spinal fusion surgery is different. Your doctors, nurses and family all have the same goal: to help you be as comfortable as possible. Tension in your body and tightening of your muscles can make you hurt more, so it is very important to help yourself relax and stay as calm as possible. It is okay to ask for medicine for your pain when you need it. In fact, the medicine works best if you receive it before the pain becomes unbearable!
Pain After Spinal Fusion Surgery
Your nurse will frequently ask you the level of your pain. He or she will use what we call a "pain scale" from 0-10. The 0 represents no pain, while the 10 signifies pain that is the worst you’ve ever experienced. Your nurse may ask you to describe your pain with words such as sharp, burning, throbbing or dull. Please be honest with your nurses at all times. They are here to help keep you comfortable.
Here are some suggestions that have helped other kids and teens relieve pain after scoliosis surgery:
- Change your position.
- Channel your pain. Think about the pain moving out of your body or concentrate on another part of your body such as your thumb or elbow.
- Listen to relaxing music.
- Have someone wash your face or hair. Feeling calm and fresh makes a world of difference.
- Have someone read to you.
- Change the look and feel of your room. For example, turn off the lights, close the blinds and turn on a fan to cool you.
- Use breathing techniques. Taking slow deep breaths sometimes helps your body to relax.
- Get up and move around.
- Go for a short walk (with help of course!).
The most important thing you can do is to identify what helps you relax and then make a plan for yourself. Share your plan with a family member who will be at the hospital with you or write it down. Always keep a positive attitude; each day will get better!
4. Admission and The Day of Your Surgery
Admission
The first place you will go the day you are admitted is to Patient Access, located on the first floor. This is where you will check into the hospital.
Once you have checked in, you will be sent to the laboratory for blood and urine tests. This does involve a needle prick, but it only hurts a little and is over quickly. The information we get tells us how your body is working on the inside. You will also be given a small container and asked to give a urine sample. This tells us how your kidneys are working.
Next, you will go to the Radiology Department, also located on the first floor. Here you will have X-rays taken. X- rays are special photos taken of your body. X- rays do not hurt!
You will then go up to the second floor where you will be given your room assignment. You will be assigned to a room. This is your "home away from home" for the next few days. You will be introduced to your nurse and will have the opportunity to ask him/her any questions you may have at that time. You may change into a hospital gown or stay in your clothing, whichever you prefer. Your family can stay with you until you fall asleep for the night. Your room includes a "sleeper chair" so that a member of your family can spend the night with you. You may ask your nurse for extra pillows and blankets.
Remember: NO FOOD OR DRINK AFTER MIDNIGHT!
The Day of Your Surgery
On the morning of surgery a technician will come and tape electrodes on your legs. These electrodes are just stickers that have a plastic wire glued to them and will be used during surgery to measure the small electricity signals that our body makes to communicate with the brain. This does not hurt! The stickers peel off easily and will be all gone by the time you wake up.
The nerve pathways that are normal for you are recorded as wavy lines on a piece of paper. During your surgery, these pathways will be monitored to detect any changes.
Before you leave for the operating room, you will be given a medicine that will make you a little sleepy and a lot less nervous! This is not the medicine that helps you to fall asleep for your surgery.
You may bring something comforting to the operating room with you such as a stuffed animal, music, photo or other familiar item.
Once you are in the operating room, you will be given special medicine through a mask. This medicine is called anesthesia. The anesthesia mask will be placed over your nose and mouth. You will need to take a couple of deep breaths and you will be asleep in no time! All IVs and cathethers are put in after you’re asleep, so you wont feel a thing!
Recovery Room
When your surgery is finished, you will be taken to the PACU (Post Anesthesia Care Unit). You will still be sleeping. In this area, we will take an x-ray of your spine and obtain labs after surgery. You will also be monitored by a nurse who will determine when you are awake enough to return to your room. Your parents will be allowed to come and see you briefly. When you wake up in your room you will be connected to a vital sign monitor, IVs for fluids and pain medication and have a plastic drain to collect fluid from the incision.
4. Admission and The Day of Your Surgery
Admission
The first place you will go the day you are admitted is to Patient Access, located on the first floor. This is where you will check into the hospital.
Once you have checked in, you will be sent to the laboratory for blood and urine tests. This does involve a needle prick, but it only hurts a little and is over quickly. The information we get tells us how your body is working on the inside. You will also be given a small container and asked to give a urine sample. This tells us how your kidneys are working.
Next, you will go to the Radiology Department, also located on the first floor. Here you will have X-rays taken. X- rays are special photos taken of your body. X- rays do not hurt!
You will then go up to the second floor where you will be given your room assignment. You will be assigned to a room. This is your "home away from home" for the next few days. You will be introduced to your nurse and will have the opportunity to ask him/her any questions you may have at that time. You may change into a hospital gown or stay in your clothing, whichever you prefer. Your family can stay with you until you fall asleep for the night. Your room includes a "sleeper chair" so that a member of your family can spend the night with you. You may ask your nurse for extra pillows and blankets.
Remember: NO FOOD OR DRINK AFTER MIDNIGHT!
The Day of Your Surgery
On the morning of surgery a technician will come and tape electrodes on your legs. These electrodes are just stickers that have a plastic wire glued to them and will be used during surgery to measure the small electricity signals that our body makes to communicate with the brain. This does not hurt! The stickers peel off easily and will be all gone by the time you wake up.
The nerve pathways that are normal for you are recorded as wavy lines on a piece of paper. During your surgery, these pathways will be monitored to detect any changes.
Before you leave for the operating room, you will be given a medicine that will make you a little sleepy and a lot less nervous! This is not the medicine that helps you to fall asleep for your surgery.
You may bring something comforting to the operating room with you such as a stuffed animal, music, photo or other familiar item.
Once you are in the operating room, you will be given special medicine through a mask. This medicine is called anesthesia. The anesthesia mask will be placed over your nose and mouth. You will need to take a couple of deep breaths and you will be asleep in no time! All IVs and cathethers are put in after you’re asleep, so you wont feel a thing!
Recovery Room
When your surgery is finished, you will be taken to the PACU (Post Anesthesia Care Unit). You will still be sleeping. In this area, we will take an x-ray of your spine and obtain labs after surgery. You will also be monitored by a nurse who will determine when you are awake enough to return to your room. Your parents will be allowed to come and see you briefly. When you wake up in your room you will be connected to a vital sign monitor, IVs for fluids and pain medication and have a plastic drain to collect fluid from the incision.
5. What to Expect After Surgery
For the first three days after your spinal surgery, you will be on a special bed that turns you continuously, this bed is called a Hill-Rom Sport bed. The turning is done very slowly and you will usually stay in each position for about 15 minutes. This can be adjusted according to your comfort level. The only thing you have to do when being turned is RELAX, and tell us how we can position you more comfortably. Turning keeps you from getting stiff and helps to prevent pressure on your skin which can cause sore spots and the changing of position also helps your lungs stay in good condition.
Your Diet
You may not feel like eating at first. The day of your surgery, your nurse and your family may keep offering you something "clear" to eat or drink such as water, apple juice, popsicles, Jello® or Gatorade®. Eating and drinking helps you regain your strength more quickly.
The next morning, you will begin to eat regular food. You may eat whatever you like from the cafeteria or from outside the hospital. It is important that you eat because the pain medication that you will take by mouth will cause stomach pain, nausea and vomiting if taken on an empty stomach.
In order to prevent constipation and dehydration, it is important that you drink lots of fluids while in the hospital and at home.
Sitting, Standing, and Walking
Immediately after your scoliosis surgery your nurses will be helping you with any necessary movement, but by the time you are ready to go home, you will be walking out the door. How can this happen in less than a week? Your physical therapist is the key. He or she is the person who will help you and your family learn the correct way to move in bed, as well as to sit and walk properly. Together, you and your physical therapist will set goals for moving in bed, sitting up and walking.
You will meet your physical therapist the day after your surgery. Your physical therapist will talk to you and your family about moving in bed, sitting, standing and walking. Your therapist will assist you in sitting up on the edge of the bed. You will sit for several minutes to become accustomed to the change in position. The therapist will then help you to stand. You will stand for a few minutes while holding on to something to stabilize yourself. Deep breathing is often helpful when standing for the first time after surgery as it helps to relax your body and keep you calm. Day two is also the day you will begin to walk. The therapist will hold on to you to help keep you steady as you take a few steps. Your therapist will not make you walk farther than you can, but will ask you to set a goal to walk a little farther each time you get out of bed.
You will be walking more each day and will be able to venture out of your room, walk around the nurses’ station, down the hall, to the activity room located on the third floor, or as far as you can go.
Because the physical therapist will only visit you once or twice a day, your nurse will often be the one helping you to do these things. Try to remember, the key to feeling better faster and returning home sooner, is to get out of bed and keep moving!
Once you are able to get out of bed and walk with the help of your family, you will be able to get up when you want to and soon will no longer need assistance each time you want to go for a walk.
Respiratory Therapy
It is important to keep your lungs healthy after surgery. When you return to your room after surgery, you will meet another important team member. The respiratory therapist will provide you with breathing treatments (medication you breathe in) to help you expand your lungs. Your nurse will also be reminding you to take deep breaths for several days after your surgery. You will be given a device called an incentive spirometer. This helps your lungs expand and keeps them clear and working at their best. You may get tired of everyone reminding you to use the spirometer. Please remember that it is important that you do as requested. Regular use of the spirometer is the best way to prevent fevers and avoid complications such as pneumonia.
The best way to make this an easier experience is to work together with the nurses, therapists, doctors and your family. Communicating with the care team will greatly benefit you and will help them take better care of you.
5. What to Expect After Surgery
For the first three days after your spinal surgery, you will be on a special bed that turns you continuously, this bed is called a Hill-Rom Sport bed. The turning is done very slowly and you will usually stay in each position for about 15 minutes. This can be adjusted according to your comfort level. The only thing you have to do when being turned is RELAX, and tell us how we can position you more comfortably. Turning keeps you from getting stiff and helps to prevent pressure on your skin which can cause sore spots and the changing of position also helps your lungs stay in good condition.
Your Diet
You may not feel like eating at first. The day of your surgery, your nurse and your family may keep offering you something "clear" to eat or drink such as water, apple juice, popsicles, Jello® or Gatorade®. Eating and drinking helps you regain your strength more quickly.
The next morning, you will begin to eat regular food. You may eat whatever you like from the cafeteria or from outside the hospital. It is important that you eat because the pain medication that you will take by mouth will cause stomach pain, nausea and vomiting if taken on an empty stomach.
In order to prevent constipation and dehydration, it is important that you drink lots of fluids while in the hospital and at home.
Sitting, Standing, and Walking
Immediately after your scoliosis surgery your nurses will be helping you with any necessary movement, but by the time you are ready to go home, you will be walking out the door. How can this happen in less than a week? Your physical therapist is the key. He or she is the person who will help you and your family learn the correct way to move in bed, as well as to sit and walk properly. Together, you and your physical therapist will set goals for moving in bed, sitting up and walking.
You will meet your physical therapist the day after your surgery. Your physical therapist will talk to you and your family about moving in bed, sitting, standing and walking. Your therapist will assist you in sitting up on the edge of the bed. You will sit for several minutes to become accustomed to the change in position. The therapist will then help you to stand. You will stand for a few minutes while holding on to something to stabilize yourself. Deep breathing is often helpful when standing for the first time after surgery as it helps to relax your body and keep you calm. Day two is also the day you will begin to walk. The therapist will hold on to you to help keep you steady as you take a few steps. Your therapist will not make you walk farther than you can, but will ask you to set a goal to walk a little farther each time you get out of bed.
You will be walking more each day and will be able to venture out of your room, walk around the nurses’ station, down the hall, to the activity room located on the third floor, or as far as you can go.
Because the physical therapist will only visit you once or twice a day, your nurse will often be the one helping you to do these things. Try to remember, the key to feeling better faster and returning home sooner, is to get out of bed and keep moving!
Once you are able to get out of bed and walk with the help of your family, you will be able to get up when you want to and soon will no longer need assistance each time you want to go for a walk.
Respiratory Therapy
It is important to keep your lungs healthy after surgery. When you return to your room after surgery, you will meet another important team member. The respiratory therapist will provide you with breathing treatments (medication you breathe in) to help you expand your lungs. Your nurse will also be reminding you to take deep breaths for several days after your surgery. You will be given a device called an incentive spirometer. This helps your lungs expand and keeps them clear and working at their best. You may get tired of everyone reminding you to use the spirometer. Please remember that it is important that you do as requested. Regular use of the spirometer is the best way to prevent fevers and avoid complications such as pneumonia.
The best way to make this an easier experience is to work together with the nurses, therapists, doctors and your family. Communicating with the care team will greatly benefit you and will help them take better care of you.
8. Going Home, and School Re-entry
Going Home
Hooray! This is the day you have been working toward, and it is a very exciting time. You should know that along with all the excitement you may also have some feelings of discouragement. You may feel very weak and tired. It might be hard to find a comfortable position. You may not have much of an appetite. If you do, watch what you eat. Your stomach will be sensitive. Remember to eat before you take your medicine. You may have itching around or inside the incisions. When you are finally able to take a full shower, you will feel like a new person.
When you get home from the hospital, have your room or the place you will be sleeping ready and waiting for you. Have a table next to you with things you like and might need such as a phone, something to drink, an MP3 player, a laptop or a CD player, and of course, the TV remote control!
Enjoy being home. You have worked extremely hard to get there. Feel good about all you have accomplished.
School Re-entry
Depending upon the time of your surgery, you may need to think about returning to school shortly after you get home from the hospital. It is very important to set up a time to meet with each of your teachers to go over your surgery. A school re-entry letter is provided upon request, ask your Child Life Specialist. Accommodations will also be reviewed so that everyone is made aware of the special needs you may have. No backpacks! You should not be carrying anything more than five pounds. You may also want to consider a gradual return to school starting with half days and working your way toward full days.
Make sure you share these helpful ideas with your teachers and school so that a plan is in place before your surgery.
Tips for Parents to Prepare for the Return to School
It is very important that you contact your child’s teachers and school before surgery to create a plan and make sure that everyone involved with your child has the same information and expectations.
- Be sure all home schooling paperwork is signed before surgery.
- Arrange to get assignments from your child’s teachers.
- Arrange for your child to leave class five or 10 minutes early in order to get to the next class safely.
- Arrange an excuse from physical education.
- Request two sets of books, one for school and one for home.
- Inform the school of your child’s absence and surgery prior to the surgery so adjustments can be made in the attendance policy.
- Request access to elevators.
- Consider a shortened school day when you child first returns to school and gradually work up to a full day.
- Ask your Child Life Specialist for a school re-entry letter.
8. Going Home, and School Re-entry
Going Home
Hooray! This is the day you have been working toward, and it is a very exciting time. You should know that along with all the excitement you may also have some feelings of discouragement. You may feel very weak and tired. It might be hard to find a comfortable position. You may not have much of an appetite. If you do, watch what you eat. Your stomach will be sensitive. Remember to eat before you take your medicine. You may have itching around or inside the incisions. When you are finally able to take a full shower, you will feel like a new person.
When you get home from the hospital, have your room or the place you will be sleeping ready and waiting for you. Have a table next to you with things you like and might need such as a phone, something to drink, an MP3 player, a laptop or a CD player, and of course, the TV remote control!
Enjoy being home. You have worked extremely hard to get there. Feel good about all you have accomplished.
School Re-entry
Depending upon the time of your surgery, you may need to think about returning to school shortly after you get home from the hospital. It is very important to set up a time to meet with each of your teachers to go over your surgery. A school re-entry letter is provided upon request, ask your Child Life Specialist. Accommodations will also be reviewed so that everyone is made aware of the special needs you may have. No backpacks! You should not be carrying anything more than five pounds. You may also want to consider a gradual return to school starting with half days and working your way toward full days.
Make sure you share these helpful ideas with your teachers and school so that a plan is in place before your surgery.
Tips for Parents to Prepare for the Return to School
It is very important that you contact your child’s teachers and school before surgery to create a plan and make sure that everyone involved with your child has the same information and expectations.
- Be sure all home schooling paperwork is signed before surgery.
- Arrange to get assignments from your child’s teachers.
- Arrange for your child to leave class five or 10 minutes early in order to get to the next class safely.
- Arrange an excuse from physical education.
- Request two sets of books, one for school and one for home.
- Inform the school of your child’s absence and surgery prior to the surgery so adjustments can be made in the attendance policy.
- Request access to elevators.
- Consider a shortened school day when you child first returns to school and gradually work up to a full day.
- Ask your Child Life Specialist for a school re-entry letter.
Media Relations
Media members needing information about Nicklaus Children's Hospital should contact our Public Relations Department.
Please be advised that patient information will only be shared if a patient consents in accordance with the patient confidentiality policy of Nicklaus Children's Hospital.
For after-hours service, please call 305-666-6511 and ask the operator for the marketing representative on call.
Video Center
Events
Nicklaus Children's Hospital extends its expertise through its educational offerings to the community providing classes and courses, in addition to family-centered services to parents, families and professionals. Browse our community calendar to discover which upcoming events you would like to attend.
Awards & Recognitions
Online Communities - Social Media Pages
Apps
Nicklaus Children's Patient Portal
The Nicklaus Children's Hospital's Patient Portal. The Patient Portal gives parents access to their discharge instructions, lab results, medications, medical diagnoses, online bill pay, and secure messaging with select doctor's practices. Parents receive an invitation to their child's Patient Portal account via the email they provide at registration.
Learn More
My Nicklaus Children's
My Nicklaus Children's app – now available in app stores – helps families access our hospital and health system service locations, pediatric health library content, virtual care services as well as receive real-time alerts. The digital platform features physician directories, appointment scheduling, patient records, bill pay options and enables families to verify hours, locations and wait times for urgent care centers.
Gozio Health's patented indoor wayfinding with turn-by-turn navigation to help families find their way to hospital departments and physician offices, as well as on-site hospital amenities, such as dining options, restrooms, ATMs, the gift shop and more.
GET Mobile
You can now order items for delivery to a child's room from our Gift Shop and the Golden Cub Café! The GET app enables you to purchase and order from our Nicklaus Children's Gift Shop and Golden Cub Café from your mobile device. You can also order from our Miracles Café but only pick-up is available. You can view individual menus and gift shop offerings via the GET app or by visiting the GET website. It is easy to select and customize your order, and even choose the time and date of delivery. Follow these steps to get started:
- Download the GET app from Google Play or the App Store.
- Select Nicklaus Children's Hospital as your institution and create an account.
- Add a credit card to begin your purchase or food order from your device.
For more information, please visit the GET app FAQ.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.
Connect to your Health Management Apps
Nicklaus Children's Hospital will soon offer the ability for you to securely connect your health record to some of the health management apps you may use (i.e. fitness trackers, dietary trackers, etc.). This new process provides access to your health and wellness data in an app of your choosing that will enable you to make informed choices.
If you are interested in connecting an app – contact us at smartapps@nicklaushealth.org – be sure to include your Name, Phone Number, Email, and App Name. Once we receive your request, we will be in touch (typically within 3-5 business days) with next steps.
Available Health Apps:
- Apple iOS Health App Integration - Coming Soon!
Apps
Nicklaus Children's Patient Portal
The Nicklaus Children's Hospital's Patient Portal. The Patient Portal gives parents access to their discharge instructions, lab results, medications, medical diagnoses, online bill pay, and secure messaging with select doctor's practices. Parents receive an invitation to their child's Patient Portal account via the email they provide at registration.
Learn More
My Nicklaus Children's
My Nicklaus Children's app – now available in app stores – helps families access our hospital and health system service locations, pediatric health library content, virtual care services as well as receive real-time alerts. The digital platform features physician directories, appointment scheduling, patient records, bill pay options and enables families to verify hours, locations and wait times for urgent care centers.
Gozio Health's patented indoor wayfinding with turn-by-turn navigation to help families find their way to hospital departments and physician offices, as well as on-site hospital amenities, such as dining options, restrooms, ATMs, the gift shop and more.
GET Mobile
You can now order items for delivery to a child's room from our Gift Shop and the Golden Cub Café! The GET app enables you to purchase and order from our Nicklaus Children's Gift Shop and Golden Cub Café from your mobile device. You can also order from our Miracles Café but only pick-up is available. You can view individual menus and gift shop offerings via the GET app or by visiting the GET website. It is easy to select and customize your order, and even choose the time and date of delivery. Follow these steps to get started:
- Download the GET app from Google Play or the App Store.
- Select Nicklaus Children's Hospital as your institution and create an account.
- Add a credit card to begin your purchase or food order from your device.
For more information, please visit the GET app FAQ.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.
Connect to your Health Management Apps
Nicklaus Children's Hospital will soon offer the ability for you to securely connect your health record to some of the health management apps you may use (i.e. fitness trackers, dietary trackers, etc.). This new process provides access to your health and wellness data in an app of your choosing that will enable you to make informed choices.
If you are interested in connecting an app – contact us at smartapps@nicklaushealth.org – be sure to include your Name, Phone Number, Email, and App Name. Once we receive your request, we will be in touch (typically within 3-5 business days) with next steps.
Available Health Apps:
- Apple iOS Health App Integration - Coming Soon!
Annual Reports
Every year, Nicklaus Children's Health System publishes a financial summary of a company’s activities during the previous year in the Annual Report. This detailed report highlights the financial standing of the health system as well as community outreach efforts, achievements, philantrophic support received and the impact our services have in the community.
Planning Your Visit
At Nicklaus Children's, we understand that a trip to the hospital can be an emotional experience for parents and their children. Being informed about what to expect during a hospital visit can help reduce stress for the patient and the entire family.
All visitors should follow the safety and visitation guidelines in order to ensure the safety and confidentiality of our patients.
General Hospital Visitation Hours:
9 a.m. - 9:30 p.m.
We continue to use protocols recommended by the Centers for Disease Control regarding the novel COVID-19 virus. Our priority, as always, is the health and safety of all our patients and visitors. Due to the current higher-than-usual rate of respiratory infections in our community, please note we are reinforcing changes to our visitor policy in all our care settings. We ask patient families to adhere to the following practices to ensure the safety of the children in our care.
Please read the protocols below prior to your visit
EXPAND TO READ ALL VISITATION PROTOCOLS
Safety Protocols for All Visits
- All parents/guardians accompanying children must be free of signs and symptoms of infectious disease, including cough, runny nose, rash, vomiting and fever. Please notify the medical provider caring for your child if you or anyone else in the home has a fever, cough, rash, shortness of breath, or any other sign of respiratory infection.
- Please remember to wash your hands or use alcohol gel frequently during your visit.
For Inpatient Visits
- Parents or guardians are welcome to be with hospitalized patients at all times. Family and friends are encouraged to visit between 9 a.m. and 9:30 p.m. The number of visitors should be limited to no more than four at a time in most units to enable patients to rest.
- During flu season, and when the incidence or respiratory illness in the community is high, visitors are restricted to parents, healthy siblings and other designated visitors.
- No one experiencing symptoms of illness should visit the hospital. Please check with your child's care unit for any special policies that may apply.
For Emergency Room, Urgent Care, Radiology and Diagnostic Services
- For the safety of all, we are limiting the number of people within exam spaces and in diagnostic areas.
- A maximum of two primary caregivers can accompany a patient for any of the above services.
- Additional family members may take turns within the exam room, but only two may be in the room at a time.
For Rehabilitation Services
- For the safety of all in our shared rehabilitation service gyms, we ask that only one primary caregiver accompany a patient to an appointment.
For Ambulatory Surgery Visits
- Only two visitors can accompany the patient. Only one of these is permitted at the bedside at a time, while the other waits in the waiting room. The two can alternate at the bedside. No one under the age of 18 is permitted.
For Neonatal Intensive Care Unit (NICU) Visits
Due to this risk and the increase in upper respiratory infections in our community during the winter season, Nicklaus Children’s Hospital Neonatal Intensive Care Unit (NICU) has modified its visitation policy. During this time, November 1 through March 31, we ask that only parents/guardians and grandparents visit patients in the NICU.
- Please cooperate with unit screening procedures. A form may be filled out that helps screen for infectious diseases.
- Parents must wear visitor ID.
- Parents must be free of cold or “flu symptoms.”
- Visitors to the NICU are strongly encouraged to receive influenza vaccine.
- Please notify the nurse caring for your child if you or anyone else in the home has a fever, cough, or any other sign of infection.
- Remember to wash your hands or use alcohol gel frequently during your visit.
We apologize for the any inconvenience and thank you for partnering with us in providing your child the best possible care and protection.
General Guidelines for Visitors
Family Centered Care through visitation is promoted at Nicklaus Children's Hospital. Family members are partners in our mission to provide the best, safest care possible. Please follow these guidelines when planning to visit a hospitalized child:
- Parents, adult primary caregivers, grandparents, extended family, and friends are welcome to visit during general visitation hours.
- All visitors should be in good health and free from symptoms of contagious disease and known exposures (flu, chicken pox, etc).
- Intensive Care Units, Bone Marrow Transplant, Special Care Nurseries, Surgical Services and Psychiatry have more restrictive guidelines about visitation. Please notify the nurse for assistance on visitation requirements into these areas.
Guidelines for Children Visiting the Hospital
- Children under 12 years of age may visit given that they are under adult supervision at all times.
Patient Visitation Policy
Download the detailed guidelines and procedures regarding the Nicklaus Children's Hospital visitation policies. Last updated September 2023.
Download PDF
Equal Visitation
Nicklaus Children's Hospital is committed to provide visitation in accordance with our non-discrimination policy which provides access without regard to race, color, sex, national origin, disability, age, religion, marital status, citizenship, gender identity, gender expression, sexual orientation, and/or other legally protected classification.
Fast-Pass Visitor Identification
All visitors to inpatient units and the Emergency Department at Nicklaus Children's Hospital – including parents, siblings, family and friends – must receive a Fast-Pass photo identification pass upon arrival, and wear the peel-and-stick pass throughout the visit.
What You'll Need
To obtain a Fast-Pass, visitors must present a current identification (driver's license, state ID, student ID, or passport) at any information desk entrance. Visitors to inpatient units should return their Fast-Pass to the location where they received it when departing the hospital.
- Inpatient Visits: The Fast-Pass is valid for a 24-hour period. Visitors to most inpatient units, including parents staying overnight, will need to obtain a new pass daily.
- Doctor and Outpatient Visits: A Fast-Pass identification is not needed for those visiting physician offices or outpatient services other than the Emergency Department.
- Visitor Limits: Staff issuing the Fast-Pass will receive an alert if the number of visitors to a patient room has exceeded hospital limits for the unit. For most units, no more than four visitors are allowed at one time. Families will have the option to have some visitors rotate out of the room to allow arriving visitors access.
Adaptive Care Program
For some children with behavioral or developmental needs, including many on the autism spectrum, a hospital visit can be challenging. At Nicklaus Children's Hospital, our inpatient Adaptive Care Program supports the needs of our neurodivergent population and other eligible children.
This inpatient program is offered to families of children over the age of 3 who have difficulty coping during hospitalization, or have sensory, behavioral, or communicative needs. If your child would benefit from the Adaptive Care Program, please contact AdaptiveCareTeam@nicklaushealth.org prior to an inpatient hospitalization, so our team can work with you to develop the best plan to support for child’s needs. Our Adaptive Care Patient Resources can also help you plan for a more comfortable experience for your child before, during, and after their hospital visit or stay.
The University of Miami-Nova Southeastern University Center for Autism and Related Disabilities (UM-NSU CARD), South Florida’s leading resource for autism support, recognizes Nicklaus Children’s Hospital as an Autism Friendly Partner.
Guest Parking
As you plan your visit to the hospital campus, we'd like to help you by providing suggested parking instructions. The hospital's My Nicklaus Children's app offers detailed instructions to our campus and detailed step by step directions once you have arrived and parked. We encourage you to download this app.
There are three separate garages on the hospital campus, each identified by a color, blue, green and yellow. Their use is entirely complimentary. Complimentary valet service is offered 24-hours a day at the entrance of the Central Building, near the Devonshire Boulevard entrance to the campus. Additional complimentary valet services are available during select hours in the blue and yellow garages. For more information visit our hospital parking page.

Campus Ride Sharing Stops
Designated stops are available for ride sharing and retail deliveries. See our map for more information on the stops in our campus.
Ride Sharing Stops
Patient and Guest Relations
Patient and Guest Relations representatives are available to assist patients and families by answering questions, explaining hospital policies, customer service and helping to resolve issues related to hospital services.
Representatives help families understand their rights and responsibilities and assist in the resolution of complaints, grievances, and treatment disagreements. They are also part of the multi-disciplinary team of care for patients and families and are available to work with families who express concerns about the hospital, its staff and its services.
To contact a Patient and Guest Relations representative, please call 786-624-4400.
Mask Wearing Requirements for all Nicklaus Children’s Facilities
As of August 1, 2023, masks are required only in certain circumstances. Examples include persons exhibiting signs or symptoms of an infectious disease, in areas of the facility that are designated sterile, or if the applicable person will be around an immunocompromised patient. This policy applies to all Nicklaus Children's staff members, patients, and visitors two years of age and older. Patients and visitors can contact the patient’s healthcare team (e.g., the treating provider’s office or inpatient unit) and staff members can contact the Infection Prevention and Control Department at ext. 2399.
For More Information
Community Events, Workshops and Support Groups
Nicklaus Children's Hospital extends its expertise through its
educational offerings to the community providing classes and courses, in addition to family-centered services to parents, families and professionals.
Browse our
community calendar to discover upcoming events to attend and learn more about Nicklaus Children's Hospital program offerings.
Health and Safety Information
Medical Records
Health Information Management (HIM)
The Nicklaus Children's Hospital Health Information Management Department is committed to respecting and protecting the rights of our patients and families. The Health Information Management staff is responsible for maintaining the confidentiality of all patient records and will be pleased to serve you with your medical records requests. Parents, guardians or patients have the right to either review or receive a copy of their child's medical records when authorized. Medical records are retained for a period of ten (10) years after your last date of service. Please note we cannot interpret what the information means or discuss it with you.
If you have additional questions after reading the information below, you may contact the HIM Department.
How To Obtain Medical Records via My Nicklaus Children's Patient Portal
Access portions of your child's medical record by accepting an email invitation to enroll in the My Nicklaus Children's Patient Portal. For access, email mykidsportal@nicklaushealth.org.
For medical records not available on the portal, refer to instructions below.
How to Request Medical Records Online (eRequest)
Request medical records via secure website hosted by our release of information partner, Datavant (formerly Ciox). If you are unable to complete request online, refer to additional options to submit your medical records request.
Please note: Complete authorization form if requesting psychiatry/psychology records or sensitive laboratory results (HIV/STD/Drug Screen/Pregnancy), as additional signature is required.
Where To Submit Your Medical Record Request
Completed authorization for release/request of information form, along with copy of photo ID, can be emailed to HIM.releaseofinformation@nicklaushealth.org or mailed to:
Nicklaus Children's Hospital
Medical Records Department
3100 SW 62 Avenue
Miami, Florida 33155
Note: We do not accept faxed requests and if the patient is now 18 years of age or older, they are the only person who can authorize the release of their medical records.
How to Request Radiology Images
For radiology images performed at the main hospital, please call the Nicklaus Children's Hospital Radiology Department at 786-624-3283. The completed authorization for release/request of information and copy of picture ID is required.
Please note: If radiology exams were performed at the outpatient centers, you must request images directly from the center.
Charges For Obtaining Copies of Medical Records
One courtesy copy is provided. There will be a charge for additional copies.
Receiving Your Requested Records
Once the HIM Department receives your request, it will take approximately 5 to 7 business days for the records to be mailed to the address you provided. You can receive records via email, if electronic record delivery request form was completed. RECORDS WILL NOT BE FAXED.
How to Request an Amendment to a Medical Record
Nicklaus Children's Hospital will grant the patient the right to amend their Protected Health Information (PHI) according to federal and state regulations.
Your Right to Make a Request
If you are requesting an amendment or correction to your or your child's PHI, complete the PHI Amendment/Correction Request form and send via email to HIM.releaseofinformation@nicklaushealth.org or mail it to the address listed above. Please include a copy of photo ID with the request.
Processing and Considering the Request
Once you have completed and submitted the request for amendment/correction the Health Information Management Director or designee will respond to your request no later than 60 days by:
- Processing the requested amendment
- Providing the patient with a written denial
- Providing the patient with a written statement of the reasons for the delay and the date by which Nicklaus Children's Hospital will respond to the request (which date may not be later than 90 days after receipt of the request).
Additional Resources
For billing records, please contact 305-663-8452 and select option 2.
Family-Centered Care Services
As healthcare professionals dedicated to providing the best care for each of our patients, the staff at Nicklaus Children's Hospital recognizes the essential role that families play in the health and wellbeing of the child. As pediatric health specialists, we realize that family members are the main source of support and strength for a child in the hospital. Because of this, every department and program at Nicklaus Children's Hospital is committed to supplying a truly family-centered care environment.
As part of our commitment to Family-Centered Care, many units at Nicklaus Children's promote family and patient participation in medical rounds. These Family-Centered Care Rounds ensure that families are actively involved in daily care team discussions related to the child’s treatment.
To learn more about a few of our departments and programs whose primary focus is on supporting the child and family both while admitted to the hospital and after they have returned to the home environment, please choose one of the links from the navigation bar on the left.
Chaplain and All Faiths Chapel
Our chaplains provide pastoral care services to patients, families and staff and assist them spiritually when they face difficult medical conditions.
Learn more
Child Life
Child Life specialists strive to normalize the hospital environment by providing psychosocial therapeutic support through a family centered care approach.Their goal is to enrich the experience for our patients and their families.
Learn more
Family Advisory Council
The council's mission is to work in partnership with hospital staff to promote the delivery of Patient and Family Centered Care. FAC members identify the needs and priorities of patients and families and work on annual goals that will benefit families coming to Nicklaus Children's Hospital.
Learn more
Social Work Services
Social workers actively collaborate with the multidisciplinary team and provide the following services to patients and their families, crisis intervention, case management, short-term individual and family counseling, discharge planning, and many other aspects of hospitalization.
Learn more
Did We Go the Extra Mile?
Want to recognize someone on your child’s care team who made a difference during your stay? You can share feedback by completing a “Did I go the Extra Mile?” form and placing it in the recognition boxes located within hospital units.
Patient Information Privacy and Security (HIPAA)
The Health Insurance Portability and Accountability Act (HIPAA) was enacted in 1996 and provides federal protections for personal health information held by covered entities like Nicklaus Children's Hospital and gives patients certain rights with respect to that information. HIPAA is enforced by the Office for Civil Rights (OCR).
There are two sections which work together to protect patients: (1) HIPAA Privacy Rule and (2) HIPAA Security Rule.
What Information is Protected?
Protected Health Information (PHI) is:
- Individually identifiable health information created, received, transmitted or maintained by a covered entity such as Nicklaus Children's Hospital that links an identifiable person with their health condition.
- Information, including demographic information, that relates to:
- An individual’s past, present or future health condition;
- Providing health care to an individual; or
- The past, present, or future payment for providing health care to an individual
- AND that identifies or is reasonably believed to identify an individual.
It may be in many formats:
- Paper or hard copy: records, labels, x-rays, films, letters
- Electronic: computerized, digitized, video, audio
- Communication: verbal, sign language (conveying a message from one individual to another
HITECH
Health Information Technology for Economic and Clinical Health Act (HITECH) added a breach notification requirement to HIPAA. The laws regarding HIPAA were updated through the American Recovery and Reinvestment Act (ARRA), which requires more enforcement and increased penalties. In addition, the recently implemented Final Omnibus Rule requires further changes to some aspects of our procedures.
There is a key change in the definition of a breach as well as the breach notification requirement.
An impermissible use or disclosure of protected health information is presumed to be a breach UNLESS the covered entity or business associate, as applicable, demonstrates that there is a low probability that the protected health information has been compromised.
Covered entities are required to notify patients if there is a breach unless after completing a risk analysis, it is determined that there is a low probability of compromise of the PHI.
- Must provide notification to patients no later than 60 days after the date of discovery
- Must notify the HHS Secretary:
- immediately if more than 500 affected
- at the end of each year if less than 500
A substitute notice is required if there is insufficient or out of date contact information.
Florida’s Health Information Privacy Laws
Florida Statutes provide extra protections for individuals with respect to their health information and social security numbers.
There are enhanced protections under Florida Law for “highly confidential information”:
- Mental Health (psychotherapy notes)
- Substance/Alcohol Abuse Treatment
- STD/HIV/AIDS Test Results, Records or Treatment
- Domestic Violence Related Treatment
Florida’s laws governing health records for these types of information are more stringent that HIPAA and will override HIPAA.
Patient Information Privacy and Security (HIPAA)
The Health Insurance Portability and Accountability Act (HIPAA) was enacted in 1996 and provides federal protections for personal health information held by covered entities like Nicklaus Children's Hospital and gives patients certain rights with respect to that information. HIPAA is enforced by the Office for Civil Rights (OCR).
There are two sections which work together to protect patients: (1) HIPAA Privacy Rule and (2) HIPAA Security Rule.
What Information is Protected?
Protected Health Information (PHI) is:
- Individually identifiable health information created, received, transmitted or maintained by a covered entity such as Nicklaus Children's Hospital that links an identifiable person with their health condition.
- Information, including demographic information, that relates to:
- An individual’s past, present or future health condition;
- Providing health care to an individual; or
- The past, present, or future payment for providing health care to an individual
- AND that identifies or is reasonably believed to identify an individual.
It may be in many formats:
- Paper or hard copy: records, labels, x-rays, films, letters
- Electronic: computerized, digitized, video, audio
- Communication: verbal, sign language (conveying a message from one individual to another
HITECH
Health Information Technology for Economic and Clinical Health Act (HITECH) added a breach notification requirement to HIPAA. The laws regarding HIPAA were updated through the American Recovery and Reinvestment Act (ARRA), which requires more enforcement and increased penalties. In addition, the recently implemented Final Omnibus Rule requires further changes to some aspects of our procedures.
There is a key change in the definition of a breach as well as the breach notification requirement.
An impermissible use or disclosure of protected health information is presumed to be a breach UNLESS the covered entity or business associate, as applicable, demonstrates that there is a low probability that the protected health information has been compromised.
Covered entities are required to notify patients if there is a breach unless after completing a risk analysis, it is determined that there is a low probability of compromise of the PHI.
- Must provide notification to patients no later than 60 days after the date of discovery
- Must notify the HHS Secretary:
- immediately if more than 500 affected
- at the end of each year if less than 500
A substitute notice is required if there is insufficient or out of date contact information.
Florida’s Health Information Privacy Laws
Florida Statutes provide extra protections for individuals with respect to their health information and social security numbers.
There are enhanced protections under Florida Law for “highly confidential information”:
- Mental Health (psychotherapy notes)
- Substance/Alcohol Abuse Treatment
- STD/HIV/AIDS Test Results, Records or Treatment
- Domestic Violence Related Treatment
Florida’s laws governing health records for these types of information are more stringent that HIPAA and will override HIPAA.
Patient and Guest Relations
Patient and Guest Relations representatives are available to assist patients and families by answering questions, explaining hospital policies, customer service and helping to resolve issues related to hospital services.
Representatives help families understand their rights and responsibilities and assist in the resolution of complaints, grievances, and treatment disagreements. They are also part of the multi-disciplinary team of care for patients and families and are available to work with families who express concerns about the hospital, its staff and its services.
Chaplain and All Faiths Chapel
Chaplain's Services
Our chaplains provide pastoral care services to patients, families and staff and assist them spiritually when they face difficult medical conditions.
Some of the services that our chaplains provide include:
- Spiritual support through prayer, guidance and ongoing bereavement care to patients and families
- Serve as a resource by supporting patients, families and staff in their faith traditions and contacting their faith leaders
- Provide the Sacraments and meet other spiritual needs of patients and families
- Daily prayers for all patients and their families.
Visiting Our Chaplain
Patients, families and staff are welcome to stop by any time to talk with the chaplain. The chaplain's office is located on the first floor across from the All Faiths Chapel. You may contact our chaplains by calling extension 4404 (786-624-4404), or extension 4472 (786-624-4472), you may ask your nurse, social worker, or operator to contact them.
A chaplain is available in the hospital weekdays from 7 a.m. to 3 p.m.; however, an on-call chaplain is always available for emergencies by pager or through the operator. The chapel is located on the first floor along the hallway west of the cafeteria, and is available for people of all faiths to use for personal prayer and meditation. The chapel is also accessible for observance of diverse interfaith religious holidays throughout the year, as well as for specific patient or staff related services. The chaplain's office is located directly across from the chapel, and a phone is available outside the office to leave messages for the chaplain.
The Nicklaus Children's Hospital chaplain is also available as a resource to hospital staff in need of pastoral services.
An interfaith chaplain is available for the spiritual and emotional needs of patients and families and visits those patients/families who have requested the chaplain upon admission or during their hospitalization. The chaplain also participates in various multidisciplinary rounds and patient care conferences, and documents all pastoral care visits. Sacraments performed at patient's/family's request and referrals made to other disciplines are documented in the patient's medical records.
The Chaplaincy Department also plans, coordinates and conducts worship services within the hospital on major religious holidays throughout the year. The chaplain leads daily healing prayer services for families and staff in the hospital chapel, administers religious rites, sacraments and celebrations in accordance with the faith and traditions of patients and families, while also serving as a liaison with community and visiting clergy.
Red Nose Docs
Nicklaus Children's Hospital is thrilled to have a healthcare clowning partner in Healthy Humor, Inc.!
Red Nose Docs offers the magic of healthcare clowns to alleviate the stress for young patients, their families and their circle of caregivers. Using an array of circus and theater skills, the professional, specially-trained performers work in teams of two to create spontaneous, joyful encounters, reintroducing play and fun as natural parts of life.
Healthy Humor’s founders have more than 50 years of combined experience in healthcare clowning.
Our silly and lovable clowns are:
- Dr. Billy
- Dr. Rocker
- Dr. Waffles
- Dr.Bumbles
- Nurse LuLu
- Dr. Purple
- Dr. Schpack
Financial Services
In an effort to best serve you in addressing your financial responsibility and medical coverage when seeking services at our facility, we have included information in this section of the website to help you to better seek additional details about the cost of pediatric healthcare and understand your co-pays and how we can be of further assistance.
Financial Assistance Policy
The Financial Assistance Policy assures that patients who are unable to pay hospital charges are evaluated for financial assistance eligibility on a nondiscriminatory basis. The policy is consistent with the mission and values of Nicklaus Children’s Hospital and takes into account each patient’s ability to pay the cost of his or her care. Nicklaus Children’s Hospital is committed to ensuring a financially sound organization so that it may continue to provide outstanding medical care with a highly skilled work force employing the latest advances.
Florida Pricing Transparency
Nicklaus Children's Hospital believes you have the right to understand your healthcare options and the cost of care. Posted prices are general estimates and do not reflect your personal financial responsibility. The prices provided on this website and our facilities are an estimate of charges for most hospital services without complications. There may be variations to prices based on services received (i.e. surgery time) as well as additional supporting areas required (i.e. anesthesia, radiology, etc.). Your final bill will include charges for the actual services provided to you and your financial responsibility.
Please note that physicians and private ancillary services will bill separately from the hospital. If you are covered by health insurance, we encourage you to contact your insurance company to confirm benefit information under your policy, for a particular health care service provided at this facility. To confirm financial responsibility, please click here to submit a quote request.
If you are not covered by health insurance, you are strongly encouraged to contact our Financial Counselor to discuss payment options prior to receiving services from the hospital. For more information, please call 305-669-6525 or email EAS@nicklaushealth.org.
To view our ChargeMaster files please visit our Pricing and Estimates section.
For comparison of pricing with that of other facilities, please visit missiontocare.org
New! Price Estimator Tool
View pricing estimates for the most common hospital services and procedures.
FloridaHealthFinder.Gov Price Information
Service bundles are non-personalized and actual costs are based on the services received. For more information on service bundles, please visit, pricing.floridahealthfinder.gov
Contracted Providers Billing Separately
Patient families should contact the providers they anticipate will be providing treatment regarding the insurance they accept and request a personalized estimate, since they will be billing separately from the hospital bill. These independently contracted providers can include surgeons, radiologists, anesthesiologists, emergency department physicians, and pathologists. To contact one of these providers, please visit our Contracted Partners and Physician Directory.
Pet Therapy
Social Work Services
Social workers actively collaborate with the multidisciplinary team and provide the following services to patients and their families:
- Psychosocial assessment and goal oriented treatment planning
- Crisis intervention
- Short-term individual and family counseling
- Discharge planning
- Patient/team conferences
- Case management
- Parent support groups
- Information and referral
- Identification of, and appropriate intervention with, child abuse/neglect cases as well as with domestic violence cases
- Patient/family education and staff in-services
- Assistance with Advance Directives and DNR process
- Grief/bereavement counseling
- Assistance with complex funeral/burial arrangements
- Interventions with diverse systems outside Nicklaus Children's Hospital
- Post-mortem conference coordination
- Short-term post-discharge phone or outpatient follow-up
Hours of Service
Social Work Services are available to patients and famlies:
Monday – Sunday from 8:30 a.m. to midnight.
The evening social worker on duty can always be reached via the operator. There is always an off-site, on-call social worker from 11 p.m. to 8:30 a.m. The on-call social worker is available by pager for phone consultations as well as for in-person response to complex cases. All Nicklaus Children's Hospital social workers hold MSW degrees and many are Florida licensed.
Children's and Family Experiences

Child Life

Music Therapy

Recreation
The Children's Experiences team consists of:
Recreational Experience and Play Spaces
These family-friendly play spaces, located throughout the hospital, offer our guests a normalized environment within the hospital setting. Children of all ages and their families are encouraged to leave the bedside and are welcomed to participate in scheduled therapeutic and expressive activities, such as music therapy drum circles, Child Life medical play sessions and expressive arts group sessions. In addition, our teams understand the importance of recreation and offer dedicated play hours, in which patients and siblings are empowered to engage in play of their choosing. Toddlers and preschoolers may engage in sensory activities or “pretend” play, while teens may enjoy video games, guided arts and crafts or board game tournaments.Additional play spaces and teen lounges are also available.
For more information, or for a copy of our daily programing, please call our recreational team at ext. 4900.
Learn more about recreational experiences
Bedside Buddy
Our Bedside Buddy program is a unique group of volunteers who are dedicated to ensuring all patients have fun, even when stuck in the hospital! Although we have many excited recreation events and activities throughout the hospital, sometimes kids just need to get better in their rooms. Bedside buddies are equipped with carts loaded with board games bringing play in the comfort of the child’s room.
Education Program
The Nicklaus Children's Hospital School Program strives to provide guidance and advocacy to all patient and families through collaboration with community partners including school districts, tutoring programs, and curriculum providers to achieve academic successes throughout the course of a patient's treatment with a goal of successfully supporting the patient's re-entry back to school.
Michael Fux Family Center
The Michael Fux Family Center (MFFC) is exclusively dedicated for the entertainment of all of our patients, families and visitors. It is our way of making you feel more at home! The center offers a wide range of services and conveniences.
Learn more about MFFC
Music Therapy
Our Mission
The Music Therapy department, consisting of Board Certified Music Therapists, strives to effectuate positive therapeutic changes in patients and families through the clinical and evidence-based implementation of music to achieve individualized goals.
Music Therapy Values
Music therapists strive to improve clinical outcomes by assessing and addressing an individual's specific need areas.
A Music Therapist may help your child by:
- Providing support during non-sedate medical procedures by using music as distraction.
- Providing pain management through music and relaxation techniques.
- Engaging the patient in therapeutic and expressive activities that include both verbal and non-verbal forms of emotional expression.
- Encouraging the patient's compliance with the medical plan of care by using music as positive reinforcement.
- Facilitating general body movement using the patient's preferred music.
- Allowing the patient opportunities to practice speech and communication skills through singing and active music making.
- Promoting opportunities for family bonding and interaction in the hospital environment.
- Creating a normalized environment by using familiar music in the session and then incorporating music as part of the patient's routine while in the hospital.
Therapeutic Interventions used by our Music Therapists may include:
- Active Music Making: May include both singing and instrument play using the patient's preferred music or music familiar to the patient in order to address attention skills, language/speech skills, sensorimotor skills, and/or emotional skills.
- Drumming: Can be experienced either one-on-one or in a group setting to promote social interaction. By learning simple hand drumming techniques, patients are given a tool for coping with their hospital experience.
- Lyric Analysis: Allows a patient to explore the meaning, structure and lyrics of a song to allow opportunities to practice emotion identification, executive functioning skills, and encourage self-expression.
- Music and Art: By combining these two fine arts, patients engage in a creative process to provide opportunities for emotional identification and self-expression, to facilitate reminiscing, and practice sustained attention skills.
- Music with Guided Imagery: Promotes relaxation and positive coping skills. This intervention can be used to decrease anxiety and stress for the patient.
- Music and Multimodal Stimulation (MMS): A combination of singing, a touch progression and rocking to promote opportunities for premature infants to not only bond with their parents but also increase their tolerance to the sensory environment around them.
- Music and Relaxation: Can be used to promote sleep or comfort through live music listening.
- Pacifier Activated Lullaby (PAL): This device is used to develop and increase the coordination of a premature infant's non-nutritive suck in order to prepare them for a successful transfer to bottle/breast feeding.
- Songwriting: Provides opportunities for creative self-expression, emotion identification, as well as reflection. This intervention also provides opportunities to explore decision making skills, can help increase self-esteem, and often is used to express the patient's medical journey and life experiences.
- Therapeutic Instrument Lesson: Unlike in regular music lessons, the ultimate goal is not mastering a new skill but rather providing the patient with a meaningful distraction, a positive coping technique, and an outlet for expression all while increasing their self-confidence.
Retail Pharmacy
For the convenience of our patient families, when you are preparing for discharge from Nicklaus Children's Hospital, the Publix Pharmacy can fill and deliver all of the needed prescriptions right to your child’s room. That way, when it’s time to leave the hospital, you’ll have all the medications your child needs to continue care, and you can get back home as quickly and easily as possible.
After Discharge
Once you’re discharged home, a Publix pharmacist will call you 72 hours after discharge to see how your child is feeling, and to answer any questions you may have about the prescribed medication regimen. When it’s time for your child’s next refill, simply visit any of our Publix pharmacies. Their records are in our system, making the transition simple.
Finding the Pharmacy
The Publix Pharmacy at Nicklaus Children's is conveniently located on the first floor of the hospital, near the visitor's parking garage.
Hours of operation are:
Monday through Friday – 7:30 a.m. to 7:30 p.m.
Saturday – 9 a.m. to 5 p.m.
Sunday – 10 a.m. to 2 p.m.
Staff
The retail pharmacy is staffed by knowledgeable pediatric pharmacists who can answer dosage and drug-specific information/questions, both in English and in Spanish.
To speak with someone in the Publix Pharmacy at Nicklaus Children’s, call 305-669-7155. You can also fax your prescription to us at 305-669-6564.
Services include:
Retail Pharmacy
For the convenience of our patient families, when you are preparing for discharge from Nicklaus Children's Hospital, the Publix Pharmacy can fill and deliver all of the needed prescriptions right to your child’s room. That way, when it’s time to leave the hospital, you’ll have all the medications your child needs to continue care, and you can get back home as quickly and easily as possible.
After Discharge
Once you’re discharged home, a Publix pharmacist will call you 72 hours after discharge to see how your child is feeling, and to answer any questions you may have about the prescribed medication regimen. When it’s time for your child’s next refill, simply visit any of our Publix pharmacies. Their records are in our system, making the transition simple.
Finding the Pharmacy
The Publix Pharmacy at Nicklaus Children's is conveniently located on the first floor of the hospital, near the visitor's parking garage.
Hours of operation are:
Monday through Friday – 7:30 a.m. to 7:30 p.m.
Saturday – 9 a.m. to 5 p.m.
Sunday – 10 a.m. to 2 p.m.
Staff
The retail pharmacy is staffed by knowledgeable pediatric pharmacists who can answer dosage and drug-specific information/questions, both in English and in Spanish.
To speak with someone in the Publix Pharmacy at Nicklaus Children’s, call 305-669-7155. You can also fax your prescription to us at 305-669-6564.
Services include:
Gift Shop
Gift Shop
|
Hours of Operation
|
Monday — Friday:
|
10 a.m. - 4 p.m.
|
The Nicklaus Children's Hospital Gift Shop provides family and friends with a wide variety of products and services to brighten the spirits of children during their hospital stay. The shop is located in the Variety building, next to the Golden Cub Café.
The Gift Shop offers the convenience to customize, purchase and have gifts delivered to patients through a simple phone call. This way, those who can't come to the hospital for any reason, can still send a gift and their wishes.
NEW! Mobile Ordering Available!
Mobile ordering is now available for our Gift Shop! Family and friends visiting patients can order items for delivery to a child's room.
The GET app allows customized purchases to be made from the comfort of a mobile device with time and date selection. To view gift items available for delivery, download the GET app or visit the GET website.
Shop our New Gift Baskets!

Assorted Balloons

Baby Basket
Includes plush, nail trimmer and rattle.
Items and prices from photos may vary due to availability.
$50 - $57

Happy Bag
Includes plush, activity book and candy.
Items and prices from photos may vary due to availability.
$32.99

Spa Kit
Assortment of six personal care items to help relax.
Items and prices from photos may vary due to availability.
$39.99 - $62.99

Sweet Tooth
Assortment of candies.
Candies and container may vary from photo.
$33.99

Beanie Babies
Stuffed animals available vary in size and price.
$19.99 an up

Baby Plushies
Includes Plush, blanket, nail trimmer and rattle.
Items and prices from photos may vary due to availability.
$60 - $70

Dad's Essentials
Hat, boxers, back scratcher and shaving razor.
$49.99

Nick's Basket
Basket included.
Fleece, beverage cup and badge reel.
$55.00
For more information on our pricing and gifts,
please call 305-662-8348.
Food Services and Dining Options
Nicklaus Children's Hospital offers a variety of food and nutrition options for its patients, staff and guests.
In-Room Food Service for Patients
The Nicklaus Children's Hospital Food and Nutrition Department provides meals, special formulas, and clinical nutrition services to inpatients. The meals prepared and served by the department meet the nutritional requirements of the patients based on their medical and cultural needs, while at the same time appealing to their taste.
Room service meals are offered from 7 a.m. to 7:30 p.m.Meals can be ordered utilizing the GETwell application located on the hospital television or by calling ext. 1010 from the hospital room phone.
The department offers guest trays for parents and family members for a fee during their child’s hospitalization. The department accepts debit or credit card payments only (no cash). Guest trays can be ordered between 7 a.m. to 7:30 p.m. by calling ext. 1010 from the hospital room phone.
Download the In-Room Service Menu (PDF)
In-Room Service Menu (Creole)
On-Campus Dining Options
The Food Service Department is committed to providing great food, great service and a pleasant place for patients, families, visitors and employees to enjoy a quality dining experience. The Golden Cub Café is located on the first floor of the Variety wing, offering breakfast, lunch and dinner. Options in the cafeteria include comfort foods (hot foods), a crafted salad station, a grill (including vegetarian options) and a specialty foods station.
Delivery Available:You can now order food and drinks for delivery to a child’s room from our campus Golden Cub Café! The GET app enables you to order from your mobile device. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.

Kosher Meal Offerings
Nicklaus Children's Hospital is pleased offer a selection of certified Kosher meal options such as TV dinners and other snacks in our hospital cafeteria, the Golden Club Café.
Golden Cub Café Hours
|
Monday — Sunday
|
Breakfast:
|
7:00 a.m. - 10:30 a.m. |
Lunch:
|
11:30 a.m. - 3:30 p.m. |
Dinner:
|
4:30 p.m. - 9:00 p.m. |
New Healing Hearts Kosher Lounge
Nicklaus Children’s is pleased to unveil a new kosher food lounge that will provide a dedicated space for Jewish patients and families to maintain their kosher food practices during a hospital stay. The new space on the first floor of the hospital’s Advanced Pediatric Care Pavilion (APCP) was dedicated in a special ribbon-cutting ceremony, thanks to a generous gift from the nonprofit organization, Healing Hearts.
The Healing Hearts Kosher Lounge will be accessible 24 hours a day, seven days a week, featuring a food prep station, storage space and areas for families to relax and pray. Through the sponsorship, Healing Hearts will be providing food on a weekly basis to keep the storage space stocked with kosher food options. Families will be able to enjoy kosher wraps, sandwiches and other lunch alternatives. During the weekend, or Shabbat, full meals will be provided for families to enjoy.
Miracles Café
Starbucks We Proudly Serve®
Located in the Advanced Pediatric Care Pavilion lobby.
This café features Starbucks We Proudly Serve® coffee program offering Starbucks seasonal hot and cold drinks, Sabores Nuestro Starbucks Cuban style coffee, assorted bottled beverages, pastries, snacks, and sandwiches.
Pick-up Available: The Miracles Café is offering pick-up when you order through the GET app. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.
Miracles Café
|
Hours
|
Monday — Sunday:
|
7 a.m. - 11 p.m. |
Last order will be taken at
|
10:45 p.m. |
Subway
Located on the first floor, next to the Golden Cub Café.
Offering soups, salads and sandwiches made to order. You can also order for pickup with the Subway App.
Half Moon Empanadas
Half Moon Empanadas is located on the first floor at the Central Building lobby entrance.
Offering an assortment of empanadas, some gluten-free items, Coca Cola beverages, Cuban style coffee and iced coffee.
Half Moon Empanadas
|
Hours
|
Monday — Friday:
|
6 a.m. - 10 p.m. |
Saturday — Sunday:
|
7 a.m. - 10 p.m. |
Vending Machines
There are a few areas with vending machines around the hospital. To the west of the Golden Cub Café are coffee, soda, ice cream, and snack vending machines, as well as a microwave available for visitor use. On the second floor of the hospital is another room with vending machines as well as within patient care unit's family waiting area of the APCP Tower. Vending machines can also be found in the Emergency Department waiting area.
Catering Services
Nicklaus Children's Hospital Food Service Department provides catering options for on campus meetings, conferences, guest lectures, social and special events such as holiday and retirement parties. We are dedicated to providing top quality innovative menus for our customers.
Food Services and Dining Options
Nicklaus Children's Hospital offers a variety of food and nutrition options for its patients, staff and guests.
In-Room Food Service for Patients
The Nicklaus Children's Hospital Food and Nutrition Department provides meals, special formulas, and clinical nutrition services to inpatients. The meals prepared and served by the department meet the nutritional requirements of the patients based on their medical and cultural needs, while at the same time appealing to their taste.
Room service meals are offered from 7 a.m. to 7:30 p.m.Meals can be ordered utilizing the GETwell application located on the hospital television or by calling ext. 1010 from the hospital room phone.
The department offers guest trays for parents and family members for a fee during their child’s hospitalization. The department accepts debit or credit card payments only (no cash). Guest trays can be ordered between 7 a.m. to 7:30 p.m. by calling ext. 1010 from the hospital room phone.
Download the In-Room Service Menu (PDF)
In-Room Service Menu (Creole)
On-Campus Dining Options
The Food Service Department is committed to providing great food, great service and a pleasant place for patients, families, visitors and employees to enjoy a quality dining experience. The Golden Cub Café is located on the first floor of the Variety wing, offering breakfast, lunch and dinner. Options in the cafeteria include comfort foods (hot foods), a crafted salad station, a grill (including vegetarian options) and a specialty foods station.
Delivery Available:You can now order food and drinks for delivery to a child’s room from our campus Golden Cub Café! The GET app enables you to order from your mobile device. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.

Kosher Meal Offerings
Nicklaus Children's Hospital is pleased offer a selection of certified Kosher meal options such as TV dinners and other snacks in our hospital cafeteria, the Golden Club Café.
Golden Cub Café Hours
|
Monday — Sunday
|
Breakfast:
|
7:00 a.m. - 10:30 a.m. |
Lunch:
|
11:30 a.m. - 3:30 p.m. |
Dinner:
|
4:30 p.m. - 9:00 p.m. |
New Healing Hearts Kosher Lounge
Nicklaus Children’s is pleased to unveil a new kosher food lounge that will provide a dedicated space for Jewish patients and families to maintain their kosher food practices during a hospital stay. The new space on the first floor of the hospital’s Advanced Pediatric Care Pavilion (APCP) was dedicated in a special ribbon-cutting ceremony, thanks to a generous gift from the nonprofit organization, Healing Hearts.
The Healing Hearts Kosher Lounge will be accessible 24 hours a day, seven days a week, featuring a food prep station, storage space and areas for families to relax and pray. Through the sponsorship, Healing Hearts will be providing food on a weekly basis to keep the storage space stocked with kosher food options. Families will be able to enjoy kosher wraps, sandwiches and other lunch alternatives. During the weekend, or Shabbat, full meals will be provided for families to enjoy.
Miracles Café
Starbucks We Proudly Serve®
Located in the Advanced Pediatric Care Pavilion lobby.
This café features Starbucks We Proudly Serve® coffee program offering Starbucks seasonal hot and cold drinks, Sabores Nuestro Starbucks Cuban style coffee, assorted bottled beverages, pastries, snacks, and sandwiches.
Pick-up Available: The Miracles Café is offering pick-up when you order through the GET app. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.
Miracles Café
|
Hours
|
Monday — Sunday:
|
7 a.m. - 11 p.m. |
Last order will be taken at
|
10:45 p.m. |
Subway
Located on the first floor, next to the Golden Cub Café.
Offering soups, salads and sandwiches made to order. You can also order for pickup with the Subway App.
Half Moon Empanadas
Half Moon Empanadas is located on the first floor at the Central Building lobby entrance.
Offering an assortment of empanadas, some gluten-free items, Coca Cola beverages, Cuban style coffee and iced coffee.
Half Moon Empanadas
|
Hours
|
Monday — Friday:
|
6 a.m. - 10 p.m. |
Saturday — Sunday:
|
7 a.m. - 10 p.m. |
Vending Machines
There are a few areas with vending machines around the hospital. To the west of the Golden Cub Café are coffee, soda, ice cream, and snack vending machines, as well as a microwave available for visitor use. On the second floor of the hospital is another room with vending machines as well as within patient care unit's family waiting area of the APCP Tower. Vending machines can also be found in the Emergency Department waiting area.
Catering Services
Nicklaus Children's Hospital Food Service Department provides catering options for on campus meetings, conferences, guest lectures, social and special events such as holiday and retirement parties. We are dedicated to providing top quality innovative menus for our customers.
Food Services and Dining Options
Nicklaus Children's Hospital offers a variety of food and nutrition options for its patients, staff and guests.
In-Room Food Service for Patients
The Nicklaus Children's Hospital Food and Nutrition Department provides meals, special formulas, and clinical nutrition services to inpatients. The meals prepared and served by the department meet the nutritional requirements of the patients based on their medical and cultural needs, while at the same time appealing to their taste.
Room service meals are offered from 7 a.m. to 7:30 p.m.Meals can be ordered utilizing the GETwell application located on the hospital television or by calling ext. 1010 from the hospital room phone.
The department offers guest trays for parents and family members for a fee during their child’s hospitalization. The department accepts debit or credit card payments only (no cash). Guest trays can be ordered between 7 a.m. to 7:30 p.m. by calling ext. 1010 from the hospital room phone.
Download the In-Room Service Menu (PDF)
In-Room Service Menu (Creole)
On-Campus Dining Options
The Food Service Department is committed to providing great food, great service and a pleasant place for patients, families, visitors and employees to enjoy a quality dining experience. The Golden Cub Café is located on the first floor of the Variety wing, offering breakfast, lunch and dinner. Options in the cafeteria include comfort foods (hot foods), a crafted salad station, a grill (including vegetarian options) and a specialty foods station.
Delivery Available:You can now order food and drinks for delivery to a child’s room from our campus Golden Cub Café! The GET app enables you to order from your mobile device. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.

Kosher Meal Offerings
Nicklaus Children's Hospital is pleased offer a selection of certified Kosher meal options such as TV dinners and other snacks in our hospital cafeteria, the Golden Club Café.
Golden Cub Café Hours
|
Monday — Sunday
|
Breakfast:
|
7:00 a.m. - 10:30 a.m. |
Lunch:
|
11:30 a.m. - 3:30 p.m. |
Dinner:
|
4:30 p.m. - 9:00 p.m. |
New Healing Hearts Kosher Lounge
Nicklaus Children’s is pleased to unveil a new kosher food lounge that will provide a dedicated space for Jewish patients and families to maintain their kosher food practices during a hospital stay. The new space on the first floor of the hospital’s Advanced Pediatric Care Pavilion (APCP) was dedicated in a special ribbon-cutting ceremony, thanks to a generous gift from the nonprofit organization, Healing Hearts.
The Healing Hearts Kosher Lounge will be accessible 24 hours a day, seven days a week, featuring a food prep station, storage space and areas for families to relax and pray. Through the sponsorship, Healing Hearts will be providing food on a weekly basis to keep the storage space stocked with kosher food options. Families will be able to enjoy kosher wraps, sandwiches and other lunch alternatives. During the weekend, or Shabbat, full meals will be provided for families to enjoy.
Miracles Café
Starbucks We Proudly Serve®
Located in the Advanced Pediatric Care Pavilion lobby.
This café features Starbucks We Proudly Serve® coffee program offering Starbucks seasonal hot and cold drinks, Sabores Nuestro Starbucks Cuban style coffee, assorted bottled beverages, pastries, snacks, and sandwiches.
Pick-up Available: The Miracles Café is offering pick-up when you order through the GET app. To view the menu, download the GET app or visit the GET website.
Please note: Food items are for non-patients only and should not be given to patients without clearance from clinical staff, due to possible dietary restrictions.
Miracles Café
|
Hours
|
Monday — Sunday:
|
7 a.m. - 11 p.m. |
Last order will be taken at
|
10:45 p.m. |
Subway
Located on the first floor, next to the Golden Cub Café.
Offering soups, salads and sandwiches made to order. You can also order for pickup with the Subway App.
Half Moon Empanadas
Half Moon Empanadas is located on the first floor at the Central Building lobby entrance.
Offering an assortment of empanadas, some gluten-free items, Coca Cola beverages, Cuban style coffee and iced coffee.
Half Moon Empanadas
|
Hours
|
Monday — Friday:
|
6 a.m. - 10 p.m. |
Saturday — Sunday:
|
7 a.m. - 10 p.m. |
Vending Machines
There are a few areas with vending machines around the hospital. To the west of the Golden Cub Café are coffee, soda, ice cream, and snack vending machines, as well as a microwave available for visitor use. On the second floor of the hospital is another room with vending machines as well as within patient care unit's family waiting area of the APCP Tower. Vending machines can also be found in the Emergency Department waiting area.
Catering Services
Nicklaus Children's Hospital Food Service Department provides catering options for on campus meetings, conferences, guest lectures, social and special events such as holiday and retirement parties. We are dedicated to providing top quality innovative menus for our customers.
Michael Fux Family Center
Located next to the main lobby, the Michael Fux Family Center (MFFC) is exclusively dedicated for the entertainment of all of our patients, families and visitors. It is our way of making you feel more at home! The center offers a wide range of services and conveniences.
Michael Fux Family Center Amenities
- Library
- Activity/Game Room
- Kitchen
- Dining Room and Lounge
- Laundry
- Cardio Gym
- FuXplore Room
|
- Reading Room
- Business Center
- Internet Cafe
- Hair Styling and Massage Room
- Showers and Lockers
- Quiet Room
- Movie Theater and performance center
|
We are grateful to Mr. Michael Fux for sharing our vision of creating a special place where families can enjoy activities, find relaxation, refresh themselves and perhaps even forget for a little while that they are in a hospital. The center is a tribute to Mr. Fux and to the thousands of families who entrust their children to our care each year. It’s a part of our commitment to support and empower those we serve.
Visiting the Michael Fux Family Center
- We ask all inpatients to obtain a medical clearance card from their nurse prior to visiting the center.
- All inpatients under the age of 13 and/ or outpatient visitors under the age of 16 need to be accompanied by an adult at all times.

Hours of Operation
Monday – Friday: 8:30 a.m. to 6:00 p.m.
Saturday – Sunday: 1:00 p.m. to 6:00 p.m.
Michael Fux Family Center
Located next to the main lobby, the Michael Fux Family Center (MFFC) is exclusively dedicated for the entertainment of all of our patients, families and visitors. It is our way of making you feel more at home! The center offers a wide range of services and conveniences.
Michael Fux Family Center Amenities
- Library
- Activity/Game Room
- Kitchen
- Dining Room and Lounge
- Laundry
- Cardio Gym
- FuXplore Room
|
- Reading Room
- Business Center
- Internet Cafe
- Hair Styling and Massage Room
- Showers and Lockers
- Quiet Room
- Movie Theater and performance center
|
We are grateful to Mr. Michael Fux for sharing our vision of creating a special place where families can enjoy activities, find relaxation, refresh themselves and perhaps even forget for a little while that they are in a hospital. The center is a tribute to Mr. Fux and to the thousands of families who entrust their children to our care each year. It’s a part of our commitment to support and empower those we serve.
Visiting the Michael Fux Family Center
- We ask all inpatients to obtain a medical clearance card from their nurse prior to visiting the center.
- All inpatients under the age of 13 and/ or outpatient visitors under the age of 16 need to be accompanied by an adult at all times.

Hours of Operation
Monday – Friday: 8:30 a.m. to 6:00 p.m.
Saturday – Sunday: 1:00 p.m. to 6:00 p.m.
Accepted Health Plans and Insurance Providers
As the only pediatric hospital in South Florida dedicated exclusively to children, Nicklaus Children's Hospital, and its multispecialty physician group, Nicklaus Children’s Pediatric Specialists, LLC, is proud to be an in-network provider for the majority of health insurance plans providing coverage to our patients. In support of our mission to inspire hope and promote lifelong health by providing the best care to every child, our Managed Care team works closely with our health insurance partners to ensure a wide array of coverage and access options for patients.
Listed below are the health insurance plans participating with Nicklaus. In addition, we also accept a variety of Behavioral Health, Dental and Vision plans. If you have any questions, please email payer.credentialing@nicklaushealth.org. In addition, we always recommend contacting your health insurance plan directly to verify Nicklaus’ participation status based on the specifics of your insurance benefit plan design.
We are grateful for the opportunity to care for your children.
| COMMERCIAL INSURANCE PLANS(HMO/PPO/POS/EPO) |
- Aetna
- AvMed Health Plans*
- Blue Cross Blue Shield of Florida
- Cigna HealthCare
*Excluding Jackson Select Product |
- Humana
- Imagine Health
- Multiplan
- UnitedHealthcare
|
| MEDICAID HMO & HEALTHY KIDS PLANS |
|
Medicaid HMO:
- Aetna Better Health
- AmeriHealth Caritas of Florida*
- Community Care Plan
- Humana
- Molina Healthcare of Florida
- Simply
- Sunshine Health
- CMS Title 19 & 21
- Child Welfare
- SMI
- UnitedHealthcare
- US Virgin Islands Government
|
Healthy Kids:
- Aetna Better Health
- Community Care Plan
- Simply/Clear Health Alliance
|
|
*No longer offering a Florida Medicaid plan effective 2/1/2025
|
| HEALTHCARE INSURANCE EXCHANGE PLANS |
- Aetna QHP
- AmBetter Sunshine
- AmeriHealth Caritas of Florida
|
|
| INTERNATIONAL PLANS |
- Best Doctors
- Global Health Claim Services
- Epic Health Solutions
|
- Quality Health Management
- Salubris
- Worldwide Concierge Healthcare Services
|
Authorization requirements vary by each plan/group. Please contact your health plan directly to verify if your insurance plan is participating with Nicklaus Children's and to verify authorization requirements as some insurance plans utilize narrow networks which may exclude our facility.
Please note that some non-employed physicians and credentialed medical staff members of Nicklaus Children's Hospital may not accept all of the health plans listed above. Also note that participation in these plans is not a guarantee of payment or coverage.
Accepted Health Plans and Insurance Providers
As the only pediatric hospital in South Florida dedicated exclusively to children, Nicklaus Children's Hospital, and its multispecialty physician group, Nicklaus Children’s Pediatric Specialists, LLC, is proud to be an in-network provider for the majority of health insurance plans providing coverage to our patients. In support of our mission to inspire hope and promote lifelong health by providing the best care to every child, our Managed Care team works closely with our health insurance partners to ensure a wide array of coverage and access options for patients.
Listed below are the health insurance plans participating with Nicklaus. In addition, we also accept a variety of Behavioral Health, Dental and Vision plans. If you have any questions, please email payer.credentialing@nicklaushealth.org. In addition, we always recommend contacting your health insurance plan directly to verify Nicklaus’ participation status based on the specifics of your insurance benefit plan design.
We are grateful for the opportunity to care for your children.
| COMMERCIAL INSURANCE PLANS(HMO/PPO/POS/EPO) |
- Aetna
- AvMed Health Plans*
- Blue Cross Blue Shield of Florida
- Cigna HealthCare
*Excluding Jackson Select Product |
- Humana
- Imagine Health
- Multiplan
- UnitedHealthcare
|
| MEDICAID HMO & HEALTHY KIDS PLANS |
|
Medicaid HMO:
- Aetna Better Health
- AmeriHealth Caritas of Florida*
- Community Care Plan
- Humana
- Molina Healthcare of Florida
- Simply
- Sunshine Health
- CMS Title 19 & 21
- Child Welfare
- SMI
- UnitedHealthcare
- US Virgin Islands Government
|
Healthy Kids:
- Aetna Better Health
- Community Care Plan
- Simply/Clear Health Alliance
|
|
*No longer offering a Florida Medicaid plan effective 2/1/2025
|
| HEALTHCARE INSURANCE EXCHANGE PLANS |
- Aetna QHP
- AmBetter Sunshine
- AmeriHealth Caritas of Florida
|
|
| INTERNATIONAL PLANS |
- Best Doctors
- Global Health Claim Services
- Epic Health Solutions
|
- Quality Health Management
- Salubris
- Worldwide Concierge Healthcare Services
|
Authorization requirements vary by each plan/group. Please contact your health plan directly to verify if your insurance plan is participating with Nicklaus Children's and to verify authorization requirements as some insurance plans utilize narrow networks which may exclude our facility.
Please note that some non-employed physicians and credentialed medical staff members of Nicklaus Children's Hospital may not accept all of the health plans listed above. Also note that participation in these plans is not a guarantee of payment or coverage.
Accepted Health Plans and Insurance Providers
As the only pediatric hospital in South Florida dedicated exclusively to children, Nicklaus Children's Hospital, and its multispecialty physician group, Nicklaus Children’s Pediatric Specialists, LLC, is proud to be an in-network provider for the majority of health insurance plans providing coverage to our patients. In support of our mission to inspire hope and promote lifelong health by providing the best care to every child, our Managed Care team works closely with our health insurance partners to ensure a wide array of coverage and access options for patients.
Listed below are the health insurance plans participating with Nicklaus. In addition, we also accept a variety of Behavioral Health, Dental and Vision plans. If you have any questions, please email payer.credentialing@nicklaushealth.org. In addition, we always recommend contacting your health insurance plan directly to verify Nicklaus’ participation status based on the specifics of your insurance benefit plan design.
We are grateful for the opportunity to care for your children.
| COMMERCIAL INSURANCE PLANS(HMO/PPO/POS/EPO) |
- Aetna
- AvMed Health Plans*
- Blue Cross Blue Shield of Florida
- Cigna HealthCare
*Excluding Jackson Select Product |
- Humana
- Imagine Health
- Multiplan
- UnitedHealthcare
|
| MEDICAID HMO & HEALTHY KIDS PLANS |
|
Medicaid HMO:
- Aetna Better Health
- AmeriHealth Caritas of Florida*
- Community Care Plan
- Humana
- Molina Healthcare of Florida
- Simply
- Sunshine Health
- CMS Title 19 & 21
- Child Welfare
- SMI
- UnitedHealthcare
- US Virgin Islands Government
|
Healthy Kids:
- Aetna Better Health
- Community Care Plan
- Simply/Clear Health Alliance
|
|
*No longer offering a Florida Medicaid plan effective 2/1/2025
|
| HEALTHCARE INSURANCE EXCHANGE PLANS |
- Aetna QHP
- AmBetter Sunshine
- AmeriHealth Caritas of Florida
|
|
| INTERNATIONAL PLANS |
- Best Doctors
- Global Health Claim Services
- Epic Health Solutions
|
- Quality Health Management
- Salubris
- Worldwide Concierge Healthcare Services
|
Authorization requirements vary by each plan/group. Please contact your health plan directly to verify if your insurance plan is participating with Nicklaus Children's and to verify authorization requirements as some insurance plans utilize narrow networks which may exclude our facility.
Please note that some non-employed physicians and credentialed medical staff members of Nicklaus Children's Hospital may not accept all of the health plans listed above. Also note that participation in these plans is not a guarantee of payment or coverage.
Nearby Restaurants and Shopping
Looking for the nearest supermarket, shopping mall, restaurant, church, or other places of worship? Use the map below to locate all the places of interest near to our main hospital campus. Click on the icon for the location of interest, or expand the menu on the top left to see the list of all the locations.
Nearby Restaurants and Shopping
Looking for the nearest supermarket, shopping mall, restaurant, church, or other places of worship? Use the map below to locate all the places of interest near to our main hospital campus. Click on the icon for the location of interest, or expand the menu on the top left to see the list of all the locations.
Locations & Directions to Hospital and Outpatient Centers
Patients and Parents Rights and Responsibilities
Nicklaus Children’s Hospital and its facilities have a responsibility to provide your child with appropriate medical care. The following is a set of guiding principles of patient care. It is important for you to know what your child’s rights are as a patient and what your rights and obligations are as a parent and user of this hospital.
We encourage you to talk with those involved with your child’s care. A summary of your rights and responsibilities follows.
You and your child have the right:
- To be treated with courtesy and respect, with appreciation of his or her individual dignity and with protection of his or her need for privacy.
- To a prompt and reasonable response to questions and requests.
- To know who is providing medical services and who is responsible for his or her care.
- To participate in the development and implementation of the patient plan of care.
- To know what patient support services are available, including whether an interpreter is available if he or she does not speak English.
- To know what rules and regulations apply to his or her conduct.
- To be given information concerning diagnosis, planned course of treatment, alternatives, risks and prognosis by the healthcare provider.
- To refuse any treatment, except as otherwise provided by law.
- To be given, upon request, full information and necessary counseling on the availability of known financial resources for his or her care.
- To know, upon request and in advance of treatment, whether the healthcare provider or healthcare facility accepts the Medicare assignment rate.
- To receive, upon request, prior to treatment, a reasonable estimate of charges for medical care.
- To receive a copy of a reasonably clear and understandable itemized bill and, upon request, to have the charges explained.
- To impartial access to medical treatment or accommodations, regardless of race, national origin, religion, handicap or source of payment.
- To treatment for any emergency medical condition that will deteriorate from failure to provide treatment.
- To know if medical treatment is for purposes of experimental research and to give his or her consent or refusal to participate in such experimental research.
- To express grievances regarding any violation of his or her rights, as stated
- in Florida law, through the grievance procedure of the healthcare provider or healthcare facility which served him or her and to the appropriate state licensing agency.
- Nicklaus Children’s Hospital complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability or sex.
A patient (or family/guardian) is responsible for:
- Providing to the healthcare provider, to the best of his or her knowledge, accurate and complete information about present complaints, past illnesses, hospitalizations, medications, and other matters relating to his or her health.
- Reporting unexpected changes in his or her condition to the healthcare provider.
- Reporting to the healthcare provider whether he or she comprehends a contemplated course of action and what is expected of him or her.
- Following the treatment plan recommended by the healthcare provider.
- Keeping appointments and, when he or she is unable to do so for any reason, notifying the healthcare provider or healthcare facility.
- His or her actions if he or she refuses treatment or does not follow the healthcare provider’s instructions.
- Assuring that the financial obligations of his or her healthcare are fulfilled as promptly as possible.
- Following healthcare facility rules and regulations affecting patient care and conduct.
Visitation guidelines:
Each patient/parent(s), legal guardian and/or legal guardian designee (or support person, where appropriate) will be informed of the right, subject to his or her consent, to receive the visitors whom he or she designates, including, but not limited to a spouse, domestic partner (including same sex domestic partners), other family members or a friend, and his or her right to withdraw consent at any time;
- Not restrict, limit, or otherwise deny visitation privileges on the basis of race, color, national origin, religion, sex, gender identity, sexual orientation or disability; and
- Ensure that all visitors enjoy full visitation privileges consistent with the patient preferences.
- All visitors should be free from symptoms of contagious disease and known exposures.
Feedback is important
The Patient and Guest Relations Department is responsible for pursuing and/or referring any questions, concerns,complaints, or grievances you may have about your rights or the quality of care and services provided by Nicklaus Children’s Hospital and its network of outpatient facilities. You may contact the Patient and Guest Relations staff directly at extension 4400, or ask any staff member to contact them on your behalf. If this is an emergency, please call the hospital operator (dial 0) and ask for them to page the Operations Administrator. We will gladly address any issues or concerns that you may have regarding your child’s care.
Should you have any questions or complaints regarding the quality of care offered by a healthcare provider or healthcare facility, you may contact the Agency for Healthcare Administration at 1-888-419-3456 or write:
AGENCY FOR HEALTH CARE ADMINISTRATION
Consumer Assistance
Unit 2727
Mahan Drive Tallahassee, FL 32308-5403
Or
DNV GL Healthcare http://dnvglhealthcare.com/patient-complaint-report
Toll Free: 1-866-496-9647
Fax: (513) 947-1250
We value your feedback and concerns.
Patients and Parents Rights and Responsibilities
Nicklaus Children’s Hospital and its facilities have a responsibility to provide your child with appropriate medical care. The following is a set of guiding principles of patient care. It is important for you to know what your child’s rights are as a patient and what your rights and obligations are as a parent and user of this hospital.
We encourage you to talk with those involved with your child’s care. A summary of your rights and responsibilities follows.
You and your child have the right:
- To be treated with courtesy and respect, with appreciation of his or her individual dignity and with protection of his or her need for privacy.
- To a prompt and reasonable response to questions and requests.
- To know who is providing medical services and who is responsible for his or her care.
- To participate in the development and implementation of the patient plan of care.
- To know what patient support services are available, including whether an interpreter is available if he or she does not speak English.
- To know what rules and regulations apply to his or her conduct.
- To be given information concerning diagnosis, planned course of treatment, alternatives, risks and prognosis by the healthcare provider.
- To refuse any treatment, except as otherwise provided by law.
- To be given, upon request, full information and necessary counseling on the availability of known financial resources for his or her care.
- To know, upon request and in advance of treatment, whether the healthcare provider or healthcare facility accepts the Medicare assignment rate.
- To receive, upon request, prior to treatment, a reasonable estimate of charges for medical care.
- To receive a copy of a reasonably clear and understandable itemized bill and, upon request, to have the charges explained.
- To impartial access to medical treatment or accommodations, regardless of race, national origin, religion, handicap or source of payment.
- To treatment for any emergency medical condition that will deteriorate from failure to provide treatment.
- To know if medical treatment is for purposes of experimental research and to give his or her consent or refusal to participate in such experimental research.
- To express grievances regarding any violation of his or her rights, as stated
- in Florida law, through the grievance procedure of the healthcare provider or healthcare facility which served him or her and to the appropriate state licensing agency.
- Nicklaus Children’s Hospital complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability or sex.
A patient (or family/guardian) is responsible for:
- Providing to the healthcare provider, to the best of his or her knowledge, accurate and complete information about present complaints, past illnesses, hospitalizations, medications, and other matters relating to his or her health.
- Reporting unexpected changes in his or her condition to the healthcare provider.
- Reporting to the healthcare provider whether he or she comprehends a contemplated course of action and what is expected of him or her.
- Following the treatment plan recommended by the healthcare provider.
- Keeping appointments and, when he or she is unable to do so for any reason, notifying the healthcare provider or healthcare facility.
- His or her actions if he or she refuses treatment or does not follow the healthcare provider’s instructions.
- Assuring that the financial obligations of his or her healthcare are fulfilled as promptly as possible.
- Following healthcare facility rules and regulations affecting patient care and conduct.
Visitation guidelines:
Each patient/parent(s), legal guardian and/or legal guardian designee (or support person, where appropriate) will be informed of the right, subject to his or her consent, to receive the visitors whom he or she designates, including, but not limited to a spouse, domestic partner (including same sex domestic partners), other family members or a friend, and his or her right to withdraw consent at any time;
- Not restrict, limit, or otherwise deny visitation privileges on the basis of race, color, national origin, religion, sex, gender identity, sexual orientation or disability; and
- Ensure that all visitors enjoy full visitation privileges consistent with the patient preferences.
- All visitors should be free from symptoms of contagious disease and known exposures.
Feedback is important
The Patient and Guest Relations Department is responsible for pursuing and/or referring any questions, concerns,complaints, or grievances you may have about your rights or the quality of care and services provided by Nicklaus Children’s Hospital and its network of outpatient facilities. You may contact the Patient and Guest Relations staff directly at extension 4400, or ask any staff member to contact them on your behalf. If this is an emergency, please call the hospital operator (dial 0) and ask for them to page the Operations Administrator. We will gladly address any issues or concerns that you may have regarding your child’s care.
Should you have any questions or complaints regarding the quality of care offered by a healthcare provider or healthcare facility, you may contact the Agency for Healthcare Administration at 1-888-419-3456 or write:
AGENCY FOR HEALTH CARE ADMINISTRATION
Consumer Assistance
Unit 2727
Mahan Drive Tallahassee, FL 32308-5403
Or
DNV GL Healthcare http://dnvglhealthcare.com/patient-complaint-report
Toll Free: 1-866-496-9647
Fax: (513) 947-1250
We value your feedback and concerns.
Request a Pediatric Appointment
At Nicklaus Children's Hospital, we take care of children from birth up to age 21. We offer a wide range of healthcare services designed specifically for kids, including urgent care, rehabilitation services, and subspecialty physician appointments. Schedule an appointment with our pediatric specialists today.
Physician Appointment Requests
Request a new patient or a general clinician visit appointment with Nicklaus Children's Hospital specialist.
Our phone line is also available to schedule your requests from Monday to Friday: 7:00 am to 7:00 pm by calling 1-888-624-2778.
Outpatient Diagnostic, Exam, or Therapy Screening Requests
Request a follow-up appointment or referral visit with one of our specialists.
You can either fill out an online form and wait for a Nicklaus Children's coordinator to schedule your visit within 24-48 business hours, or you can speak with an agent and schedule your appointment over the phone between Monday to Friday: 7:00 am to 7:00 pm.
Prescription Requests for Appointments
Request a Pediatric Appointment
At Nicklaus Children's Hospital, we take care of children from birth up to age 21. We offer a wide range of healthcare services designed specifically for kids, including urgent care, rehabilitation services, and subspecialty physician appointments. Schedule an appointment with our pediatric specialists today.
Physician Appointment Requests
Request a new patient or a general clinician visit appointment with Nicklaus Children's Hospital specialist.
Our phone line is also available to schedule your requests from Monday to Friday: 7:00 am to 7:00 pm by calling 1-888-624-2778.
Outpatient Diagnostic, Exam, or Therapy Screening Requests
Request a follow-up appointment or referral visit with one of our specialists.
You can either fill out an online form and wait for a Nicklaus Children's coordinator to schedule your visit within 24-48 business hours, or you can speak with an agent and schedule your appointment over the phone between Monday to Friday: 7:00 am to 7:00 pm.
Prescription Requests for Appointments
SAFE KIDS Miami Dade County
Nicklaus Children's Hospital Injury Prevention Programs
Nicklaus Children's Hospital is the Proud Lead Organization for the Miami-Dade County SAFE KIDS Coalition. The Miami-Dade County SAFE KIDS Coalition is comprised of public, private and voluntary organizations united and committed to identify and significantly reduce unintentional deaths and injuries to the children of South Florida. We respond to the needs of our community by providing professional education, practical training programs, and legislative initiatives essential to promote the safety and wellbeing of our children.
For more information about SAFE KIDS or for additional age specific safety tips visit:
safekids.org
SAFE KIDS Miami Dade County
Nicklaus Children's Hospital Injury Prevention Programs
Nicklaus Children's Hospital is the Proud Lead Organization for the Miami-Dade County SAFE KIDS Coalition. The Miami-Dade County SAFE KIDS Coalition is comprised of public, private and voluntary organizations united and committed to identify and significantly reduce unintentional deaths and injuries to the children of South Florida. We respond to the needs of our community by providing professional education, practical training programs, and legislative initiatives essential to promote the safety and wellbeing of our children.
For more information about SAFE KIDS or for additional age specific safety tips visit:
safekids.org
Child Life in the Community
The Child Life department at Nicklaus Children’s Hospital is involved in a variety of programs within the community.
Community Field Trips
Community Field Trips are pre-arranged tours conducted by the child life department for students in kindergarten through the sixth grade. This community service is designed to normalize and increase awareness of the hospital environment.
Helpful Tips and Information
- Arrange your own transportation
- Limit group size to 15 - 20 students
- Every child should wear a name tag
- A Child life specialist will welcome your students in the front lobby
Field Trip Goals and Objectives
- To enhance existing curricula/thematic unit
- To increase awareness of the hospital experience
- To increase understanding of medical equipment and supplies
- To increase awareness of body parts/anatomy systems
- To increase awareness of professions, job duties, and responsibilities within a hospital setting
- To promote the importance of team work
- Medical Play Session
- Specific departmental tours and orientation to role and job duties
- Opportunities for multi-sensory educational activities
Child Life Career Day
Please email the child life department to coordinate a career day.
Gift and Toy Donations
The Child Life department at Nicklaus Children’s Hospital is extremely grateful for those interested in making a donation for our patients. Please keep in mind that we are unable to accept donations of used toys (including stuffed/cloth toys) due to the hospital's infection control policy.
Donation Guidelines
- Due to strict infection control purposes, all donated items must be new and unwrapped.
- We do not accept latex balloons, candy/food items, or violent toys.
- In order to ensure patient safety and abide by patient confidentiality regulations, gifts cannot be delivered directly to patients by the donor(s).
Drop-Off Instructions
You may drop off your toy donations at any Nicklaus Children's Outpatient Center.
If you have any questions, please call 786-624-2880 or email toydrive@nicklaushealth.org.
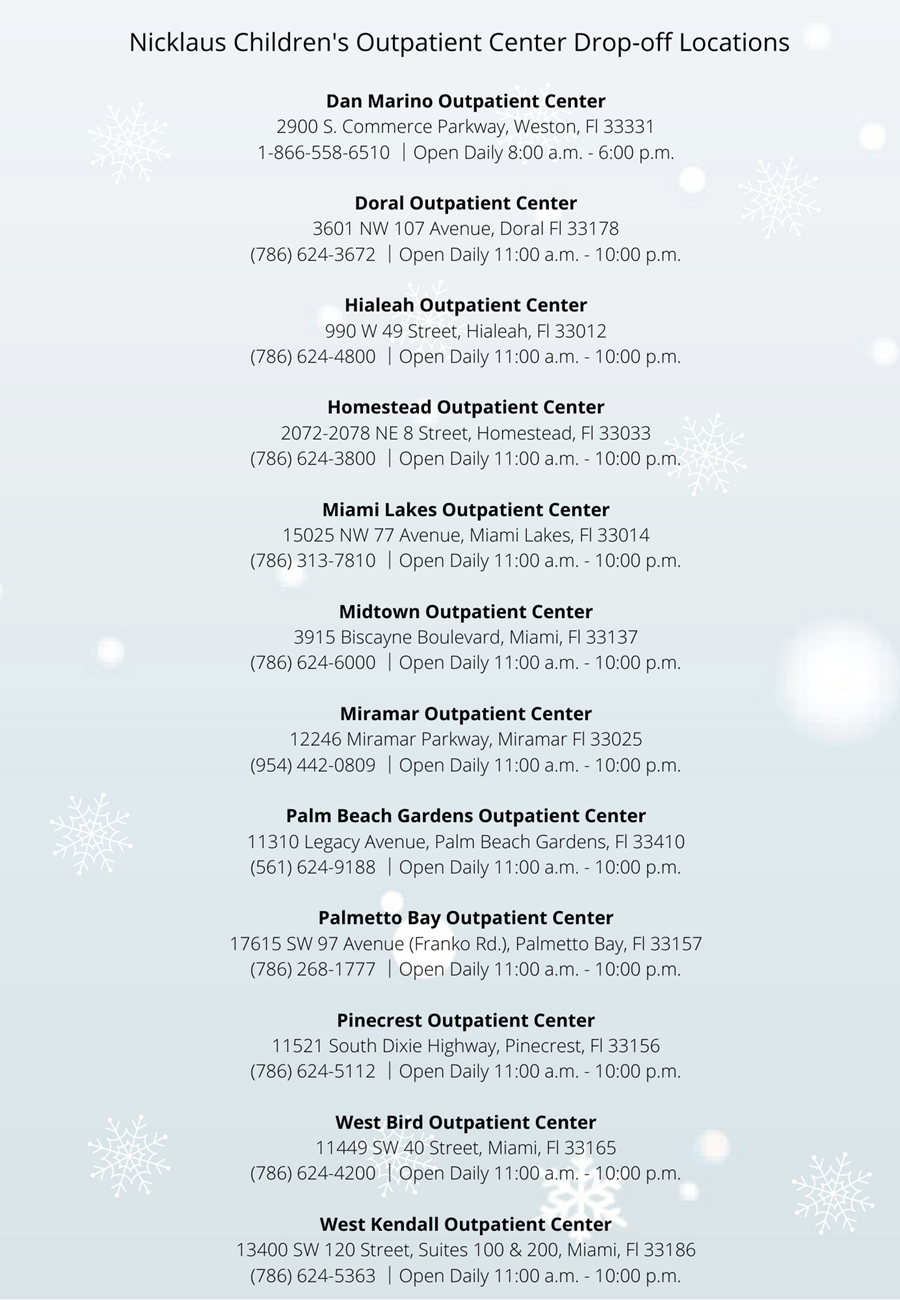
Our Top Priority Needs
- Gifts for Teens
- Light Up Toddler Toys
- Infant toys (rattles, pacifiers, etc.)
- Gross Motor Riding Toys
- Popular Card/Board Games (i.e. Uno)
- Superhero Toys/Action Figures
- I-Pods
- Gift Cards in Small Increments ($5-$15); Walmart, Target, iTunes.
- Teen Coloring Books/Sketch Pads
- Coloring books
- Bubbles
Children's Experiences' Team Wish list
Click a title to view the full list or
click to view in Amazon.
Infant/Toddler Toys
Infant/Toddler Toys
(Greatest Need)
- Musical Crib Soothers
- Nurture Smart Mobiles (by Playability)
- Bouncy Chairs/Baby Swings
- Double Feature Mirror (by Manhattan Toy)
- Leap Frog Toys
- Fisher Price Toys
- V-tech Toys
- Baby Activity Gyms
- Light up/Musical Toys
- Rattles/Teethers
Gifts for Teens
Gifts for Teens
(Greatest Need)
- Room Décor (posters, glow-in-the-dark stars, etc.)
- Journals
- Poker Sets
- Table Top Tennis/Foosball/Air Hockey
- Sports Balls
- Lego Architecture Sets
- Jigsaw Puzzles
- Headphones
- Jewelry Gift Sets
- Teen Activity Kits
- Scrap Booking Kits
- Ceramic Painting Kits
- Jewelry/Bracelet Craft Kits
- Make-Up Sets
- Colognes /Perfumes/Body Spray
- Nail Polish/Nail Art Kits
- Spa Kits
- Headbands
- Eye masks (to sleep)
- Scented chap stick
- Gel pens
General Toys
General Toys
- Pretend Play Food
- Play-Doh/Play-Doh Kits
- Lego Sets (girl & boy – all ages)
- Construction Sets (car/train)
- Musical Instruments (for kids)
- Fisher Price & Doc McStuffins Medical Kits
- Matchbox Cars
- Train Sets
- Plastic Wagons (by Radio Flyer)
- Barbie Dolls
- Fisher Price “Little People” Play Sets
- Action Figures
- Plastic Animals
- Baby Dolls
- Mickey Mouse/ Minnie Mouse Toys
- Board Games (preschool, school-age, and teen)
- Uno Cards
- Headbands Game
- Science Kits
Arts and Crafts/Distraction Items
Arts and Crafts/Distraction Items
- Bubbles (wedding size/ bubble wands)
- Grab-and-Go Activity Kits (Target dollar section)
- Stress Balls
- Light up Handheld Toys (light spinners)
- Glitter Wands
- Puzzles (for all ages)
- Coloring/Sticker/Activity Books
- Crayola Activity Packs
- Crayons/Markers/Colored Pencils
- Canvases/Acrylic Paint
- Craft Supplies (glue, scissors, markers, pencils, colored pencils, sharpeners)
- Beading Kits/Loom Bracelet Kits
- Sand Art Kits
- Sketch Pads
- Adult Coloring Books
- Sharpies (all colors)
- Lap Desks
- Dry Erase Boards
Gift Cards
Gift Cards
(in small increments to give as gifts)
- Target
- iTunes
- Claire’s
- Best Buy
- Toys R Us/Babies R Us
- Barnes and Noble
- Dave and Busters
- Visa
- Build a Bear
- Movie Theaters
- Gymboree
- Amazon
Electronics
Electronics
- iPods/iPads/iTouch
- Earphones
- Polaroid Cameras (with film)
- IPhone/Android chargers
- Wireless Bluetooth Speakers
- Wireless Headphones
- X-box & Wii game systems
Musical Instruments
Musical Instruments
- Character Themed Instrument Sets (drums, kazoos, maracas, tambourines)
- Children’s rainstick
- Chiquita shakers
- Egg shakers
- Headphones
Educational Materials
Educational Materials
- School Supplies (notebooks, pencils, sharpeners, spiral notebooks)
- Flash Cards
- Learning Games
- Pre-K Workbooks
- Reading books (pre-school & school age)
Meet the Child Life Specialist Team
Meet the Child Life Specialists
Child Life Students
Child Life Practicum Program (Pre-Internship Experience)
Child Life Practicum opportunities are available in Fall semester.
The Child Life Practicum Program at Nicklaus Children's Hospital provides students a variety of opportunities for an observation experience under the direct supervision of a Child Life Specialist in his/her designated unit. This experience follows the Association of Child Life Professionals’ pre-internship modules to enhance learning and prepare students for their clinical child life internship.
Through these observations, practicum students will see how a Child Life Specialist uses developmental theories to make assessments and provide individualized interventions to help aid in patients and families coping within the hospital setting. Interventions include but are not limited to: developmentally appropriate diagnosis and procedural teaching, distraction during medical procedures, medical play sessions, therapeutic play, special events, legacy building and bereavement support.
Child Life Practicum Length
The Child Life Practicum at Nicklaus Children’s Hospital is an 80-hour clinical experience offered during the Fall semester (2- 5 weeks). Practicum students schedule will follow the work hours of unit preceptor.
**Child Life coverage is currently provided at the hospital 7 days a week from 6:30am-11:30pm.
Child Life Practicum Application Requirements
To be considered for a Child Life Practicum, students must be at a junior college level status towards completion of a bachelor's or master's degree in the fields of Child Life, Child development, Education, Family and Human development, Recreation Therapy, and Psychology.
Due to hospital requirements, students applying of for a practicum must be affiliated with one of the following universities to be eligible for consideration: American Public University, Florida International University, or Nova Southeastern university.
Selection of practicum students is determined based on a variety of criteria that include: academics, previous experience working with children, references, and an interview. Applicants will be notified via email if they are selected to move forward in the interview process.
A completed practicum application form must include:
- Cover Letter
- Resume
- Verification of a minimum of 50 hrs. of hospital volunteer experience in a pediatric hospital/medical setting
- Verification of a minimum of 50 hrs. of experience with well children and families
- Unofficial transcript
- Two letters of recommendation
Applications can be forwarded to: childlifestudentprograms@nicklaushealth.org
Due Date is September 20, 2024
Child Life Practicum Program Application Form
Child Life Internship Program
Child Life Internship opportunities are available in Spring and Summer semesters.
The Child Life Internship Program at Nicklaus Children's Hospital is an Association of Child Life Professionals (ACLP) accredited internship program that provides students a variety of opportunities for experience and practice in providing child life interventions. With support from their preceptors, child life interns will utilize developmental theories to gain increasing independence making assessments and providing individualized interventions to help aid patients and families in coping within the hospital setting. Interventions include but are not limited to: developmentally appropriate diagnosis and procedural teaching, distraction during medical procedures, medical play sessions, therapeutic play, special events, legacy building and bereavement support.
Child Life Internship Length
Child Life intern will have the opportunity to observe and implement Child Life interventions in various clinical units where child life services are provided at Nickalus Childrens Hospital.
As part of the required 600hrs of clinical internship experience, Child Life interns will complete 2 clinical rotations that are 6 weeks in length and an additional mini rotation in patient care units open of students. Child Life interns must complete 600 hours over 15 weeks (40 hours per week – this can include days, nights, and weekends). The selected intern's schedule will follow the work hours of unit preceptor.
**Child Life coverage is currently provided at the hospital 7 days a week from 6:30am-11:30pm.
The Spring internship typically takes place from January through May while the Summer internship typically takes place from June through September.
Child Life Internship Application Requirements
To be considered for a Child Life Internship, students must be in the process of pursuing a bachelor’s degree and have senior level status or be graduate students earning a degree in a suggested child development related major. All ACLP required coursework must be completed prior to the internship start date. Due to hospital requirements, all students must be affiliated with a college/university during their internship semester.
A completed internship applications must include:
- Completed ACLP Internship Readiness Common Application Application Portal (smapply.io)
- Unofficial copy of all college/university transcripts
- Resume
- ACLP Eligibility Assessment
- Child Life Course Verification
- Two letters of recommendation
- HIGHLY RECOMMENDED - Verification of completion of Child Life Practicum
Applications can be forwarded to: childlifestudentprograms@nicklaushealth.org.
Selection of Child Life interns is determined based on a variety of criteria that include: academics, previous experience working with children in or outside of hospital setting, references, and an interview. Candidates will be notified via email if they are chosen to move forward in the interview process.
Our program follows the standard internship deadline, offer, and acceptance dates published by the ACLP.
At this time, Nicklaus Children’s Hospital is unable to provide housing or a stipend for child life interns.
Accepted interns must comply with the Nicklaus Children’s Hospital employee dress code and the dress code of the Child Life Department. Following acceptance of an internship offer, the student must provide:
- Background check
- Current immunization records
- Flu and Covid vaccination records
- CPR Certification (AHA approved only)
We appreciate your interest in Nicklaus Children's Hospital Child Life internship. If you have any questions, please contact the Child Life Student Academic Coordinator at 786-624-5482.
This hospital fully complies with the Age Discrimination in Employment Act of 1968 and the Civil Rights Act of 1964 which prohibits employment discrimination based upon race, color, creed, sex, age, national origin, physical disability or veteran status.
A Criminal Conviction record search is made of all prospective students of the hospital. A conviction record does not disqualify applicants from acceptance; factors such as age and time of offense, seriousness and nature of violation and rehabilitation will be taken into account. However, concealment of any conviction on this application shall be cause for disqualification.
Prospective Child Life Volunteers
For those that are interested in learning more about the child life profession or would like to volunteer with our Child Life department, please follow the links below.
Needs of Hospitalized Children
This page will give you an overview of what typical developments expect in your child, their needs, and how to help them during their hospitalization at different age stages. You may also download this page in PDF Format
I am 0-4 months old
Play:
- I like soft music, singing and rocking.
- I like to play with small rattles and look at mobiles.
- Please talk to me in a low voice.
- I also like to play in front of a mirror.
Social:
- I begin to smile in response to other’s smiles at 6 – 8 weeks old.
- I can show pleasure by making funny noises.
- I love to be rocked and sung to.
- I sleep off and on between feedings, and for about 4 – 6 hours a night.
- You can interact with me by holding me in front of your face, talking about everything you are doing, and moving my arms and legs.
Sleep:
- I need 15-20 hours of sleep per day.
What I can do with my body:
- I can calm myself by sucking.
- I like to use my hands to reach for objects.
- I do not have very good head control, but I’m working on it.
- I like to be rocked.
- Please prop me in your lap so I can see what people are doing.
Concerns I have about being in the hospital:
- I do not like to be separated from my caregiver's.
- I do not get my usual stimulation.
- I am in an unfamiliar setting.
- I am out of my usual routine.
How can you help me while I am in the hospital?
- Please bring my favorite things from home.
- Take me out of my bed when I am awake.
- Let my caregiver be with me as much as possible.
- Provide me with stimulations that I can see, hear, and touch.
- Let me see lots of colors and shapes.
- Think of ways that I can have a routine “play time”.
I am 5 - 10 months old
Play:
- I like to play peek-a-boo.
- I like toys that I can push or pull.
- I love putting everything in my mouth.
- I like large soft toys, rubber rings, blocks and toy keys.
- Banging objects and throwing toys is also fun.
Social:
- I can recognize familiar people and objects.
- I want to explore my environment.
- I can laugh aloud.
- I wiggle around when I get excited.
- I know how to get someone’s attention through crying or making noises.
Sleep:
- I need 14-16 hours of sleep per day.
What I can do with my body:
- When I am young, I like to roll around and work on sitting up.
- As I get older, I may begin to pull up on objects and work on crawling.
- I am learning to pick up small things with my fingers (I like finger foods).
- I can point to show the things I want.
- I like to roll balls on the ground.
Concerns I have about being in the hospital:
- I am afraid of strangers.
- I do not like being separated from my caregiver.
- Please find a comfortable position in which to hold me.
- Do not disturb me when I am sleeping, it will disrupt my routine for the rest of the day.
- I get bored being in my room all the time.
How can you help me while I am in the hospital?
- Please bring my favorite things from home.
- Take me out of my bed to play; I need different stimulation.
- Let my caregiver be with me as much as possible.
- Provide me with stimulations that I can see, hear, and touch.
- Think of ways that I can have a routine “play time”.
- Playing on a floor mat is a great way for me to get stronger and perfect my physical skills.
- Play time is best if it is in a playroom or a place where there is new stimulation.
- During procedures, let me sit comfortably in my caregivers lap.
I am 11 - 15 months old
Play:
- I love peek-a-boo and patty-cake.
- I like toys that I can poke, bang, pull and twist.
- I like to put objects in a container and dump them out.
- I can pretend to care for dolls and animals by feeding and holding them.
- I like stacking blocks, the older I am the more I can stack.
Social:
- I need my caregiver in the room with me so I don’t get scared in strange places.
- I love looking at myself in the mirror.
- I like to imitate adults, especially when they make animals noises.
- I can listen and wiggle my body to music.
- As I get older I can repeat words that I hear.
- Please read me books, this helps me learn common words.
Sleep:
- I need 14-16 hours of sleep per day.
What I can do with my body:
- I will climb on everything.
- I can stand on my own, and am learning to take a few steps.
- I like to use my fingers to pick up small toys.
- I like to pound objects to see how loud I can be.
- I want to be exploring my environment, not stuck in my crib.
Concerns I have about being in the hospital:
- I am afraid of strange people and strange rooms.
- I may try to pull out my tubes.
Development
- I get really frustrated because the medical equipment can hinder my movement.
- I can associate people with pain.
- I need lots of different sights and sounds that can stimulate me.
- I may have more dependent behaviors (I may want to drink from a bottle instead of a cup).
- I may become clingy and whiny when my caregiver is not around.
- My routine may get disrupted, so make sure to create a daily schedule that is similar to what I do at home.
How can you help me while I am in the hospital?
- Give me stimulating activities such as pop-up toys, trucks or dolls that make noise, containers I can put things in and out, and blocks for stacking.
- Talk to me in a calming voice during procedures.
- Let my caregivers help with my care as much as possible.
- Provide a safe place for me to play (playrooms are great, but a mat on the floor is good too).
- Ask me about my favorite toys from home so you can provide similar activities that I normally play with.
I am 16 - 20 months old
Play:
- I like to build block towers and then knock them down.
- When you read to me, I like to point out pictures and turn the pages.
- I like to imitate adults (like pretending to talk on the telephone and taking care of my stuffed animals).
- I like when you hide my toys under or behind objects so I can find them.
- I can scribble with crayons.
- I like toys that I can take apart.
Social:
- I love saying “NO!”, so be careful not to ask me yes or no questions but rather give me options between two things.
- I have a short attention span.
- I can understand simple commands and answer yes or no questions.
- I like for you to hand me things and then let me hand them back to you.
Sleep:
- I need 14-16 hours of sleep per day.
What I can do with my body:
- I am learning to have better balance and coordination.
- I may begin running.
- I can pickup and play with toys from a standing position.
- I can shift crayons and marker from one hand to another.
- I am able to walk backwards.
Concerns I have about being in the hospital:
- I am afraid of strangers and strange places.
- I get very tearful when my caregiver is gone.
- I remember people that cause me pain.
- I do not like being confined to my room, especially if I have to stay in my crib.
- My daily routine is disturbed, so make sure to create a daily schedule that is similar to what I do at home.
- I may respond to nurses and doctors with aggression.
How can you help me while I am in the hospital?
- Provide me gauze so I can wrap up my stuffed animals to look like me.
- Play games with me in my room.
- Let my parents help with my care as much as possible.
- Ask my parents ways that my environment can be as normal as possible.
- Let me help during procedures by playing with the gauze or alcohol wipe.
I am 21 - 24 months old
Play:
- I like to build block towers and then knock them down.
- When you read to me, I like to point out pictures and turn the pages.
- I like to imitate adults (like pretending to talk on the telephone and taking care of my stuffed animals).
- I can scribble with crayons.
- I like toys that I can take apart.
- I like toys that make noise.
- I have favorite toys and dolls.
Social:
- I love saying “NO!”, so be careful not to ask me yes or no questions but rather give me options between two things.
- My vocabulary is increasing every day (I know up to 300 words, and can say 2 word combinations).
- I can show affection by giving hugs and kisses.
- I can understand simple commands and answer yes or no questions.
- I like you to hand me things and then let me hand them back to you.
- I have a strong sense of what is “mine”.
Sleep:
- I need 12-16 hours of sleep per day.
What I can do with my body:
- I can ride tricycles.
- I can jump from low objects.
- I can kick a ball.
- I can drink from a straw.
- I am learning to feed myself with a fork and spoon.
Concerns I have about being in the hospital:
- I am afraid of strangers and strange places.
- I get very tearful when my caregiver is gone.
- I remember people that cause me pain.
- I am not getting enough normal stimulation.
- My daily routine is disturbed, so make sure to create a daily schedule that is similar to what I do at home.
- I may be afraid to explore my environment.
- I may become afraid of the dark.
How can you help me while I am in the hospital?
- Find time for me to have safe play opportunities with new things.
- Play games with me in my room.
- Let my parents help with my care as much as possible.
- Ask my parents ways that my environment can be as normal as possible.
- Let me help during procedures by playing with the gauze or alcohol wipe.
I am 2 - 3 years old
Play:
- Playing helps me master my environment.
- I can match pictures, objects and sounds.
- I use play to learn and work through fears and express myself.
- I like to listen to you talk to me and tell me about what you are doing.
- I love playing with Play-Dough and other squishy textures.
Social:
- I can understand “now”, “soon” and “later”.
- I am able to repeat stories from books.
- I can show jealousy.
- I can use my words to make requests.
- I am gaining a sense of control and confidence in my abilities.
- I have a hard time understanding others point of view and am only concerned with MY thoughts.
Sleep:
- I need 10-14 hours of sleep per day.
What I can do with my body:
- I can put on my clothes but have trouble with zippers and laces.
- I can feed myself with a fork and a spoon.
- I can stand in place and hop on one foot.
- I can sleep 10 hours a night.
Concerns I have about being in the hospital:
- I feel like I am losing control and autonomy.
- I am scared to move with IVs and other medical equipment connected to me.
- I may regress in my abilities (potty training) and act like an infant.
- I have a strong fear of strangers.
How can you help me while I am in the
hospital?
- Tell me what you are doing and what it is going to feel like.
- Allow security objects to accompany me to procedures (ie blankets, stuffed animals, pacifiers or dolls).
- Provide me with opportunities for choice and control (you can ask me if I want cherry or grape flavored medicine).
- Blowing bubbles and singing songs can be helpful during procedures.
- I am improving my self help skills, so encourage me to do things on my own.
I am 3 - 5 years old (preschool)
Play:
- I love coloring and drawing.
- I enjoy imaginative play (i.e. pretending to be a parent or a doctor).
- I love showing off my accomplishments.
- I like cutting paper and finger painting.
- I can build structures that symbolize other things such as animals or buildings.
Social:
- I am beginning to have an understanding of time.
- I have a great imagination, which can lead to misconceptions about the hospital.
- I have difficulty separating make-believe from reality.
- I can separate from my parents for short periods of time.
- I am able to learn rules and obey them.
Sleep:
- I need 10-14 hours of sleep per day.
What I can do with my body:
- I can draw circles and squares.
- I can can feed self, brush teeth, comb hair, wash, dress, hang up clothes with little assistance.
- I can form shapes and objects out of clay or play dough, sometimes human and animal figures.
- I can thread small beads on a string.
Concerns I have about being in the hospital:
- I fear long separations from my loved ones.
- Medical procedures can be seen as a punishment.
- Imagining what a procedure is going to be like can be worse than reality; I NEED to be told the truth.
- I feel a sense of loss of control.
- Unknown events scare me.
How can you help me while I am in the hospital?
- Reinforce that illness is not the child’s fault and treatment is not the child’s punishment.
- Give clear explanations as magical thinking and fear of bodily injury is common.
- Encourage parental participation, verbalization and social interaction and give positive reinforcement.
- Set limits and provide structure.
- Allow child to manipulate and explore medical supplies and their purpose.
- Provide preparation for any procedure or “new” thing they will experience.
- Give them a job during procedures (blowing a pinwheel or looking at a book will help them learn coping strategies).
I am 5-11 years old (school aged)
Activities:
- I enjoy playing board games and video games.
- Being with friends becomes increasingly important.
- Organized and group play creates a sense of security.
- School aged children love to talk about themselves and what they like.
Social:
- I have a strong desire to perform well, do things right.
- I have interest in new skills.
- I want to earn recognition and be successful.
- I am independent and modest.
- I have an increased anxiety of missing school.
- I am learning social cooperation and appropriate behaviors.
- I talk about my feelings.
Sleep:
- I need 8-12 hours of sleep per day (varies by age, younger children need more).
Physical Issues:
- Puberty can be a source of anxiety (girls may begin menstruation).
- Differences between peers can be a source of anxiety and self consciousness.
Concerns I have about being in the hospital:
- Disgrace, loss of competence
- Compromised body image
- Invasions of privacy
- Loss of status in peer group
- Death and disability
- Hesitant to reveal fears
- Loss of body control
- Enforced dependence
How can you help me while I am in the hospital?
- Reinforce that illness is not the the child’s fault and treatment is not the child’s punishment.
- “All about me” posters help the child feel in control and allows staff to know the child’s likes and dislikes.
- Allow choices when possible (give them choice of IV location).
- Provide activities and games in order to make atmosphere more normal.
- Preparation for procedure is important to reduce anxiety associated with the unknown.
- Allow children to explore medical equipment and rehearse upcoming procedures.
I am 13+ years old (adolescent)
Activities:
- I enjoy playing board games and video games.
- Being with friends is extremely important.
- Cell phones and e mail may be an important way to allow patient to keep in touch with friends.
Social:
- I have a strong desire to perform well, do things right.
- I have an interest in new skills.
- I want to earn recognition and be successful.
- I want independence and privacy.
- I have an increased anxiety about missing school.
- I am learning social cooperation.
- I can verbalize feelings.
Sleep:
- I need 8-12 hours of sleep per day (varies by individuals).
Physical Issues:
- Puberty can be a source of embarrassment and frustration.
- Sexual development and body image are on the forefront of their minds; be sure to address how procedures and surgeries may impact this.
- Body image and self-worth can be tormenting issues for both males and females.
Concerns I have about being in the hospital:
- Compromised body image
- Invasions of privacy
- Loss of status in peer group
- Death and disability
- Hesitant to reveal fears
- Forced dependence on medical equipment and nursing staff can be frustrating
- Fear of failure in school
- Teenagers may hide from confusion and lack of understanding.
How can you help me while I am in the hospital?
- Respect individual as separate from parents.
- Altered body image, privacy and peers are paramount.
- Involve teenagers in medical responsibilities and decision-making.
- Peer socialization will benefit patient.
- Preparation will help teenagers learn about and cope with procedures and diagnosis.
This content was provided by Vanderbilt University Medical Center 2008.
Support & Advocacy for Pediatric Healthcare
Nicklaus Children's commitment to being 'where the children are' means providing more than just top-rate medical care to our patients. Nicklaus Children's Hospital actively advocates on behalf of children and pediatric healthcare throughout the region, state and country. We also encourage participation by both our patients and their families in our Teen Council and Family Advisory Council as we work towards making every stay at Nicklaus Children's Hospital as pleasant as possible. Through summer camps, support groups, and fun activities supported by Radio Lollipop, Nicklaus Children's Hospital helps children cope with their condition and their time in the hospital.
Our Role: An Advocate for Children's Health
The mission of the Public Policy and External Affairs Department is to enhance child health advocacy at Nicklaus Children's Hospital. This office collaborates its efforts with our friends and colleagues in the community to reach out to local, state and federal officials in order to educate and create awareness on the need for, and importance of quality healthcare for children.
Our department is also responsible for:
- Serving as a resource on legislative and regulatory issues that affect children's health
- Representing Nicklaus Children's Hospital and staff in organizations that support the health and well-being of children
- Coordinating grassroots advocacy efforts within the hospital community
- Working with other organizations to support the health and well-being of children
 Tell Congress To Support Childhood Cancer And Pass The STAR Act
Tell Congress To Support Childhood Cancer And Pass The STAR Act
The Childhood Cancer Survivorship, Treatment, Access, and Research (STAR) Act would advance pediatric cancer research, increase transparency and expertise for pediatric cancer research at the National Institutes of Health (NIH), ensure pharmaceutical companies have publicly accessible compassionate use policies, and expand research into the long-term side effects due to childhood cancer and its treatments.
Legislature Contact
Nicklaus Children's Hospital, maintains strong working relationships with elected officials representing children throughout South Florida. Our Advocacy Team is actively engaged in keeping our elected representatives informed and aware of issues affecting our children.
United States Senate
- The Honorable Rick Scott
502 Hart Senate Office Building
Washington, DC 20510
(202) 224-5274
- The Honorable Senator Marco Rubio
284 Russell Senate Office Building
Washington, DC 20510
(202) 224-3041
marcorubio@senate.gov
To find your elected officials write in your zip code below or, for a complete list of senators in other states, click here.
United States House of Representatives
The Honorable Maria Elvira Salazar
1616 Longworth House Office Building
Washington, DC 20515
(202) 225-3931
For names and addresses of U.S. Representatives, visit the US House of Representatives website.
- U.S. Capitol Switchboard: You can also contact elected officials by calling the U.S. Capitol switchboard at (202) 224-3121.
- Florida House of Representatives: Danny Perez
- Florida Senator: Annette Taddeo
- Miami-Dade County Mayor: Daniella Levine Cava
- Miami-Dade County Commissioner: Rebeca Sosa
To obtain the name and contact information of your Florida State Legislators click here.
Frequently Asked Questions
The following questions and answers are based on materials provided by the National Association of Children's Hospitals and Related Institutions (NACHRI).
Who are children's advocates?
Anyone who has ever spoken on behalf of a child. It's that simple.
What is legislative advocacy?
Almost anything done to influence a legislator's position on legislation or public policy. Writing letters, making phone calls, visiting legislators and testifying before committees all come under the heading of legislative advocacy. A lot of advocacy is just a matter of individual, private citizens speaking out by writing, calling and meeting with their legislators and other public officials. It means literally "to plead the cause of another." Legislative advocacy just carries that "pleading" into the legislative or public policy arena and does it on behalf of people we may not know personally. It is a practical way for individuals to translate their concerns about children into policies and laws.
Why is legislative advocacy important to children and Nicklaus Children's Hospital?
Public policy is critical to children's health and the ability of Nicklaus Children's Hospital to serve them. Children have different health care needs than adults, they represent only a small fraction of the health care marketplace, and they are the poorest segment of the population. As a consequence, they don't have the economic clout to command attention sufficiently to ensure all their needs are met. That is why legislation establishing public policies on children's health is so important. Government programs already pay for the health care of more than a quarter of all children and an even larger percentage of children with special health care needs. Government programs also pay for, on average, nearly half of the patient care provided by children's hospitals.
What is grassroots legislative advocacy?
Grassroots legislative advocacy encourages many individuals who share the same concerns to speak up about those concerns when they talk to legislators and elected officials. In the children's hospital community, it means bringing together many people who care about children and children's health and organizing them to communicate with elected officials in an effective and efficient way, such as letter writing, phone calls and personal visits.
Why is grassroots legislative advocacy important for children?
In a 1995 report issued by the State Legislative Leaders Foundation, hundreds of state legislators from across the country were asked about the effectiveness of children's advocates. This study and others show that legislators rarely hear from their constituents about children's issues. We can't afford for issues that impact children to be decided by elected officials who are unfamiliar with children's needs.
Who are grassroots advocates?
Examples of people who have become grassroots advocates for children's hospitals are administrators, doctors and nurses, other health care professionals, trustees, volunteers, parents and hospital donors.
Why should you become a grassroots advocate for children?
In order to build a better future for our children, we need to actively participate in public policy debates and help shape decisions that will influence the future. Grassroots legislative advocacy is the bridge between imagining a better life for children and taking the concrete steps to make it a reality. Your participation as a grassroots children's advocate will ensure that all of our elected officials are hearing regularly from the "folks back home" about what is important for children.
Is it legal for me to be a legislative advocate?
Federal and state governments limit the amount of legislative advocacy in which nonprofit organizations may engage, but there are no such limits on private citizens who act on their own time. In fact, legislative advocacy by a private citizen is a constitutional right of every citizen, protected by our Bill of Rights just like freedom of speech and freedom of religion. The writers of our Constitution recognized that our democratic system works best when individual citizens are fully engaged, advocating their views on public policy to their legislators.
Links
We invite you to visit the following sites for more information about becoming an effective advocate on children's health and safety issues:
Federal
State
Local
Associations
Links available in this page are not necessarily endorsed, reviewed, or sponsored by Nicklaus Children's Hospital. By clicking on any of the links, you will be leaving Nicklaus Children's Website.
Advocacy Message Tips
As an advocate for children's health and safety, you will be in contact with elected officials on the local, state and federal level. It is important to be able to communicate effectively with your legislative leaders. Here are some tips for delivering your advocacy message.
Tips for Effective Letters, Faxes and Emails
- Write to the legislators who represent your district.
- Fax or email your letter if the time frame for action is short.
- Limit your letter to one or two pages.
- Clearly state your position on a particular issue.
- Give your credentials when appropriate.
- Ask the legislator to take a particular action.
- Request a letter stating the legislator's position on the issue.
- Express your appreciation for past or future support.
- Send a copy of your letter to Public Policy & External Affairs Department, Nicklaus Children's Hospital, 3100 SW 62 Avenue, Miami, FL 33155-3009.
Tips for Making Effective Phone Calls
When time is short, a personal phone call may be the most effective method to communicate your views.
- If you don't know the legislator, ask to speak with the assistant who handles health issues.
- If you can't reach a legislative assistant, leave a concise message.
- Once you reach the legislator or assistant, focus on a single issue.
- Have talking points - or your own notes - in front of you when you call to stay focused on the message you want to deliver.
- Mention the local impact of the issue on the legislator's constituents.
- Clearly state the action you wish the legislator to take on the issue.
- Limit your call to no more than three or four minutes.
- Leave your name and telephone number in case a staff member has any further questions.
- Send a thank-you note.
- Keep a record of the conversation. If you spoke to an assistant, write down that person's name, so you can ask for him/her next time.
- Inform the Public Policy & External Affairs Department of your conversation via letter, fax or email.
Sponsor a Special Event
Thank you for your interest in hosting a Special Event for our patients and families at Nicklaus Children's Hospital. We welcome your Special Event ideas.
What is a Special Event?
Special Events refer to visits that allow our patients the opportunity for hands-on participation and involvement via unique experiences and activities. Since many of our programs already provide ample craft and play opportunities daily, we value your creativity in proposing a visit which will provide our patients with a “one-of-a-kind” activity. This is your time to explore your talents and skills and share them with our patients and families!
ALL GUESTS ATTENDING MUST READ, COMPLETE AND SIGN the below application agreement.
Ideas for Special Events:
- Theater Performances
- Licensed Character Visits
- Seasonal Celebrations/Themed Carnivals
- Engaging Craft Activity
- Athlete Meet & Greets
- Musical Concerts
- Watch Parties
- Special Giveaways
Please ensure that your proposed idea will be enjoyable to a wide audience. Nicklaus Children's Hospital serves patients from birth to 21 years of age.
Rules and Guidelines
INFECTION CONTROL
- We recommend up-to-date immunizations, flu and COVID vaccines.
- All special event guests must be in excellent health on the day of the visit.
- For the safety of our patients, special event guests showing signs of fever, cough, or diarrhea on day of visit will be asked to refrain from entering the hospital. The event can be rescheduled for an alternative date.
PATIENT PRIVACY
- HIPAA is a federal law that guarantees patient and family rights to confidentiality and privacy.
- Participants may not inquire about a patient's condition or hospital stay.
- No cell phone photography or personal photography permitted.
- Requests for media, photos or videography must be made in advance of the event. Photos will be shared for use.
ATTENDEES
- No more than FIVE members of the organization may participate, including an adult leader.
- The minimum age of an attendee is 15 years of age.
- All individuals must be accompanied by a Nicklaus Children’s staff member while on the hospital campus or outpatient location.
- Patient participation varies based on hospital admission and patient census.
TOYS & DISTRIBUTION
- Guests may not distribute toys, gifts, food or candy unless approved by the Nicklaus Children’s staff prior to the event date.
- For the safety of our patients, toys and gifts must be NEW and age-appropriate. Please review our toy wish list.
- Balloons: Nicklaus Children’s is a latex-free facility. Latex products, including balloons, are not permitted. Mylar balloons may be used.
- Face paint: only individual and disposable applicators (one sponge/brush per patient) for make-up, face paint, and tattoo applications.
DIETARY RESTRICTIONS
- Catering services by our Food & Nutrition Department is preferred due to patient safety.
- Shelf stable items must be store bought (no homemade foods or drinks) and in a sealed package.
- Items containing peanuts and tree nuts are not permitted due to allergy risks.
ATTIRE
- Individuals must be responsible, friendly, clean and well-mannered.
- No clothing with profane language and/or graphics. No shorts, tank tops, midriffs or miniskirts.
Cancelations must be made no later than 48 HOURS PRIOR to the event.
Nicklaus Children's Hospital staff reserves the right to cancel or discontinue special events at any time if they are thought to be inappropriate or unsafe for patients.
Pediatric Human Patient Simulation Program
Enhancing pediatric healthcare training through medical simulation.
As part of its commitment to excellence in pediatric healthcare, Nicklaus Children's Hospital has developed a state-of-the-art Pediatric Human Patient Simulation Program to support healthcare trainees and professionals in developing and enhancing skills required to provide medical assessment and treatment of children.
The program features a high-fidelity child-sized mannequin with computerized medical simulation that has the capability to mirror the physiologic parameters and medical responses of a young patient. The program also features two infant sized medium fidelity simulators as well. This technology provides a superior learning environment for health care professionals
Simulation technology offers many benefits. It enables healthcare professionals and students to practice relevant pediatric scenarios and acquire basic pediatric care skills. Specifically, it can support healthcare students and professionals in:
- Improving teamwork and building team-leading skills
- Enhancing communication skills
- Developing and improving critical-thinking skills
- Practicing new procedures or testing new equipment
- Enhancing medication administration safety
- Administering medications based on pediatric dosing
- Improving patient assessment and bedside decision making
- Enhancing competency-based assessment skills
- Practicing infrequently used emergency treatment skills
Mission Statement
Through the use of its pediatric human patient simulator lab, the Medical Education Department at Nicklaus Children's Hospital is dedicated to providing state of the art educational opportunities for physicians, nurses, allied health professionals and the community.
Goals
- Improve patient safety and quality of care through team-work and clinical decision-making using medical simulation
- Promote learning in a safe, controlled, non-clinical environment using state-of-the-art teaching tools and medical simulation
- Provide healthcare professionals with an opportunity to demonstrate knowledge basic to pediatrics and clinical practice relevant to pediatrics using medical simulation
About the Nicklaus Children's Hospital Pediatric Human Patient Simulator Model
The Pediatric Human Patient Simulator (PHPS), has the capability to mimic the physiologic responses of a 7-year-old. The PediaSim®, a child-size mannequin from Medical Education Technologies, Inc. (METI), is remarkably lifelike. It can open and close its eyes, talk, inhale oxygen and exhale carbon dioxide, and responds to medications and CPR. The PediaSim®'s programming is based on complex mathematical models of physiology and pharmacology that enable the mannequin to respond to interventions in real-time. This provides trainees with opportunities to immediately experience the impact of treatments. The "health" and well-being of the PHPS is linked directly to how well trainees work together to respond to its needs.
We have now added BabySim® & SimBaby®to extend the range of our simulations and portability. BabySim®is METI’s infant counterpart to PediaSim. Using similar mathematical computations he is able to approximate appropriate physiological responses to learner’s interventions. SimBaby has been designed by Laerdal as a slightly smaller portable infant.
Simulation Scenarios Enhance Education
Simulation is an outstanding tool for acquiring diagnostic skills and practicing medical procedures. Simulation scenarios can range widely in complexity. Some are used simply to review assessment skills, while others significantly alter the patient's underlying physiologic status.
The following are examples of how the Pamela Garrison Simulator can be applied to enhance learning:
- Trainees can assess normal and abnormal heart sounds and breath sounds, perform neurological exams (including pupil response) and cardiovascular exams (including EKG interpretation, blood pressure and differentiation of bilateral pulses)
- Trainees can realistically intubate, start IV lines, cardiovert and defibrillate the simulator and immediately observe the simulator's response
PediaSim® recognizes pharmacologic interventions and will react accordingly
- BabySim & Simbaby both allow many additional procedures to be performed including insertion of chest tubes, needle throacostomy and intraosseus needle placement
- Instructors can customize a "patient" and isolate critical teaching modules to address a trainee's specific needs
- Trainees can be exposed to unusual pediatric emergency situations, allowing them to acquire infrequently used skills and practice them without risk to a real child. In such scenarios, the computer system allows reality to be suspended. PediaSim® becomes a real child undergoing a real emergency
Programs and Customized Courses
Multiple course offerings now can incorporate the pediatric simulation as part of the curriculum.
In addition, the Nicklaus Children's Pediatric Patient Simulator Lab staff can tailor specific training programs to fulfill requests from area healthcare educators, including nursing and allied health professional instructors. The Lab is also available to parents and other caregivers for children with special needs. Pharmaceutical and medical device companies, as well as others interested in research projects, are also encouraged to find out more about the Simulator Lab at Nicklaus Children's Hospital.
The Pediatric Human Patient Simulation Program is made possible through a generous grant from Peacock Foundation. The Pamela Garrison Simulator has been funded by South Florida philanthropist R. Kirk Landon. The purchase of BabySim has been funded by grant from the Hugoton Foundation.
For more information
To learn more about the pediatric human patient simulator or to schedule time in the Pediatric Patient Simulator Lab,
please call 786- 268-1726 or e-mail: simulator.lab@nicklaushealth.org
For Students
At Nicklaus Children's Hospital you'll be encouraged to think creatively,
share your ideas and prove your determination for success!
If you are seeking a challenging and rewarding opportunity where you'll receive:
- Hands on experience
- Collaboration with highly regarded professionals in the medical field
- Possible hiring opportunities after internship completion
- An internship among one of the top Children's Hospitals in the nation
Then Nicklaus Children's Hospital is the place for you!
Nursing Rotations
Nicklaus Children’s Hospital takes pride on investing time to develop the nursing profession and continuing education for all nurses and future nurses. Nicklaus Children’s Hospital recognizes the importance of providing clinical opportunities to ensure nursing excellence and the delivery of safe quality care.
We would like to take this opportunity to commend you for taking on this great journey as a future nurse and choosing Nicklaus Children’s Hospital for your clinical rotation and practicum experience. During your time at Nicklaus Children’s Hospital, you will gain a valuable and worthwhile experience with our nursing staff. We value your dedication to the nursing profession and wish you the best while you are on campus and in your journey as a future nurse.
Before you Begin
You must be approved by your college or university to do your clinical rotation or practicum at Nicklaus Children’s Hospital. Clinical rotations and practicum are approved only if they are done as part of your nursing program.
Once approved by your school, the school representative must request placement in CCPS for any nursing rotation or contact our Education Program/Internship Specialist by email at studentplacement@nicklaushealth.org for any Practicum rotations.
All students requesting to rotate at Nicklaus Children's Hospital must be enrolled in a credit program with an affiliated institution (see our affiliated institutions).
After Approval is Confirmed
Nicklaus Children's Hospital and Health System employees are not able to do their rotations in the same department/center they currently work or during scheduled work hours. They must also follow all student requirements.
Nursing Rotations
Nicklaus Children’s Hospital takes pride on investing time to develop the nursing profession and continuing education for all nurses and future nurses. Nicklaus Children’s Hospital recognizes the importance of providing clinical opportunities to ensure nursing excellence and the delivery of safe quality care.
We would like to take this opportunity to commend you for taking on this great journey as a future nurse and choosing Nicklaus Children’s Hospital for your clinical rotation and practicum experience. During your time at Nicklaus Children’s Hospital, you will gain a valuable and worthwhile experience with our nursing staff. We value your dedication to the nursing profession and wish you the best while you are on campus and in your journey as a future nurse.
Before you Begin
You must be approved by your college or university to do your clinical rotation or practicum at Nicklaus Children’s Hospital. Clinical rotations and practicum are approved only if they are done as part of your nursing program.
Once approved by your school, the school representative must request placement in CCPS for any nursing rotation or contact our Education Program/Internship Specialist by email at studentplacement@nicklaushealth.org for any Practicum rotations.
All students requesting to rotate at Nicklaus Children's Hospital must be enrolled in a credit program with an affiliated institution (see our affiliated institutions).
After Approval is Confirmed
Nicklaus Children's Hospital and Health System employees are not able to do their rotations in the same department/center they currently work or during scheduled work hours. They must also follow all student requirements.
For Physicians
Physician Logins and Forms:
Continuing Education, Medical Journals:
-
Postgraduate Programs: Information about our world renowned "Perspectives in Pediatrics" Postgraduate Course.
-
Continuing Education: The Departments of Medical Education, and Education and Professional Development at Nicklaus Children's Hospital support continuing education for doctors.
-
Medical Library: Information on medline searches, interlibrary loans, codes for 24-hour library access. Learn more.
-
Weekly Updates in Pediatrics: Concise information about a broad range of current pediatric topics to enhance the education of practicing primary care pediatricians.
Read the latest newsletter.
For Residents:
For Nurses
Nationally Recognized Nursing Leadership

The American Nurses Credentialing Center's (ANCC) Magnet Recognition Program® for excellence in nursing services has designated Nicklaus Children's as a Magnet hospital. According to the ANCC, the leading nursing credentialing organization in the United States, Magnet designation is widely accepted as the gold standard of patient care. Only 6 percent of hospitals nationwide have achieved Magnet designation. Nicklaus Children's Hospital, first received this recognition in 2004, becoming only the fifth pediatric hospital nationwide to achieve this distinction which recognizes the nursing staff for meeting the rigorous quality indicators and standards of nursing practice as defined by the American Nurses Association's Scope and Standards for Nurse Administrators. These standards include an environment that fosters leadership, nursing research, staff involvement and innovation in practice, as well as fostering an environment that supports teamwork and collegiality. Our nursing staff works as a team, like no other, to put children and families first.
Nationally Recognized Care
 The Beacon Award for Excellence recognizes unit caregiver teams that successfully improve patient outcomes and align practices with American Association of Critical-Care Nurses (AACN) six Healthy Work Environment Standards. Units that achieve this three-level award with gold, silver or bronze designations meet national criteria consistent with Magnet Recognition, the Malcolm Baldrige National Quality Award and the National Quality Healthcare Award.
The Beacon Award for Excellence recognizes unit caregiver teams that successfully improve patient outcomes and align practices with American Association of Critical-Care Nurses (AACN) six Healthy Work Environment Standards. Units that achieve this three-level award with gold, silver or bronze designations meet national criteria consistent with Magnet Recognition, the Malcolm Baldrige National Quality Award and the National Quality Healthcare Award.
The
Cardiac Intensive Care Unit (CICU) has achieved a
gold level Beacon Award for Excellence in patient care from the AACN. The
Neonatal Intensive Care Unit (NICU) as well as 3 North (Specialty Medical), 3 South (Respiratory), and 5 Tower (Neurology) have achieved silver level.
Nationally Recognized Nursing Education
Nicklaus Children's Hospital has also been recognized as an Accredited Provider by the ANCC. The ANCC Accreditation Program recognizes the importance of high-quality continuing nursing education (CNE), interprofessional continuing education, transition to practice programs, and skills-based competency programs. Around the world, ANCC-accredited organizations provide nurses with the knowledge and skills to help improve care and patient outcomes.
The Horizon Nurse Residency Program was honored with ANCC PTAP National Accreditation with distinction on December 19th, 2017. Practice Transition Accreditation Program (PTAP) sets the global standard for residency programs that transition nurses into new practice settings. Achieving this accreditation elevates the standards of the Horizon Nurse Residency Program at Nicklaus Children’s Health System with ANCC evidence-based criteria, demonstrating excellence in the transitioning nurses from novice to proficient. The Horizon Nurse Residency Program was further developed in 2014 and has transitioned over 240 nurses with a 92% overall retention, since the inception of the program.
At Nicklaus Children's Hospital, you make a difference… all in a place where you can make a lasting impression in the life of a child each and every day. You can help smiles supplant tears and bring laughter where there was fear. Nothing compares to receiving a smile or a hug from a child and seeing them get better.
Nicklaus Children's Hospital, is committed to advancing the understanding and practice of patient and family-centered care in an environment that enhances comfort. At Nicklaus Children's Hospital, you are an integral part of the care team in an environment, supportive of the nurse. It is our goal to recruit and retain top staff and as such, we deliver...
Extraordinary care… by extraordinary people.
Nicklaus Children's Hospital, has also made an organizational commitment to our employees to be an "Employer of Choice" in South Florida. As a part of that commitment, we offer a package of attractive benefits such as tuition reimbursement, flexible scheduling, reward/incentive programs.
Nicklaus Children's Hospital, offers an active nursing research program, the Frida Hill Beck Nursing Education endowment fund to support education and research, a Shared Leadership nursing council/committee structure, career advancement and development, as well as a nursing clinical ladder.
All of these benefits and more enable us to recruit and retain top nursing talent and achieve exceptionally low vacancy and turnover rates that fall well below state and national levels. What’s more, our reputation and location support opportunities for international exchange with nurses throughout the world, with highlights including recent exchanges with nurse leaders from Taiwan, Turkey, Ecuador, Puerto Rico, China, Chile and Italy.
So, come take a closer look at what Nicklaus Children's has to offer.
Join our team!
From the Desk of Shannon Odell, Vice President, Chief Nursing Officer:
 Welcome to the special world of pediatric nursing at Nicklaus Children's Hospital. Our nursing team is proud to be part of the only freestanding hospital exclusively for children in South Florida. We offer careers that are never routine, always challenging and extremely rewarding.
Welcome to the special world of pediatric nursing at Nicklaus Children's Hospital. Our nursing team is proud to be part of the only freestanding hospital exclusively for children in South Florida. We offer careers that are never routine, always challenging and extremely rewarding.
A Special Calling
As pediatric nurses, we have the opportunity daily to make a difference in the lives of children and their families. Our young patients can’t always communicate what they are feeling, so we quickly become experts at interpreting the needs of those we serve, from babies to children and adolescents. It is our honor to be champions for children and to provide clinical expertise and a supportive presence to see them through their healthcare journeys, from routine medical visits to challenging procedures and inpatient stays. We proudly live our organization’s commitment to putting patients and families first in all we do.
National Leadership
Nicklaus Children’s enjoys special status in the nursing field, having attained Magnet recognition from the American Nurses Credentialing Center for the fourth consecutive term. Only a few pediatric hospitals in the nation have achieved a fourth Magnet designation.
The Magnet Difference
Magnet recognition is the gold standard for nursing excellence. The Magnet model, to which we adhere, provides a framework for nursing practice, research, measurement and inclusion of nurses in organizational decision-making. As a result, Magnet hospitals have enhanced patient satisfaction as well as lower nursing turnover and fewer vacancies when compared to hospitals without the designation.
Nurses at Nicklaus Children’s are dedicated, talented, and compassionate professionals who work together to make a better world for children. You can learn more about a career at Nicklaus Children’s by visiting our careers website.
Sincerely,
Shannon Odell, MSN, RNC-OB, NE-BC
Nicklaus Children’s Hospital
Humpty Dumpty Falls Prevention Program™
Medical Education
Welcome to the Department of Medical Education at Nicklaus Children's Hospital. The Department is committed to the oversight and provision of high-quality, evidence-based, and innovative Continuing Medical Education (CME), Graduate Medical Education (GME), and Undergraduate Medical Education (UME).
Nicklaus Children's Health System extends its medical education impact beyond Florida through our educational initiatives in the USA and across the world. Our faculty members are strongly committed to lifelong learning, personal and professional development, and professional and scholarly work. Our medical education programs are based on Adult Learning Principles. Teaching is done using multiple modalities including: live didactic lectures, workshops, multidisciplinary conferences, web-based technology, and simulation.
The Department of Medical Education at Nicklaus Children's Hospital is responsible for:
- Oversight and maintenance of compliance with accreditation requirements for the institution, CME, GME, and UME programs
- Planning and implementation of educational initiatives
- Faculty development
- Partnership and collaboration with local, regional, national, and worldwide educational institutions.
Thank you for considering the Department of Medical Education at Nicklaus Children's Hospital as a source for your medical education needs.
Executive Director of Medical Education
Designated Institutional Official (DIO)
Physician Lead - Diversity, Equity, & Inclusion
Nicklaus Children's Hospital
Nicklaus Children's Health System
Life Support Education (CPR, PALS, NRP, AED, First Aid)
CPR Classes for Friends and Family
A community education courses for parents, grandparents, and care takers. Classes are also available in Spanish, please call to inquire.
CPR Certification Courses
Courses for educators, fitness trainers, security guards, day care workers, camp counselor and coaches. Parents with young children and adolescents are also highly encouraged to attend.
Completing these courses will earn you a 2-year certification.
- Heartsaver® CPR AED - $45
- BLS (Basic Life Support) CPR - $45*
- PALS (Pediatric Advanced Life Support) - $85*
- NRP (Neonatal Resuscitation Program) - $85**
*You must also purchase the BLS ($36) or PALS ($168) course from the American Heart Association prior to attending the course and to complete your certification.
**You must also purchase the NRP 8th Edition Advanced Provider Curriculum ($55) from the American Academy of Pediatrics prior to attending the course and to complete your certification.
Physician Careers
Nicklaus Children's Hospital, a 307-bed freestanding children's hospital and Level III trauma center, and Nicklaus Children's Pediatric Specialists, the physician-led multispecialty group practice of Nicklaus Children's Health System, offer exceptional career opportunities to pediatric specialists.
Nicklaus Children’s Hospital is renowned for excellence in all aspects of pediatric medicine and has numerous subspecialty programs that are routinely ranked among the best in the nation. It is also home to the largest pediatric teaching program in the southeastern U.S. Many of our physicians have trained or worked at other leading medical institutions. Join a phenomenal team that brings lifelong health and hope to children and their families through innovative and compassionate care.
Each year, Nicklaus Children’s Hospital trains:
Our academic affiliation is with Florida International University’s Herbert Wertheim College of Medicine.
Physician Directory
Simulation Lab
Graduate Medical Education (GME)
Undergraduate Medical Education (UME)
Nicklaus Children's Hospital is the site for Third Year Core Pediatric Clerkships for Medical Students from our three Medical School Affilates: Florida International University College of Medicine (FIU), Nova Southeastern University (NSU), and St. George's University (SGU). During their Pediatric Clerkship, medical students rotate in the Emergency Department, on inpatient and outpatient services in both General Pediatric and Pediatric Subspecialty Services. The medical students' curriculum is designed with a blend of clinical experiences, didactic sessions, small group discussions, interactive, and self-directed learning. The curriculum is based on the Pediatric Curriculum designated by the Council on Medical Students in Pediatrics (COMSEP) and is meant to assist the parent institutions to meet the accreditation of the Liaison Committee on Medical Education (LCME) or the American Osteopathic Association (AOA).
Requirements

Third-year core pediatric clerkships and fourth-year subspecialty electives
Only third year students from our affiliated medical schools are eligible to take their core pediatric clerkship at Nicklaus Children's Hospital. However, Nicklaus Children's Hospital offers 4th year electives in various subspecialties to 4th year medical students from LCME or AOA-Accredited Medical Schools in the US and Canada based on availability.

Observerships, rotations, teen programs, and international clinical externships
Nicklaus Children's Hospital does not routinely offer observerships or rotations for national or international observers or shadowers. Students of international medical schools are not accepted for clinical externships. We only allow fourth year electives on our clinical services to those students who are registered and are in good standing at LCME or AOA accredited medical schools. Additionally, we do not have a teen program or program for any students less than 18 years of age.
Fourth-Year Medical Students
Nicklaus Children's Hospital is committed to its role as a teaching hospital providing medical school elective rotations for fourth year medical students throughout most of the departments. Students from LCME (Liaison Committee on Medical Education) or AOA (American Osteopathic Association)-accredited medical schools are eligible for electives at Nicklaus Children's Hospital. LCME is the nationally recognized accrediting authority for medical education programs leading to the M.D. degree and AOA is the nationally recognized accrediting authority for medical education programs leading to the D.O. degree. LCME/AOA medical schools are licensed and accredited medical schools in North America and Puerto Rico. Medical students will be allowed to schedule their rotations 6 months in advance and up to 4 weeks prior to the beginning of a rotation. Approval is based on good academic standing and availability. Medical students enrolled in the FIU College of Medicine are given first priority for all rotations. Non-FIU students may participate in electives only if space is available. Only students who have completed all their third year clinical clerkships and are in good standing in their own medical schools will be accepted.
Students of international medical schools are not accepted for clinical externships.
Subspecialties Offered
Adolescent Medicine
Allergy/Immunology
Cardiac Intensive Care
Cardiology
Cardiovascular Surgery
Emergency Medicine
Endocrinology
Gastroenterology
Genetics & Metabolism
Hematology/Oncology
Infectious Diseases
Nephrology
Neurology
Neurosurgery
Neonatal Intensive Care
Ophthalmology
Orthopedics
Otolaryngology
Outpatient General Pediatrics
Pediatric Critical Care
Pediatric Hospital Medicine
Pediatric Surgery
Plastic Surgery
Pulmonary Medicine
Radiology
Rheumatology
Urology
Radiology
Download Brochure
Application
All requests must be made directly to the Department of Medical Education by submitting the required documentation via the Visiting Student Learning Opportunities/AAMC (VSLO). You will need to have a username and password, which is sent by VSLO once you are authorized by your school. Any requests made outside the VSLO system will not be considered.
After acceptance of your rotation, the Student Affairs Coordinator will contact you with information regarding your rotations. We do not provide lab coats or housing.
For more information or questions, please contact the Medical Education Department at (305) 669-5873 or at Medical.Education@nicklaushealth.org.
Apply on VSLO
Our FIU Affiliation
On Monday, December 10, 2007, Florida International University College of Medicine (FIU) signed an affiliation agreement with Nicklaus Children's Hospital. The affiliation agreement between Nicklaus Children's Hospital and FIU adds an undergraduate dimension to the existing Nicklaus Children's Hospital educational programs. The FIU Department of Pediatrics is based at Nicklaus Children's Hospital, under the leadership of Dr. Jefry Biehler, Chairman of the FIU Department of Pediatrics.
The FIU College of Medicine was approved in 2006 by the Florida Board of Governors and the Florida Legislature. The inaugural class of medical students began their studies on August 3, 2009 following accreditation by the Liaison Committee on Medical Education (LCME).
Continuing Medical Education (CME)
Nicklaus Children's Health System is a CME provider accredited with commendation by the Accreditation Council for Continuing Medical Education (ACCME). Nicklaus Children's Health System sponsors several regularly scheduled series (RSS) and yearly conferences at Nicklaus Children's Hospital and in the community.
Continuing medical education (CME) consists of educational activities which serve to maintain, develop, or increase the knowledge, skills, and professional performance and relationships that a physician uses to provide services for patients, the public, or the profession. The content of CME is that body of knowledge and skills generally recognized and accepted by the profession as within the basic medical sciences, the discipline of clinical medicine, and the provision of health care to the public.
Live CME Courses
NOTICE: Due to the ongoing COVID-19 pandemic, our live courses and sessions are all taking place virtually. Information on participating in these live sessions can be found on our online CME portal, iLearnPeds.com, linked below.
For information regarding a specific event please contact the Medical Education department directly at cme@nicklaushealth.org
Online CME Courses
Note: iLearn works with Firefox, Safari, Chrome, IE 11 and above, iPad, iPhone or Android.
Visit the website: iLearn (www.ilearnpeds.com) (Bookmark it)
Existing NCHS staff, and affiliates with a Nicklaus Children's Hospital email, can log in via Single Sign On by clicking the log-in option on the left, and entering their NCHS email and password.
New and visiting users may create a profile by clicking "Register" on the top right of the page, and create a new visitor account.
Once you create a profile, log in to the site. You can will be able to see any upcoming live events and/or register for any of the existing sessions.
For those seeking CME Credit, you must complete any pre or post tests, as well as any event or speaker evaluations. You will be able to claim and save/print the PDF of the certificate.
Regularly Scheduled Series
Pediatric Grand Rounds
Fridays, 8:00 AM to 9:00 AM - Held virtually via Zoom
Click the link above to view scheduled dates, upcoming speakers, Zoom meeting information, and to complete CME requirements. |
Trauma Conference
Third Thursday of every month - Held virtually via Webex
Click the link above to view scheduled dates, upcoming sessions, Webex meeting information, and to complete CME requirements. |
Tumor Board
Wednesdays - Held virtually via Webex
Click the link above to view scheduled dates, upcoming sessions, Webex meeting information, and to complete CME requirements. |
Faculty Development Seminars
Held Quarterly - Held virtually via Zoom.
Click the link above to view scheduled dates, upcoming speakers, Zoom meeting information, and to complete CME requirements. |
Practical Community Pediatrics (PCP) Seminar Sessions
Held Quarterly - Currently Postponed
These courses are expected to resume in Winter of 2020 in a virtual format. Register on iLearn to be notified of any updates. |
Radiology Conference
Wednesdays, 8:15 AM - 9:15 AM - Currently Postponed
These sessions are expected to resume in Winter of 2020 in a virtual format. Register on iLearn to be notified of any updates. |
Evidence-Based Medicine
Welcome to Nicklaus Children's Hospital Pediatric Evidence-Based Medicine (EBM) website. This site is a complement to the Nicklaus Children's Hospital EBM Curriculum. It is designed to assist students, residents, fellows, and faculty to learn more about EBM in Pediatric practice. The website includes valuable teaching and evaluation tools for faculty, forms that can be used to practice EBM, and EBM resources and links for faculty and learners. We hope that you find this site educational. Please feel free to send us any feedback, comments, or questions!
Objectives
- Supplement the EBM curriculum
- Provide the EBM teacher with teaching tools, worksheets for EBM application, and competency-based evaluation tools to be used in training
- Serve as an educational resource for EBM learners (students, residents, fellows, and faculty) to sharpen and solidify their EBM skills and knowledge
- Highlight existing web-based external EBM resources and links in one place of reference
Goals
The main goal of this website is to share pediatric EBM information, tools, and resources with students, residents, fellows, and faculty and to assist them in teaching and learning Pediatric EBM.
 Rani S Gereige, MD, MPH, FAAP
Rani S Gereige, MD, MPH, FAAP
Director of Medical Education
Nicklaus Children's Hopsital
Fellowship Training Programs
Our Medical Education Leadership
 Rani S. Gereige, MD, MPH, FAAP
Rani S. Gereige, MD, MPH, FAAP
Executive Director of Medical Education
Designated Institutional Official (DIO)
Diversity, Equity, & Inclusion (DEI) Lead
Dr. Rani Gereige joined Nicklaus Children's Hospital in February 2010 as the Director of Medical Education & Designated Institutional Official (DIO). In his role at Nicklaus Children's Hospital, he oversees the Undergraduate, Graduate, and Continuing Medical Education Programs and Faculty Development and serves as the Portfolio Program Manager for the Nicklaus Children's Hospital MOC 4 Portfolio Sponsor Program for the American Board of Pediatrics (ABP) and the American Board of Medical Specialties (ABMS) Multi-Specialty Portfolio. He currently holds a faculty appointment as a Clinical Professor, Volunteer Faculty in the Department of Pediatrics at Florida International University College of Medicine. Prior to joining Nicklaus Children's Hospital, Dr. Gereige served as a Professor of Pediatrics at the University of South Florida (USF) College of Medicine and the Course Director for the Evidence-Based Clinical Practice Course at the USF College of Medicine for the second year medical students.
Dr. Gereige received his medical degree from the American University of Beirut in Lebanon. He subsequently completed a Pediatric residency at University of South Florida (USF)/ All Children’s Hospital followed by one year as Chief Resident. He then completed a Masters Degree in Public Health in Maternal and Child Health at USF. In February 2010, he graduated from the USF Leadership Institute.
At the State level, Dr. Gereige previously served as the chair of the Continuing Medical Education Taskforce in the Florida Pediatric Society/ Florida Chapter of the American Academy of Pediatrics. He also served on the executive board of the AAP Florida Chapter as the Regional representative for Region VIII and the State champion for the Oral Health initiative. Dr. Gereige is a member of Oral Health Florida.
At the national level, Dr. Gereige completed a six year term as member of the national AAP executive committee of the Council on School Health where he served as the newsletter and website co-editor. He also served 6 years terms as a member of the Executive Committee of the AAP Oral Health Initiative and the Executive Committee of the Section on Oral Health where was the NCE Program Chair. In addition to being a fellow of the American Academy of Pediatrics (AAP), he is a member of the Academic Pediatric Association (APA), the American Public Health Association (APHA), the American Pediatric Society (APS), and the Association of Pediatric Program Directors (APPD). He is a member of the Editorial Board of Pediatrics in Reviews where he serves as the CME Editor and manuscript reviewer. At the AAP, in 2018 Dr. Gereige completed 6 years term as a member of the AAP National Conference and Exhibition (NCE) Planning Group. He is currently a member and Chair of the AAP Committee on Continuing Medical Education (COCME) and a member of the NCE Planning Group. In addition he serves as a Faculty Advisor for the APA Educational Scholars Program. Dr. Gereige served on the NBME USMLE Step 2 test writing committee for the Pediatric test questions for 4 years (2007-2011) and has been serving on the USMLE Step 2 Interdisciplinary Review Committee (IRC) since 2012 to present and on the USMLE Scientific Abstracts Test Material Development Committee Since 2020. Dr. Gereige serves as a surveyor for the Accreditation Council on Continuing Medical Education (ACCME). In January 2015, Dr. Gereige was appointed to serve as a member of the Pediatric Residency Review Committee (RRC) of the Accreditation Council of Graduate Medical Education (ACGME) and served on the Pediatric RRC until June 30 2021 where he served as the Vice-Chair of the ACGME Pediatric RRC.
While at USF, he was the Associate Pediatric Clerkship Director for USF Medical Students before assuming the position of the Associate Director of the Pediatric Residency Program for six years followed by the position of the Program Director of the USF General Academic Pediatric Fellowship and the Interim Academic Division Chief for the General Academic Pediatric Division at USF. He also served on the Board of Directors of the USF Physicians Group representing the Department of Pediatrics. He is the recipient of several teaching awards from residents and medical students including the 2002 Arnold P Gold Foundation Humanism in Medicine Award and was nominated for the 2003 AAMC Humanism in Medicine Award. He was listed in the 2009 List of Best Doctors in America. In addition, at USF, Dr. Gereige directed the School Health and Sports Medicine residents and medical students’ rotations and the EBM resident’s curriculum. He designed the curriculum for training residents in school health including an Adopt-A-School program. Dr. Gereige also served as Assistant Medical Director for the Children’s Medical Services in the State of Florida for Pinellas and Pasco Counties.
Dr. Gereige has numerous publications in peer-reviewed journals. He is certified by the American Board of Pediatrics. In addition to Medical Education, his interests include School Health, primary care Sports Medicine, Public Health, Evidence-Based Medicine, Oral Health, and Children with Special Health Care Needs and Sports. He is the recipient of the AAP 2018 National Oral Health Service Award given by the AAP Section on Oral Health.
Milestones Newsletter
Milestones in Education is a newsletter dedicated to highlighting the milestones achieved by members of the Department of Medical Education at Nicklaus Children's Hospital, including students, residents, fellows, alumni, and staff.
Milestones in CME... GME... UME...
Milestones in Scholarly Work
Milestones in Academics
Awards & Recognition
Nursing Awards Archive
Awards received by Miami Children's Hospital Nursing department and outstanding nurses.
2013 Nursing Awards
 FIU 30th Anniversary Gala
FIU 30th Anniversary Gala
Congratulations to Jo Ann Nieves, MSN, ARNP, PNP-BC, CPN, for her recognition at the Florida International University (FIU) 30th Anniversary Gala. Jo Ann received the 2013 Outstanding Achievement Award, Honorable Mention Nicole Wertheim College of Nursing & Health Sciences (Florida International University College of Nursing).
FNA Membership Assembly Great 100 Awards
Congratulations to
Laura M. Hernandez , MSN, ARNP, FNP-BC, CPN. She has been selected as a recipient of the Great 100 Awards by the FNA Membership Assembly.
2011 Nursing Awards
Miami Children's Hospital, March Of Dimes 2011 Miami-Dade and Monroe nurse of the year Finalists and Winners.
- Annalyn Velasquez, ARNP, MSN, CPNP, CCRN, won the Critical Care/Surgical Services category
- Raquel Pasaron, ARNP, DNP, FNP-BC won in the category of advanced practice.
Miami Children's Hospital Finalists
Advance Practice
- Cindy M.Ayala, RN, MSN, CPN
- Patricia Dean, ARNP, MSN
- Jo Ann Nieves, MSN, CPN, ARNP, PNP-BC, FAHA
- Elena Ortega, ARNP, MSN, CCRN
- Raquel Pasaron, ARNNP, DNP, FNNP-BC
Case Management/Care Coordination/Managed Care
- Maytee Perdomo, RNN, AS
- Clinical & Academic Education
- Laura Hernandez, ARNP, MSN, CPN, FNP-C
- Janice Serrano, RN, BSN
Critical Care/Surgical Services
- Lorna Allen, RN, BSN
- Holda Delavoe, RN
- Melinda Duran, RN, BSN
- Claudia Martin-Shimizu, RN, BSN ,CNOR
- Miriam Prado, RN
- Annalyn Velasquez, ARNP, MSN, CPNP, CCRN
Emergency/Trauma
- Holly Olsen-Aloi, RN, BSN
Leadership-Executive
- Jane Bragg, RN, MSN,MBA
- Mirtha Gonzalez, ARNP,MSN
Leadership-Managers
- Diana Garcia, RN, MSN
- Flor Tena, RN, MSN
Pediatric/Adolescent Health
Miami Children's Patricia Dean to Receive American Epilepsy Society’s 2011 J. Kiffin Penry Award
The American Epilepsy Society (AES) has announced that Patricia Dean, ARNP, MSN, a pediatric nurse practitioner and Clinical Coordinator of the Comprehensive Epilepsy Program at Nicklaus Children's Hospital, formerly Miami Children's Hospital, has been named recipient of this year’s J. Kiffin Penry Excellence in Epilepsy Care Award. Jackie Gonzalez, ARNP, MSN, NEA-BC, FAAN, Senior Vice President/Chief Nursing Officer, Was inducted on November 4th as President -Elect 2012 of Florida Organization of Nurse Executives (FONE).Congratulations!
Florida Nurses Association State Award
- FNA, Nursing Administrator of the Year, Jackie Gonzalez, MSN, ARNP-Vice President/Chief Nursing Officer
- FNA, Nurse Practitioner of the Year, Raquel Pasarón, DNP, ARNP, FNP-BC
Florida Nurses Association South Region Symposium and Awards Ceremony held on Saturday, April 16, 2011.
- Laura Hernandez: Nurse Educator Award—Winner
- Diana Garcia: Nursing Administration Award—Winner
- Raquel Pasarón: Advanced Practice Nursing Award—Finalist
- Nicklaus Children's Hospital Nursing Team (Jackie Gonzalez)--Community Action Award—Finalist
- Nicklaus Children's Hospital NICU Nursing Team--Promotion of Excellence Award—Winner
Society for Pediatric Nursing 2011 National Conference in Las Vegas, NV -- Maria Soto, MSN, ARNP, Carmen Duque, MSN, ARNP, Dr. Simpser/2nd place (Clinical Practice Award) - “Caring for the Ventilator Dependent Pediatric Patient in a Medical Surgical Unit” (Poster).
JoAnn Nieves, MSN, ARNP, PNP-BC-on April 30, 2011, was elected as a Fellow of the American Heart Association by the leadership committee of the Council on Cardiovascular Disease in the Young.
2011 Nurse of the Year Winners
- RN of the Year: LifeFlight: Kenneth Patino, BSN, RN, CPN
- LPN of the year: Andres Valencia, LPN
- Rookie of the year: Emergency Department: Lizette Rivera, BSN, RN, CPN
- Leader of the year: IV team and Dialysis: Solfia Torre, BSN, RN, CDN
- Nursing support staff of the year: 2 East- Evangeline Juggan, CA
- Scholar of the year: CICU-Jacqueline Whyte, BSN, RN, CPN
- Professional Services of the Year: 3 South-Patricia Dean, MSN, ARNP, PNP
Unit base winners:
- 2E: Chau Nguyen, BSN, RN
- 2NE: Andrea Downs, RN
- 3N: Annette Caravia, MSN, RN, CPN
- 3E: Inga Bolanos, BSN, RN, CPN
- 3S: Karen Ricketts, RN, CPN
- 2N: Cristina Meca, BSN, RN, CPN
- Same Day Surgery: Jannette Martinez, BSN, RN, CPN
- CICU: Shannon Hutcherson, BSN, RN
- ED/Rapid Care: Carolyn Ramirez, BSN, RN, CPEN
- NICU: Miriam Prado, RN
- OR: Jessica Jameson, BSN, RN
- PICU: Christina Forcine, MSN, RN, CCRN, CPN
- Psychiatry: Shirley Kendzora, RN, MSN, APRN-BC
- PACU: Bill Gehring, RN
- MRI/Radiology: Amy Hollifield, BSN, RN
- UCC: Verna Haik, BSN, RN, CPN
- Minor Procedure Suites: Marlene Marquez, RN
- Pediatric Care Center: Diane Litchman, RN, CPN
- 3NE:Arnold Jumagbas, BSN, RN
- IV Team: Alicia Lue, RN, VA-BC
- Dialysis: Vanessa Polumbarit, BSN, RN
2010 Nursing Awards
Individual Nurse Awards
- RN of the year: 3 Northeast: Rosanne Wills, RN, BSN, CPN
- LPN of the year: 3 South: Lizette Garcia, LPN
- Rookie of the year: 2 North: Cristina Milian, RN, BSN
- Leader of the year: Emergency: Susan Churchill, RN, CPN- Manager
- Nursing support staff of the year: PCC- Judith Bello, CA
- Scholar of the year: OR Support Staff- Raquel Pasaron, MSN, ARNP, FNP-BC
Unit base winners:
- 2E: Anja Thumm, RN
- 2NE: Ann Lisa Marasigna, RN, BSN
- 3N: Jacqueline Arocho, RN, BSN, CPN
- 3E: Lizel Dagum, RN, BSN
- 3S: Leidy Dominguez, RN
- 2N: Michele Moreno, RN, BSN
- Same Day Surgery: Giselle Menendez, RN, BSN
- CICU: Melissa Vidaechea, RN, MSN, PNP-BC
- ED/Rapid Care: Abel Guerrero, RN, CPEN
- Float/Staff Relief: Mayi Ramirez, RN, BSN, CPN
- NICU: Maryanne Pridgen, RN
- OR: Rubin Reinis, RN, BSN
- PICU: Sourrette Joseph, RN, CPN
- Psychiatry: Shirley Kendroza, RN, MSN, APRN-BC
- Quality Resources: Mary Blackburn, RN, CPUM
- PACU: Saadia Cendeno, RN, BSN
- MRI/Radiology: Lizette Gorelick, RN, BSN
- UCC-Palmetto Bay- Kathleen Williams-Atkinson, RN
- LifeFlight: Holly Olsen, RN, BSN, CCRN
- Minor Procedure Suites: Lisa Moose, RN, BSN
- Pediatric Care Center: Teresa Mackenzie, RN, BSN, CPN
American Pediatric Surgical Nurses' Association (APSNA) scholarship grant
Raquel Pasaron, MSN, ARNP, FNP-BC, was awarded the American Pediatric Surgical Nurses' Association (APSNA) scholarship grant at the 19th Annual APSNA Scientific Meeting (May 13-16, ).
DAISY Award Winners
2009 Nursing Awards
2009 Nursing Awards
- Susan Churchill, RN, BSN, CPN- Nominee 2009 South Florida Organization of Nurse Executives (SFONE) Leadership Award.
- Candace Pineda, RN, BSN, CPN- Nominee 2009 South Florida Organization of Nurse Executives (SFONE) Leadership Award.
- Nikole Sanchez- Rubiera, RN, MSN, MBA- Nominee 2009 South Florida Organization of Nurse Executives (SFONE) Leadership Award.
- Elizabeth Padilla, RN, BSN, CPN- Finalist 2009 Nursing Spectrum Excellence Awards, Customer Service
- Sarah Taylor, RN, BSN, CPON- Finalist 2009 Nursing Spectrum Excellence Awards, Management
- Alison Scheflow, RN, MA, BSN, CCRN- Finalist 2009 Nursing Spectrum Excellence Awards, Clinical Care
- PICU Staff - 2009 Best in Collaboration, Advance for Nurses
2009 Nurse of the Year Winners
- RN of the year: 3 South: Carolina Ferraz, RN
- LPN of the year: ER: Michelle Perez, LPN
- Rookie of the year: 3NE: Cristina Suarez, RN
- Leader of the year: LifeFlight: Juliette Edwards, RN
- Nursing support staff of the year: 3 East: Dalva Ferraz, CA
- Scholar of the year: Director of Hematology/Oncology: Debbie Del- Favero MSN/ED, CPN, NE-BC
Unit base winners
- LifeFlight: Joann Dennis, RN
- NICU: Gayle O’Donnell RN
- CV: Diana Arias, RN
- Same Day Surgery: Jennifer Stringer, RN
- PACU: Susan Goldstein, RN
- OR: Danny Monroe, RN
- ER: Donald Torres, RN
- PICU: Melinda Duran, RN
- Radiology: Raquel Morales, RN
- 3S: Carolina Ferraz, RN
- 3E: Nancy Breen, RN
- 3NE: Jocelyn Reyes, RN
- 3N: Michelle Bursztein, RN
- Psych: Yoely Hernandez, RN
- 2E: Stephanie Whitley, RN
- Patient access: Grisel Cepeda, RN
- 2NE: Stefania Sarno, RN
- 2N: Ana Perez, RN
- Ancillary: Meiling Marenco
DAISY Award Winners
2009 Nursing Awards
2009 Nursing Awards
- Patricia Dean, MSN, ARNP, PNP-BC- 2008 Hospital Hero of the Year from the Florida Hospital Association (FHA).
- Deborah Del-Favero, MSN, RN, NE-BC, CPN- Nominee 2008 South Florida Organization of Nurse Executives (SFONE) Leadership Award.
- Jackie Gonzalez, MSN, ARNP, NEA-BC, FAAN- 2008 Alumni of Distinction Award, University of Miami
- Evelyn Gonzalez-Morlate, RN-BC, MSN- 2008 Professional Advocate, Advance for Nurses
2008 Nurse of the Year Winners
- RN of the year: CICU: Emily Zubira, RN, BSN
- LPN of the year: MRI: Teresa Sanchez, LPN, (now RN)
- Rookie of the year: PICU: Janice Serrano, RN, BSN
- Leader of the year: PICU: Pat Thorpe, RN, BSN
- Nursing support staff of the year: 3 Northeast: Reyna Amador, CA
- Research Award Winner: Joanne Nieves, MSN, ARNP, PNP, CPN
- Evidence Based Practice Award: Alison Scheflow, RN, BSN, CCRN
Unit Winners
- 2E: Rochelle Gabas, RN, BSN
- 2NE: Monica Brown, RN, MSN, CPN
- 3N: Tracee Smith, RN, BSN
- 3NE: Adam Fader, RN, BSN
- 3S: Claudia Alfonso, RN
- Same Day Surgery: Irene Bowers, RN
- 3E: Vivian Gimon, RN, CPN
- ED/Rapid Care: David Pastor, RN, BSN, CPN
- Float/Staff Relief: Lisa Morgan, RN, MSN
- NICU: Viviana Gonzalez, RN, BSN
- OR: Enio Ortega, RN, BSN
- PICU: Sandra Wiley, RN, BSN
- Psychiatry: Nova Franklin-Bremmer, RN
- Quality Resources: Charity Zayas, RN
- PACU: Maria Morales-Ojeda, RN
- MRI/Radiology: Margot Sarratea, RN, CPN
- South Dade Center: Carmen Rodriguez, RN, BSN, CPN
- Support Department: Jane Salvaggio, ARNP, MSN
- IV Team: Alicia Lue, RN
- Pediatric Care Center: DeDe Lichtman, RN, BSN
- Afterhours: Monica Hawkins, RN, BSN
2007 Nursing Awards
2007 Nursing Awards
- Dottie Thomas, RN, BSN, CIC - Miami Dade Health Care Hero Award Recipient
- Jeanette Diana, MSN, ARNP - Sigma Theta Tau, Beta Tau Chapter- Leadership Award
- Deborah Hill-Rodriguez, MSN, ARNP, CS-BC - Florida Nurses Association District V- Promoting an Environment for Excellence of Nursing Practice
- Michelle Burke, MSN, ARNP, CPN, CPON - 2007 Jean Fergusson Excellence in Pediatric Hematology/Oncology Nursing Education Award, American Pediatric Hematology/Oncology Nurses Association
- Maria Fernandez, MSN, ARNP, MBA, CFRN – 2007 Florida Flight Nurses Association Transport Nurse of the Year
- Jill Tahmooressi, RN-BC, MBA - 2007 Nursing Spectrum Nursing Excellence Awards for the Florida region, finalist in the category of Advancing and Leading the Profession
- Jean Buckley, RN - 2007 Nursing Spectrum Nursing Excellence Awards for the Florida region, finalist in the category of Community Participation
2007 Nurse of the Year Winners
- RN of the year: 3East: Johnny Mok, RN
- LPN of the year: 3South: Lizette Garcia, LPN
- Rookie of the year: 3Northeast: Liane Franquiz, RN
- Leader of the year: CICU: Ingrid Gonzalez, MSN, RN, CPN
- Nursing support staff of the year: Psychiatry: Saskia Izaquirre, BHT
- Research Award Winner: Carolyn Domina, ARNP, MSN, NE-BC, CORN & Carol Roach, RN, MSN, CPN
Unit Winners
- 2E: Ana Arrubla, RN, BSN
- 2NE: Marocon Villnueava, RN, BSN
- 3N: Sylvia Perez, RN, BSN
- 3NE: Jean Buckley, RN
- 3S: Beatriz Milian, RN, BSN
- Same Day Surgery: Ana Ruiz, RN, BSN
- CICU: Susan Flores, RN, BSN, CPN
- ED/Rapid Care: Susana Sanchez, RN
- Float/Staff Relief: Elizabeth Padilla, RN, BSN, CPN
- NICU: Janet Madill, RN
- OR: Karen Witsken, RN
- PICU: Vivian Lacandalo, RN, BSN
- Psychiatry: Shirley Kendroza, RN, MSN, APRN-BC
- Quality Resources: Grisel Cepeda, RN
- PACU: William Gehring, RN
- MRI/Radiology: Veronica Rivera, RN, CPN
- South Dade Center: Verna Haik, RN, CPN
- Support Department: Cindy Garlesky, ARNP, MSN, CEN, RN-BC
2006 Nursing Awards
2006 Nursing Awards
The Wonder of a Nurse - 2006 Miami Children's Hospital, Nursing Essay
Winner: Sara Turpel, RN, MSN, CCRN
Cheryl Minnick, BSN, RN, Bing Wood, ARNP, MSN, Deborah Hill-Rodriguez, MSN, ARNP, CS,BC, Patricia Messmer, PhD, RN, BC, FAAN, Maryann Henry, RN, Dania Vasquez, ARNP, MSN, and Deborah Salani, MSN, ARNP,BC, CPON - Won the 1st place for the poster "Implementing the Humpty Dumpty Falls Assessment Program" at Fifth Annual 2006 Summer Institute on Evidence-Based Practice Quality Improvement, Quality Indicators in San Antonio, Texas.
Deborah Hill-Rodriguez, MSN, ARNP, CS,BC, Patricia Messmer, PhD, RN, BC, FAAN, Jill Tahmooressi, RN,C, MBA - Research Poster Award for “Pediatric Nurses’ Perception of National Certification”. Society of Pediatric Nursing 16th Annual Convention, Orlando, Florida.
Sofia Morales, MSN, ARNP, CPN- Poster titled "Italian Connection: Nursing Care Across Cultures" won best poster at the 22nd Annual Pediatric Nursing Conference in Dallas, Texas.
Julissa, Jimenez, ARNP, MSN a nurse on the Cardiac Intensive Care Unit was selected to present her exemplar, "A Transcultural Experience with Kosovo Mothers and their Children Diagnosed with Congenital Heart Disease" at the 2006 Florida Nurses Association 19th Annual Ingeborg Mauksch Clinical Excellence Conference February 17, 2006 in Fort Myers, Florida.
Department Awards
The Emergency Department was named one of four "Best Teams" by Advance for Nurses for Achievement in Emergency/Trauma Care.
Individual Nurse Awards:
- 2E – Lilly Alexander
- 2NE – April Anderson
- 3E – Nubia Albites
- 3NE – Karen Murray
- 3N – Sarah Taylor
- 3S – MaJomela Nagal
- After Hours – Teresita Febre
- Ambulatory – Jennifer Gamad
- CICU – Thomas Flock
- ER/OP/Rapid Care – Lisette Gorelick
- Float/SR – Bonnie Flagley
- IV Team – Irma Vergara
- NICU – Heather Leidich
- OR – Christopher Wolary
- PICU – Isoldy Augusten
- Psych – Shirley Kendzora
- Quality/UR – Griselle Angulo
- Recovery Room – Lilia Alonso
- South Dade – Kathleen Atkinson
- Support Staff – Lourdes Lam
- Rookie of the Year – Geeta Singh
- LPN of the Year – Lissette Morales
- Mentor of the Year – Joann Wiacek-Krupin
- Nursing Support Staff of the Year – Ainsley Bryan, Behavioral Health Tech – Psychiatry
2005 Nursing Awards
2005 Nurse Awards
Jackie Gonzalez Selected as Fellow of American Academy of Nursing
 Jackie Gonzalez received recognition from Barry University School of Nursing (pictured with Dean Pegge Bell & Thomas Rozek) for Community Leader Tribute on February 19th, 2005 at the Conrad Hotel, Miami.
Jackie Gonzalez received recognition from Barry University School of Nursing (pictured with Dean Pegge Bell & Thomas Rozek) for Community Leader Tribute on February 19th, 2005 at the Conrad Hotel, Miami.
July 11, 2005 - Jackie Gonzalez, MSN, ARNP, Senior Vice President/Chief Nursing Officer has been named as a Fellow of the American Academy of Nursing (AAN). Fellows are selected by their peers for outstanding contributions to the Nursing profession and healthcare.
The criteria for selection of Fellows requires evidence of outstanding and broad contributions to Nursing and healthcare as well as evidence of strong potential for continuing influence in practice and health policy aimed at improving the health of the American people.
Jackie is a devoted and inspiring leader who has instilled a passion for excellence and innovation within the nursing team at Nicklaus Children's. Her selection as a Fellow of AAN is a tribute to her leadership here at the hospital as well as her commitment to the profession of Nursing on a regional and national level. All of us at Nicklaus Children's are enormously proud of her many achievements.
Seven FNA District V awards were awarded to Nicklaus Children's Hospital nurses at the FNA District V luncheon on Saturday, April 30, 2005:
- Jane Bragg, RN, MSN, MBA,CPON, CNAA,BC Director of Psychiatry and Hematology-Oncology received the FNA District V Nurse Administrator Award
- Lisa Burton, ARNP-BC, MSN, ARNP for Psychiatry received the FNA District V Advanced Practice
- Carolyn Domina, ARNP, MSN, CNA, BC, Director of Operating Room received the FNA District V Community Award
- Patricia R. Messmer, PhD, RN,BC, FAAN Nurse Researcher and Chair of the Nurses Charitable Trust, District V, FNA on behalf of the trust received the FNA District V Special Recognition Award
- Kris Roberts, MSN, RN,CPN, Nurse Manager 2E, received the FNA District V Nursing Student Liaison Award
- Dottie Thomas, RN, BSN, CIC Infection Control Nurse was one of the 6 national finalists for the Sharps Injury Prevention Award.
- Dania Vasquez, ARNP, MSN, CNS 3 East/3South received the FNA District V Nursing Student Liaison Award
Individual Nurses Awards
- Nursing Profession: One Profession, Many Roles
- 2005 Nicklaus Children's Hospital, Nursing Essay Winner: Lisa Capezzuto, RN, 3 South
- Jane Bragg, RN, MSN, MBA,CPON, CNAA,BC Director of Psychiatry and Hematology-Oncology received the FNA Nurse Administrator Award in Bonita Springs, FL September, 16, 2005
- Connie Fishman, BSN, RN was a finalist for Nursing Spectrum of the Year award (one of 5 selected from 48 nurses statewide)
- Miami Children's Hospital, Nurses received Certificates of Recognition from PNCB for the Pursuit of Excellence by their Certified Pediatric Nurses.
- Patricia Messmer, PhD, RN, CBC, FAAN, was recently honored by the University of Pittsburgh School of Nursing for being a 2005 Distinguished Alumni Awardee. She was recognized at a ceremony along with 2 of her peers. For more information, please visit the University of Pittsburgh website.
- 2005 Nicklaus Children's Hospital Nurse Excellence of the Year Award: Carol Cupido-Hylton, RN - NICU
- 2005 Nursing Leadership Award Winner: Connie Fischman, RN
Department & Unit Awards
- Laura Chechila, RN - 2 East
- Holda Delavoe, RN - PICU
- Anna Diaz, RN - 3 North
- Cathy Donellan, RN - Utilization Quality Management
- Karin Espinosa, RN - PACU
- Cynthia Etter, RN - IV Team
- Roxanna Gomez, RN - After Hours
- Denise Jorge, RN - CV
- Helene Liwanag, RN - Radiology
- Marcina Maraj, RN - 3 South
- Kelli Ann L. McIntosh - 3 NorthEast
- Flor Olivera, RN - Psych.
- Elizabeth Padilla, RN - Float/Staff Relief
- Larry Regalado, RN - Emergency Room
- Kim Ronselli, RN - Operating Room
- Heidi Story, RN - Ambulatory Surgery
- Vanessa Tamariz, RN - 3 East
- Carla Trueba, RN - CVICU
2004 Nursing Awards
2004 Nursing Awards
Nicklaus Children's Nursing Department was featured in an article, "The Magnet Pull", in the April, 2004 issue of Nursing Management. p. 63-66.
Three FNA District V awards were awarded to Nicklaus Children's Hospital nurses at the Florida League for Nursing & FNA District V luncheon on April 17, 2004:
- Jacqueline Gonzalez, ARNP, MSN, CNAA, BC - Nurse Administrator
- Maria Fernandez, ARNP, MSN, CMTE - Advanced Practice
- Natasha Melbourne, ARNP, MSN - Student Liaison
Individual Nurse Awards
- Patricia R. Messmer, PhD, RN, BC, FAAN, nurse researcher, received the American Nurses Credentialing Center (ANCC) Certified Nurse Award at the American Nurses Association (ANA) Convention in Minneapolis, MN on Saturday, June 26, 2004.
- Lisa Juskowitz, RN, CPN, Ambulatory Surgery received "Honorable Mention" Nursing Spectrum of the Year award (one of 5 selected from 48 nurses throughout state of Florida).
- Jeannette Diana, ARNP, MSN, pediatric surgery nurse practitioner, received the "Founder's Award" from the American Pediatric Surgical Nurses' Association (APSNA) 13th Annual Scientific Conference Presentation May 25, 2004, in Ponte Vedra Beach, Florida. The award is presented to a nurse who has made a significant contribution to the care of pediatric surgical patients and provided leadership within the hospital and the community at large.
- 2004 Nicklaus Children's Hospital Nurse Excellence of the Year Award: Blanca Callejas - 3 East
- 2004 Nursing Leadership Award Winner: Suzy Prieto - 3 East
- 2004 Licensed Support Services Award Winner: Karen Niblack, LPN - Emergency Department
Unit Nurse Excellence Award Winners
- Kelly Bronkan - Ambulatory Surgery
- Grisel Cepeda - Utilization Quality Management
- Frances Crawford - 3NE
- Nicole Dixon - 2 East
- Raiza Figueredo - 3 South
- Geraldine Florian - 3 North
- Yulie Giralt - Operating Room
- Susan Golzbein - PACU
- Maytee Gonzalez - 2NE
- Julissa Jimenez - Cardiac Care Unit
- Jennifer McCartney - PICU
- Beverly Newlin - Psychiatry
- Barbie Rivera - Emergency Department
- Nikole Sanchez - Float Pool
- Margot Sarratea - GI Lab
- Sonia Tezini - After Hours
- Sarah Tyner - NICU
2003 Nursing Awards
2003 Nursing Awards
Department Awards
- Communication Media, Florida Nurses Association Award, 2003.
- Promoting Environment for Excellence in Nursing Practice, Florida Nurses Association Award, 2003.
- Promoting Environment for Excellence in Nursing Practice, Florida Nurses Association Award, (Dade County, District V), 2003.
- Caritas Award for Outstanding Contributions to the School of Nursing, Barry University, 2003.
Individual Nurse Awards
- Lisa Juskowitz, RN, Staff Nurse, PACU, Nurse of the Year, Nicklaus Children's Hospital, formerly Miami Children's Hospital, 2003.
- Jackie L. Gonzalez, ARNP, MSN, CNAA received Florida International University (FIU) Pediatric Nursing Initiative Award, March 11, 2003.
- JoAnn Nieves, MSN, ARNP, CPN, APRN-BC was appointed as an item writer to the Certified Pediatric Nurses (NCBNPN) exam.
- Maria Lina (Bing) Wood, Director of PICU, Staffing & ECLS, Cheryl Topps, ARNP, MSN, Nursing Information Specialist, and Jackie L. Gonzalez, ARNP, MSN, CNAA, VP & Chief Nursing Officer, received first place for a poster presentation entitled: Implementation of Scan for Safety Bar-coding Technology, NACHRI (National Association of Children's Hospitals and Related Institutions) Annual Meeting, 2003.
- Jackie L. Gonzalez, ARNP, MSN, CNAA, Vice President and Chief Nursing Officer Inducted into the Nicklaus Children's Hospital Hall of Excellence, 2003.
- Pat Dean, MSN, ARNP, honored by The Epilepsy Foundation of South Florida as an outstanding volunteer, 2003.
- Dottie Thomas, RN, Community Action Award, Florida Nursing Association, 2003.
- Jill Tahmooressi, RN, Nursing Student Liaison Award, Florida Nursing Association, 2003.
Professional Governance
The Professional Governance structure consists of councils at both the Nursing Department Hospital Wide and Patient Care Unit Based levels. The Professional Governance provide nurses at all levels with a forum to actively support and effectively operationalize the Nicklaus Children's Hospital Nursing Philosophy and Standards of Pediatric Practice along with the mission and values of the organization. All councils report to the Nursing Executive Council (NEC) on a quarterly basis, which oversees all aspects of nursing practice; it is chaired by the Nurse Executive SVP/CNO. All clinical nurse chairpersons from the hospital wide councils and unit practice councils (UPCs) report progress and outcomes to NEC.
Quality and Safety Outcomes Council
- The Quality & Safety Outcomes (QSO) Council focuses on improving patient care outcomes and drives quality based strategic goals. Implements structures and processes across the organization in alignment with strategic goals. Ensures that optimal care and outcomes are evidence based standard practices.
Nursing Research and EBP Council
- The Nursing Research and Evidence-Based Practice (NR&EBP) Council is the interprofessional governing body, for which nursing services promotes, supports, facilitates, and conducts nursing research studies and evidence-based practice projects.
- The NR&EBP Council reviews and approves all nursing research proposals and makes recommendations as appropriate; heightens awareness of EBP with annual workshops; and provides consultation to potential researchers on the external IRB process (WIRB) in collaboration with NCH Research Institute department and its standing council members.
Clinical Practice Council
- The Clinical Practice Council enhances nursing expertise by certification, education advancement, etc...; evaluates, develops, and modifies clinical practice related policies and procedures; and collaborates with supply chain in equipment evaluation of products used at the point of care.
Finance Council
- The Finance Council focuses on managing staffing processes, cost savings initiatives, nurse-staffing ratios, and acuity scales for patient care assignments; unit based self-scheduling guidelines to meet the needs of the unit and patients, FMLA and floating guidelines, and any strategic goals that relate to the above.
Exemplary Professional Practice Council
- The Exemplary Professional Practice (EPP) Council evaluates and applies the Nursing Professional Practice Model (PPM), reinforces Magnet standards and a culture of nursing excellence; and participates in community healthcare outreach.
Engagement & Recognition Council
- The Engagement & Recognition (EAR) Council promotes employee engagement through innovative strategies and organizes both internal and external nursing and interprofessional recognition efforts.
Advance Practice Nurse Council
- The Advanced Practice Nurse (APN) Council promotes advanced practice nurse advocacy and the advancement and interdisciplinary collaboration of the nursing profession through scholarly activities.
Nursing Operations Council
- The Nursing Operations Council (NOC) promotes communication between all leadership levels with continued focus on a Magnet culture at the hospital wide level, promotes leadership recognition and involvement, and supports an environment of transparency and advocacy.
Night Shift Council
- The Night Shift Council promotes engagement activities for night shift employees to ensure their voices are heard for initiatives that impact them directly.
Operational Innovations
At Nicklaus Children's Health System, we embrace innovation by deploying state-of-the-art technology throughout the hospital to improve patient safety and the patient experience, as well as to make our operational processes more efficient. Transforming pediatrics through innovation takes a village, and we are proud to work with leading technology companies, community programs, schools, policy-makers and other organizations for the betterment of our patients and their families.
Bar Code Technology
In 2002, Nicklaus Children's became the first pediatric hospital in the nation to introduce medication bar-code technology - the most sophisticated technology available for medication administration control.
Here's how it works:
- Upon inpatient admission, patients receive a bar-code wristband. All medications from the pharmacy also have a specific bar-code.
- Upon receipt of a medication order, the pharmacist reviews the order on the computer. The medication to be given is displayed on the nurse's computer.
- The nurse verifies the order for accuracy and scans the patient's wristband to verify the information.
- The nurse then scans medication to be administered with the bar-code scanner. The computer checks it for accuracy and the nurse then administers the medication after verifying the match.
Electronic Health Record
In 1997, Nicklaus Children's began using a computerized documentation system. We use the computerized system to document the care provided by the healthcare staff in all our patient care areas. The system contains the patient history, flow sheets and progress notes for all disciplines to document their assessments, observations, education, and interventions.
The computerized system is located at the nursing stations and on mobile workstations, workstations on wheels (WOWs), which can be taken to the patient's bedside. Throughout the health system, the system is available to other healthcare providers that have access to view patient information.
On April 17, 2012, Nicklaus Children's Health System successfully transitioned to an electronic health record system that provided significant enhancements for patients and caregivers alike. Internally known as PEDS (Pediatric Electronic Data System), this state-of-the-art program captures all data related to patient care from throughout the multi-facility pediatric healthcare system, including information from radiology, the laboratory, pharmacy, inpatient care, outpatient care, rehabilitation, and urgent and emergency care all in one comprehensive system.
PEDS could not have been developed without the involvement and collaboration of nurses across all levels. Known as subject matter experts, or "SMEs", nurses were selected from units throughout Nicklaus Children's Health System to provide input into the development of the PEDS clinical documentation system. This process took eighteen months to bring Nicklaus Children's Health System to the final "launch" date, and included process mapping, product testing, end-user education, and support during go-live.
EMR Application Suite
The CareAware® suite of applications enables interoperability between medical devices, healthcare applications and the EHR by enabling seamless connectivity among medical devices, nurse call systems, location-based technologies, and other network-connected systems. CareAware® is helping Nicklaus Children's Health System improve operational efficiencies, minimize errors, and reduce costs.
Digital White Board
Cerner's digital unit whiteboard, CareAware® CareView was designed to improve communication and to help eliminate documentation redundancies that often occur when using a handwritten whiteboard.
Capacity Management Bed Tracking and Patient Flow System
The ability to transfer patients from one bed to another seems like a simple task; however, communication barriers between units, transport teams, and environmental services can make this a complex undertaking.
Ultimately, these breaks in processes can extend patient wait times and slow bed turnover. CareAware® Capacity Management helps improve patient throughput by optimizing bed management and automating job assignments for environmental services and patient transportation. Operationally, leaders can view the entire organization's throughput endeavors under this single application.
Smart Phone Communication Platform
CareAware® Connect is a clinical mobility solution designed for smartphones, which helps improve efficiency by completing multiple workflows and coordinating communications using one device. The application allows real-time alerts and notification to be routed to the right user at the right time.
Scheduling and Acuity Systems for Safe Staffing
Clairvia® leverages outcomes, interventions, and observations to create a custom workload calculation based on each patient's clinical condition. By continuously comparing the incoming projected admission, discharge, transfer, and workload demand for patients with existing schedules, managers are able to easily identify any pockets of over or understaffing and proactively adjust staffing needs.
Clairvia® helps Nicklaus Children's Health System appropriately plan for staffing needs and have those needs align to individual patient care coordinating the right patient with the right caregiver at the right time.
More Time at the Bedside
CareAware® VitalsLink®
CareAware® VitalsLink® provides a streamlined, barcode-driven process on an integrated device for clinicians to chart vitals data directly into the EHR at the point of care. Receiving the correct vitals data in a timely manner is critical. The context these data points provide for the diagnosis and treatment during a hospital stay can improve overall patient health outcomes.
CareAware® Seizure Alert
Each room in the Neurology and Neurosurgery Unit is equipped with a seizure alarm. When a patient is having a seizure, the family is instructed to press the seizure alarm to notify the staff. This alarm has a unique ringtone to alert the staff there is a seizure. The alarm sounds throughout the unit and to the nurses CareAware® phones. The Hill-Rom lights flash purple, indicating what room the seizure is occurring.
Hillrom Nurse Call
The Hillrom Nurse Call/Light system is an enhanced clinical application used within the hospital to improve the patient experience and keep patients safe. Not only does Hillrom Nurse Call provide communication between patients and caregivers it also provides secure and reliable communication platform across the hospital.
This system integrates the use of the traditional nurse call system with the addition of easily visible notifications for each patient. With customizable and hospital standard notifications, health care workers can provide quality and safe care by automating the care environment. Nurse Call has been proven to reduce falls with injury by 67%, improve the patient experience score by 30%, and allow the staff to spend more time on direct patient care.
Timeless Medical™ Women and Infants
Timeless manages, tracks & traces the entire preparation & feeding processes at Nicklaus Children's Hospital. It easily integrates with PEDS (our Pediatric Electronic Data System) to provide real-time updates, which saves time and reduces errors. The system also tracks the patient's breastmilk inventory and provides automatic text message notifications in both English and Spanish to mothers when more breastmilk is needed.
Nursing Opportunities
Seeking an opportunity in pediatric nursing? Look no further.
Some of the best nursing jobs in South Florida are right here at
Nicklaus Children's Hospital.
Where else can you tap into one of the finest benefit packages in the region while reaping the personal rewards that come from making a difference in the life of a child? What's more, you'll enjoy the pride that comes with working in one of the best pediatric hospitals in the nation, as ranked by U.S. News & World Report.
Due to Nicklaus Children's Hospital's special focus on children and those who care for them, we try to make life at Nicklaus Children's Hospital fun. Our Red Nose Docs, Children Experience's Department, Radio Lollipop® on-site station, Michael Fux Family Center and volunteer-staffed art and game carts can make all the difference in a child's hospital stay - creating a warm and caring environment that enriches the lives of patients and staff members alike.
Nicklaus Children's is among the most technologically advanced hospitals in the region. Innovations include fully computerized patient records and wireless work stations for fast and efficient charting. We are also the first facility in South Florida and first pediatric facility in the United Sates to introduce bar code technology for medication administration. This demonstrates our commitment to providing the safest, most technologically advanced setting for patient care.
Be part of the team that cares for more than 187,000 children a year. Besides the smiles, giggles and laughter, you'll receive many outstanding benefits. As a Nicklaus Children's Hospital nurse you receive free educational opportunities, the ability to participate in nursing research, evidence-based practice projects and innovation for the sake of the children.
Patient Care Units & Departments
Learn more about our patient care units and departments. Medical nursing divisions at Nicklaus Children's Hospital include:
Ambulatory Units
Ambulatory Units
Dialysis Unit
Nicklaus Children's Hospital Dialysis Unit in collaboration with Children's Hospital Association (CHA), provides specialized modalities for the End Stage Renal Disease (ESRD) pediatric population throughout South Florida. As part of Outpatient Center Services, the Dialysis Unit works closely with other health care facilities for pre and post-transplant work-up and treatment. It has 5 stations equipped to care for 30 patients a week on an outpatient basis.
The unit also provides acute services to adjacent units; PICU, NICU, CICU, and 3NE respectively. The advanced modalities of continuous veno-venous hemodiafiltration (CVVHDF), Peritoneal Dialysis, and Hemodialysis are implemented with specific attention to the individual needs of the patient in acute renal failure. The care team is comprised of highly trained and experienced nephrologists, dietitians, social workers, child life specialists, patient representatives and hospital chaplain who provide 24 hour on-call services 365 days a year.
In addition, the dialysis unit also serves the needs of those end stage renal disease (ESRD) patients receiving Peritoneal Dialysis home therapy. The team educates the patient and family prior to discharge on all facets of peritoneal dialysis specific to care and management in the home environment. Interprofessional daily rounds serve the team to address, plan and discuss dialysis prescription, renal osteodystrophy, anemia, lab adequacy, nutrition, access management, clinical status, medications, social services, and spiritual counseling.
The dialysis unit values research, preventative maintenance and education. Continued ESRD education is provided to nurses working on and in adjacent units to ensure knowledge and hands on skills competency.
Infusion Unit
The Infusion Unit is comprised of 18 beds and infusion chairs. This unit is designed to meet the short-term infusion and transfusion needs of children, adolescents and young adults on an outpatient basis. This specialized unit serves over ten medical specialties for scheduled procedures, transfusions, chemotherapy and other infusion therapies. This outpatient area gives patients access to televisions, games, entertainment and meal options while receiving their medical treatment. Play and age-appropriate activities are integrated into the unit to help keep patients entertained.
Critical Care Units
Critical Care Units
Pediatric Intensive Care Unit
 Nicklaus Children's Hospital's 40-bed Pediatric Intensive Care unit (PICU) has the most sophisticated and extensive pediatric intensive care technology and experience available. The PICU is a multidisciplinary unit that provides high quality care to infants, children and adolescents who become critically ill. Our PICU, located in the new Advanced Pediatric Care Pavilion which spans over six stories and 213,000 square feet provides an enhanced care environment for our patient population. The PICU consistently outperforms national averages in both national outcomes and length of patient stays.
Nicklaus Children's Hospital's 40-bed Pediatric Intensive Care unit (PICU) has the most sophisticated and extensive pediatric intensive care technology and experience available. The PICU is a multidisciplinary unit that provides high quality care to infants, children and adolescents who become critically ill. Our PICU, located in the new Advanced Pediatric Care Pavilion which spans over six stories and 213,000 square feet provides an enhanced care environment for our patient population. The PICU consistently outperforms national averages in both national outcomes and length of patient stays.
The medical staff includes pediatric intensivists, pediatric intensive care fellows, and pediatric residents. The unit maintains a 1:2 nurse/patient ratio to ensure safe, optimal and personal care.
The PICU is home to the state's first and largest pediatric and neonatal Extra Corporeal Membrane Oxygenation (ECMO) resource for children with life-threatening heart and lung conditions. It is also one of three pediatric apheresis blood treatment centers in the state. PICU is proud to hold the prestigious AACN Beacon Gold award.
Neonatal Intensive Care Unit
The 37-bed Neonatal Intensive Care Unit (NICU) provides care for babies who are born early. It includes 30 designated Level III beds and 7 designated level II beds. Our Level III nurse/patient ratio is 1:1 or 1:2 depending on the level of care required by the patient. The Level II nurse/patient ratio is 1:3 or 1:4. The unit is capable of invasive and non-invasive monitoring of the neonate's cardiorespiratory systems and can provide oxygen, suction and age appropriate thermoregulation. In addition, heart rate, respiratory rate, blood pressure and oxygen saturation are monitored continuously.
Pediatric Cardiac Intensive Care Unit
Nicklaus Children's Pediatric Cardiac Intensive Care Unit (CICU) is one of the few pediatric CICUs in the nation. The unit provides highly specialized pre- and post-operative care for children undergoing cardiac surgery and interventional catheterization. The latest equipment and a multidisciplinary team ensure the finest care for pediatric cardiac patients. Innovative therapies available in the pediatric CICU include nitric oxide (an inhaled medication used to relax blood vessels), new inotropic agents, mechanical cardiac assist technology, and a computerized data collection and storage system providing an integrated database for management of patients with complex lesions.
Emergency Department
Emergency Department
Emergency Room
The
Emergency Department (ED) at Nicklaus Children's Hospital provides care for nearly 80,000 children annually and serves as a regional Pediatric Trauma Center. The ED includes a state-of-the-art Triage Center, an outdoor play area for siblings and a raised helipad. The Emergency Department offers one of the shortest emergency room waiting times in country. The department achieves this success through continuous evaluation of services and processes, and a commitment to implementing changes that enhance efficiency and customer satisfaction.
Urgent Care Centers
Nicklaus Children's Urgent Care Centers are strategically located in Miami- Dade, Broward and Palm Beach counties. The centers provide medical care for minor injuries and illnesses. These fast-paced centers are accessible to the community 365 days a year. X-ray services are provided at all Urgent Care Center locations. Ultrasound and MRI services are available at select centers. For information about hours of operation or to schedule diagnostic services, please call 305-663-8413 or toll-free 877-624-8413.
Inpatient Units
Inpatient Units
Pediatric Surgical Unit/Orthopedic (3 North)
This 26-bed surgical/orthopedic unit provides care for children newborn to adolescent who have undergone general pediatric surgery, plastic and reconstructive surgery, urological surgery and orthopedic surgery and treatment. The unit also provides care for general medical and trauma patients. This is an exciting high-paced nursing unit with the opportunity to acquire advanced level nursing skills. The unit is proud to be the recipient of a silver-level Beacon Award for Excellence in patient care from the American Association of Critical-Care Nurses (AACN) for distinguished patient care.
The Department of Psychiatry
The Department of Psychiatry provides inpatient and outpatient services to children and adolescents. The inpatient unit is an acute care, crisis-stabilization unit for children and adolescents between the ages of 4-17 years, with a maximum capacity of 20 beds. As a licensed Baker Act receiving facility, the unit’s structured, safe, therapeutic environment offers an interdisciplinary approach with planned activities and group sessions organized throughout the day.
The Inpatient Psychiatry Unit focuses on diagnostic evaluation, stabilization, discharge and follow-up care. All patients attend daily activities during their stay that include school, group therapies, family therapy, and individual therapy. The interdisciplinary team members include psychiatrists, psychiatry fellows, psychiatry residents, psychologists, psychology interns and students, mental health therapists, nurse practitioners, behavioral health nurses, behavioral health technicians, case coordinators, case managers, and Miami-Dade County Public Schools teacher.
Outpatient Psychiatry services include psychiatric evaluation and medication management with psychiatrists, psychological testing, individual and family therapies, and group therapies. In addition, The Department of Psychiatry offers an Intensive Outpatient Therapy Program that provides an intermediate level of intensive psychotherapeutic services in a least restrictive level of care (12 hours per week) to those adolescents that meet criteria for inclusion.
Neurology and Neurosurgery Services Unit (5 Tower)
This 40-bed unit provides care for patients who have neurological conditions or who have undergone neurosurgery. Within the unit is a 12 bed telemetry unit specifically designed for patients on continuous video electroencephalography monitoring. The unit provides care for children experiencing seizures, neurologic developmental delays, migraines, brain tumors, head trauma, and other general medical patients. Located in the Advanced Pediatric Care Pavilion, 5 Tower utilizes the latest technology for diagnosing and treating epilepsy and other neurological disorders. 5 Tower was awarded the Gold Beacon Award for Excellence from the AACN.
Renal/Gastroenterology/Endocrinology Unit (3 Northeast)
3 Northeast is a 20 bed medical-surgical unit which specializes in the care of children with renal, gastroenterology, endocrinology, adolescent medicine, rheumatology, and other diagnoses 24 hours a day, 7 days a week. The majority of patients served are school age and adolescents. 3 Northeast is recipient of Gold Beacon Award, Improvement Huddle Board Award 2017 and the Team Daisy award. 3 Northeast is committed to providing excellent patient-centered care emphasizing the child's health promotion, health restoration and education, utilizing a holistic approach to nursing care. 3 Northeast is a rewarding unit with the opportunity to acquire advanced level nursing skills such as peritoneal dialysis and insulin pump technology.
Respiratory Unit (3 East)
3 East is a 20 bed medical/surgical unit that specializes in the care of inpatients and observation patients with respiratory illness and other medical diseases including patients on Home Ventilator via a tracheostomy, on BIPAP, CPAP and on High Flow Nasal Cannula support. Care is based on 24 hour a day, 7 days a week. 3E is recipient of Gold Beacon award, Improvement Huddle Board award 2017. 3 East is committed to providing excellent family centered care emphasizing the child’s health promotion, health restoration and education, utilizing a holistic approach to nursing care. It also provides safe, quality and cost-effective care to patients requiring evaluation and treatment for a period of 24-48 hours. 3E is a fast paced nursing unit with the opportunity to develop advanced skills level nurses and foster critical thinking.
Hematology/ Oncology and Bone Marrow Transplant (BMT) Unit (6 Tower)
This unit is located on the 6th floor of the Advanced Pediatric Care Pavilion with 35 inpatient beds, seven of which comprise the Blood and Bone Marrow Transplant (BMT) unit. The inpatient hematology oncology unit specializes in the care of patients with hematology diseases such as: sickle cell anemia, bleeding disorders and other alterations in the hematopoietic system. Additionally, patients with oncology diseases are admitted for chemotherapy treatments, biotherapy treatments, toxicities such as febrile neutropenia, and supportive care. The seven bed BMT unit treats a variety of malignant and non-malignant disorders with autologous hematopoietic stem cell transplants, allogeneic related hematopoietic stem cell transplants, allogeneic unrelated hematopoietic stem cell transplants and related and unrelated cord blood stem cell transplants.
Infant Care Unit / Observation Unit (2 North)
The Infant Care Unit/Observation Unit (2 North) at Nicklaus Children's Hospital is a 14-bed unit; eight of these rooms are designated to receive infants (<1 y/o) with medical/surgical care needs and the other six beds are designated to admit children/adolescents (0-21 y/o) that meet criteria for observation status. In June 2018, 2 North was awarded the Silver Beacon Award for Excellence recognized by the American Association of Critical-Care Nurses. This national three-year designation marks a significant milestone on the path to exceptional patient care and achieving a healthy work environment.
The five most common diagnoses admitted to the Infant Care Unit are as follows: acute bronchiolitis due to Respiratory Syncytial Virus (RSV), Gastroesophageal Reflux Disease without Esophagitis, Urinary Tract Infection, Congenital Hydronephrosis, and Salmonella Enteritis. The Infant Care Unit provides opportunities for infant specialized care such as phototherapy for the treatment of hyperbilirubinemia and high flow nasal cannula (HFNC) for the treatment of bronchiolitis.
The Observation Unit is dedicated to patients who require additional monitoring. A stay in the Observation Unit is an alternative to a hospital admission. A typical stay lasts between 4 hours and 23 hours. Our goal is to provide excellent care in order to send the child home as soon as possible. The Observation Unit admits patients under general pediatrics and/or pediatric surgery.
LifeFlight® Critical Care Transport Program
LifeFlight® Critical Care Transport Program
Nicklaus Children's Hospital LifeFlight® critical care transport team provides transport of critically ill children from referring hospitals to Nicklaus Children's Hospital pediatric care units. In addition to ground ambulance transports, the LifeFlight® program offers air transport via helicopters operated by PHI, Inc., one of the world’s most experienced aircraft operators and the holder of a Part 135 Certificate issued by the Federal Aviation Administration, and through contracted fixed-wing aircraft charters.*
Staffing is provided by a team of an RN, Paramedic and EMT and Communication Specialist. If needed, a physician will accompany the LifeFlight® medical crew members. Drivers are EMT's or paramedics and have been trained in the safe operation of emergency vehicles and equipment. LifeFlight® provides a specialty neonatal/pediatric team of an RN and Paramedic on all transports. Quality patient care is assured during transport because LifeFlight's medical crew members are recognized for their high standards of professional excellence. They have advanced neonatal/pediatric cardiac and critical care experience. Each RN and Paramedic is certified in PALS (Pediatric advanced Life Support, ACLS (Advanced Cardiac Life support) and NRP (Neonatal Resuscitation Program) and has specialized Department of Transportation flight training and safety. These programs include survival training, skill labs as well as intubation training. EMT's and Paramedics have been trained in the safe operation emergency vehicles and equipment.
* Nicklaus Children's Hospital is not a direct air carrier. Aircraft, both helicopter and fixed wing, are operated pursuant to contract with Nicklaus Children's Hospital, by companies which are FAA certificated.
Radiology Department
Radiology Department
The Department of Radiology at Nicklaus Children's Hospital is an exclusive pediatric radiology facility. We have been imaging children since 1950; constantly providing state-of-the art equipment and staff that is trained and dedicated to the care of infants and children. The department is staffed by highly trained specialists, including Radiologists, Radiology Nurses, Techs and support staff. These experts work together with clinical sub-specialists and attending physicians to support the care of children.
The department's commitment to excellence has led to its establishment as a regional leader for pediatric radiology, serving children throughout Florida as well as the Caribbean, Central America and South America.
The Nicklaus Children's Hospital Radiology Department is proud to be accredited by the American College of Radiology (ACR) for Magnetic Resonance Imaging (MRI), Ultrasound (US), Nuclear Medicine, PET and Computed Tomography (CT) services. Compliance with all requirements and receipt of accreditation is an outstanding achievement and speaks well of the dedication, skill and determination of the Radiology Department.
Surgical Services
Surgical Services
Same Day Surgery Unit
Same Day Surgery is comprised of an 8 bed preoperative unit and 8 bed Phase II Post-Anesthesia Care Unit (PACU II). Average monthly case volume is approximately 450, with the age of patients ranging from newborns to 21 years. The unit provides preoperative screening and care to both inpatient and outpatient patient populations for the following surgical specialties: general, ophthalmology, ENT, orthopedics, plastic and reconstructive, neurosurgery, cardiovascular, and urology. The PACU II phase provides post-operative nursing care for patients being discharged on the day of surgery.
Cardiac Catheterization Lab
The Cardiac Catheterization Lab (CCL) serves both the inpatient and outpatient population by providing care for children and adults who were previously served by the hospital for congenital heart disease or who are referred for a specialized procedure for congenital heart disease with congenital or acquired heart disease. The CCL includes two interventional suites, 1 Cath lab and 1 Hybrid Suite specializing in the following interventional services: Cardiology, Electrophysiology and Neurology.
Operating Room
The Operating Room Department includes 9 ORs, one OR is a hybrid iMRI suite. Also in the department are 1 Cardiac Cath Suite and a Hybrid interventional radiology/Cardiac Cath/Surgical suite. For total of 11 rooms.
The OR annually provides care for thousands of children, from newborn to 21 years of age. We are a Level 1 Pediatric Trauma Center. We are staffed 24/7, ready for any emergency. Staff members include approximately 65 nurses, scrub techs, peri-operative aides, and anesthesia techs.
In addition to the core OR staff, we have interdisciplinary teams from Anesthesiology, Radiology and Neuro-Physiology.
Surgical Specialties include:
Post Anesthesia Care Unit (PACU)
The PACU I unit is a critical care area that specializes in recovery of perioperative patients in the immediate post-anesthesia phase. The unit is comprised of 12 PACU bays with one isolation room. Nurses in the PACU I phase care for both inpatient and outpatient patient populations, ranging from newborns to adult with oversight by an attending anesthesiologist. Specialties served by the PACU include ENT, ophthalmology, orthopedics, general, plastic and reconstructive, neurosurgery, urology, interventional radiology, and cardiac catheterization lab.
Minor Procedure Suite
The Minor Procedure Suite (MPS) serves both inpatient and outpatient population ranging from infancy through 21 years. The department supports services to include Dermatology, Gastroenterology, ENT, Hematology/Oncology, and Dental procedures, with an average volume of 300 cases per month. The following procedures are also performed by the MPS department: pH probe study, hydrogen breath test, esophageal and biofeedback manometry, and body composition analysis.
Philosophy of Care
The philosophy of the Nursing Department upholds the same core principles of patient and family centered care:
“The delivery of nursing care is guided by comfort care principles and family centered care. The nursing department believes that each patient is a unique and integral part of the family unit. The delivery of patient care ensures respect for the dignity, values, religious and cultural needs of our children and families.”
All aspects of nursing care at Nicklaus Children's Hospital revolve around the concept of incorporating the parent and child’s needs into the care of the child. Nicklaus Children's Hospital recognizes that supporting the needs of patient, family and caregivers facilitates their involvement in the planning and delivery of care. One example of supporting the needs of the family is the construction of the Michael Fux Family Center (MFFC), a family friendly campus enhancement at Nicklaus Children's Hospital. This beautiful and welcoming facility, which opened in October 2009, is designed for the comfort and care of families as they transition through the difficulties of caring for a sick child. To ensure that the patient and his or her support system is involved in the planning and delivery of care, the MFC has access to computers for family use which link to the patient and family educational “Get Well Network”. Families with children in the ICUs which do not have bedside access to the network can access it there. The Micheal Fux Center has various other family friendly amenities from basic comforts, such as showers and laundry facilities, to stress relievers including a workout gym, massage room, family entertainment facilities and a movie theater.
The Nursing Department has adopted Dr. Katharine Kolcaba’s Comfort Theory as its conceptual framework and foundation for the Nursing Professional Practice Model (PPM). The Comfort Theory is embedded throughout the PPM reinforcing the framework for nursing practice is continuously supporting an environment and culture of comfort.
The Nursing mission statement to “provide compassion and comfort through innovative advanced care for our children and families” and vision “we will be where the children are, providing comfort through exceptional nursing care” demonstrate the Nursing Department’s commitment to the Comfort Theory as the conceptual framework for the Nursing PPM.
Collaboration within the Continuum
Collaboration is a core element to care delivery and is incorporated into all components of Nursing within the organization. The nursing department believes in interprofessional collaboration within the continuum of care, emphasizing the patient and the family as the central element in the process. Collaboration across other healthcare professionals with similar purposes, such as, child health advocates, organizations at the local, regional, state, national, and international levels. Advancing the art and science of pediatric nursing, occurs through interactive efforts among all nurses in clinical practice, education, research, and administrative.
Quality and Continuous Improvement
The focus on patient quality and outcome measurements of continuous improvement is integrated into nursing practice and in the foundation for improving patient outcomes. It is a core concept where creativity, perseverance and participation are paramount. The nursing department establishes position statements and standards of practice in alignment with the American Nurses Association (ANA) and Society of Pediatric Nurses (SPN). Assuring safety is principal in the delivery of quality patient care. We encourage creativity, team work, and patient advocacy in achieving optimal outcomes for each individual and family. Our scope of practice extends beyond the walls of the institution into the community, through Nicklaus Children's Hospital's commitment to the promotion of health and wellness.
Child and Family Advocacy
Each nurse is an advocate for the child and family, and promotes the utilization of resources for the individual needs of the child and their family. In addition, nurses advocate accessible, affordable, comprehensive healthcare services for children and their families.
Preserving Dignity
Preserving the dignity and privacy of children and families is the focus of Family-Centered Care. Respect is an integral component of care delivery.
Embracing Diversity
The nursing staff honors and respects patients and families they serve as well as their colleagues. Patients and families come from all over the world to receive care in a Family-Centered Care environment. Excellent care is provided, honoring cultural beliefs, values, religious beliefs and diverse backgrounds.
Professional Growth
Professional growth is encouraged and integrated into all aspects of nursing practice including participation in professional organizations, encouraging education, certification, research utilization and evidence-based practice. The culture at Nicklaus Children's Hospital embraces professionalism, collaboration and accountability. The organization believes that a clinical learning environment for students and staff is conducive to the continuing development and practice of excellence in patient care.
The goal of excellence is at the core of nursing at Nicklaus Children's Hospital. Each person is encouraged to achieve their best, as a personal commitment, as well as a commitment to the children and the families who come to Nicklaus Children's Hospital for care.
References:
Statement on the Scope and Standards of Pediatric Nursing Practice. Society of Pediatric Nurses. 2003.
Society of Pediatric Nursesand American Nurses Association. Family-Centered Care: Putting It Into Action 2003.
American Nurses Association (ANA). Nursing Administration: Scope and Standard of Practice. January 2003.
http://www.pedsnurses.org. Nov. 2002.
Hallstrom, I. Dr. med sci, RN, RSCN, Runesson, I., RN, RSCN and Elander, G. Dr. med sci, RN, RSCN. (2002). Observed Parental Needs During Their Child's Hospitalization. Journal of Pediatric Nursing, Vol. 17, No. 2, April. pp. 140-148.
Ahmann, E. & Johnson, BH. (2001). Family matters: New guidance materials promote family-centered change in health care institutions. Pediatric Nursing, 27 (2), 173-175.
Ahmann, E. & Johnson, BH. (2000). Family matters: Family-centered care: Facing the new millennium. Pediatric Nursing, 26 (1), 87-90.
American Nurses Association. Scope and Standards of Practice for Nursing Professional Development 2000.
Gordin, P. & Johnson, BH. (1999). Technology and family-centered perinatal care: conflict or synergy? JOGNN - Journal of Obstetric, Gynecologic, Neonatal Nursing, 28 (4), 401-8.
Professional Development
The Nursing Philosophy at Nicklaus Children's Hospital states:
Professional growth is encouraged and integrated into all aspects of nursing practice including participation in professional organizations, encouraging education, certification, research utilization and evidence-based practice.”
The Staff and Community Education Department is responsible for continuing the talent development process supporting Nicklaus Children's Hospital's operating statement: “a network of comprehensive care centers with talented people dedicated to exceeding the expectations…”. The Staff and Community Education Department is also responsible for the implementation of continuing nursing education programs. Training Magazine's annual listing of the top 125 training organizations in the country recognized Nicklaus Children's Hospital in their "Training Top 125" list for organizations that excel at employee learning and development.
At Nicklaus Children’s Hospital, we believe that investing in professional development enhances nursing satisfaction and patient outcomes. Nurses are provided numerous opportunities to advance their knowledge and skills. Some of our educational programs include:
- Nursing Grand Rounds are held monthly and highlight current research and practice topics and feature expert speakers.
- The Preceptor Development Course is a full day event that provides prospective preceptors with a foundation for stepping into the role of developing nurses new to the organization.
- The End of Life Nursing Education Conference provides health care providers with the knowledge to care for palliative care patients.
- Raising the Bar is our Annual Pediatric Nursing Conference that features current themes, research, and evidence-based practice topics.
- Annual Simulation Labs and Nursing Skills Fair
- Specialty-based classes which support advanced knowledge in leading areas including Oncology, Congenital Heart Disease Curriculum, Emergency Nursing and Trauma training, Extracorporeal Life Support, Dialysis, and Diabetes education.
The Aim for Professional and Educational Excellence (APEX) is the nursing professional ladder that provides staff nurses across all settings with a professional development and monetary incentive to go above and beyond in their practice, education, and professionalism. Nurses are given points in a variety of categories to promote nursing professionalism including: education, professionalism, clinical skills, experience, certification, special projects and councils. These points are accumulated during the nurse’s annual evaluation as one of the components on performance appraisal and merit increases. Nurses have an entire year to participate in several opportunities to accumulate APEX points and strive for advancing to a higher level.
Nursing Publications
The Nursing Department at Nicklaus Children's Hospital supports, engages and empowers nurses to initiate Evidence Based Practice (EBP) process improvements and nursing research throughout the organization. Nurses across all levels are continuously encouraged to explore the most current and best practices and generate new knowledge when an identified need arises. Integration of evidence based best practices and nursing research into clinical and operational processes aligns to the Nursing Department’s commitment to provide the high quality care associated with positive patient outcomes.
Professional Practice Model
NOTE: Please hover over and select the desired topic on the star below to visit each section.
Nursing Annual Report
2022 Nursing Annual Report

2020-2021 Nursing Annual Report

2018-2019 Nursing Annual Report
2016-2017 Nursing Annual Report
2014-2015 Nursing Annual Report
2012-2013 Nursing Annual Report
Medical Library
The services of the Medical Library at Nicklaus Children's Hospital are designed to promote quality health care and continued medical education through the provision of knowledge-based resources; in print and electronic formats as well as audiovisual materials. In addition to providing services to the medical and hospital staff, residents and students, the Medical Library serves as a resource center for the educational and research programs of Nicklaus Children's Hospital. In order to receive the services offered by the Nicklaus Children's Hospital Medical Library, all patrons must be registered, and be a part of the Nicklaus Children's Hospital staff.
Medline Searches
Interlibrary Loans
Through our Interlibrary Loan program, patrons looking for articles not available at Nicklaus Children's Hospital are able to borrow or order from a network of 85 libraries. The Library staff will make every effort to locate material needed. Fees will be assessed on those articles obtained from out-of-town libraries.
We encourage you to e-mail your request. Turnaround time for this service is five working days; however, Patient Care Emergency Requests can be filled within 24 hours. Please let us know if material is needed immediately.
Codes for 24-hour Library Access
The Medical Library is available after hours and on weekends through badge access. During this time patrons can use the copier and computer terminals. No materials can be removed while unattended, since the Library is under strict security surveillance at all times. Failure to follow these guidelines will set off the alarm. A report must then be filed with security.
Access to Ovid Medline
The computers located in the medical library at Nicklaus Children's Hospital provide around the clock access to the Ovid Medline system, allowing patrons to run searches on Medline as well as other databases. Presently, there are hundreds of full-text journal titles available online. Users outside Nicklaus Children's Hospital may request an individual password for remote access to this system.
Other Resources
The Medical Library at Nicklaus Children's Hospital also provides information from other websites such as the American Academy of Pediatrics, and access to applications such as the Advisory Board, UptoDate and RefWorks.
About the Staff
The Medical Library falls under the Senior Director of Clinical Affairs, Elizabeth Menocal, who is on duty from 8:00 a.m. to 4:30 p.m., Monday through Friday. There are also two support staff on duty from 8:00 a.m. to 5:00 p.m., Monday through Friday.
Physician Portal
The Nicklaus Children's Hospital Physician Portal allows authorized hospital physicians access to their patients records via the Internet. If you are an Nicklaus Children's Hospital physician and do not already have access to the Physician Portal, please call (305) 666-6511 to request access and training information.
Please follow the checklist below for your PC setup before using the Physician Portal for the first time:
| System Requirement |
Checklist |
- Workstation (IBM Compatible
- Microsoft Windows
(Microsoft Windows 2000 Professional or Microsoft Windows XP Professional)
- 1 GHz Processor, 256 MB RAM
- Microsoft Internet Explore 6.0 or Higher
- Internet Access (Broadband Connections such as Satellite, DSL, or Cable Modem
- Java 5.0 for Windows
|
-
Set your screen resolution to 1024 x 768 (or higher)
-
Install Adobe Acrobat Reader (see link below)
-
Install Sun Microsystems Java plug-in (see link below)
-
High-speed Internet access (Cable / DSL) works best
|
|
Click the button below to download the free
Adobe Acrobat Reader program

|
Click the link below to download the free
Java plug-in for viewing Medical Records Deficiencies. Choose the option to Open when the download starts.
Java Plug-in for Deficiencies
|
Health Outcomes, Policy and Economics Center
Welcome to the Health Outcomes, Policy and Economics Center (HOPE), part of the
Radiology Department. This page was developed to provide you with useful information about the kind of outcomes, policy and economics studies we perform, our specific services, scientific staff and current projects.
Goal
The HOPE Center's goal is to perform robust studies in technologies assessment, health outcomes, quality of life, evidence-based clinical guidelines, cost-effectiveness analysis, quality improvement systems and error prevention programs which will benefit patient care in developed and developing countries.
On-going Projects
Quality Improvement and Error Prevention Systems
- Sedation and contrast reaction computerized simulator.
- Prospective trials of training programs in sedation and contrast reactions.
Evidence-Based Clinical Guidelines
- Clinical and imaging predictors of surgical disorders in children with macrocrania.
- Clinical predictors of surgical intracranial space occupying lesion in children with headache.
Decision Analysis and Cost Effectiveness Studies
- The role and cost-effectiveness of imaging in children with headache suspected of having an intracranial space-occupying lesion.
- The role and cost-effectiveness of imaging in newborns with suspected occult spinal dysraphism.
- The role and cost-effectiveness of imaging in newborns with suspected craniosynostosis.
New Imaging Technology and Techniques
- Advance three-dimensional reconstructions in craniosynostosis and complex calvarial fractures.
- MR cholangiography and pancreatography.
- CT angiography in the evaluation of extremity vascular trauma.
- Functional MRI in children with learning disorders and seizures.
Imaging Protocol Optimization
- Intracranial space-occupying lesions and brain tumors.
- Occult spinal dysraphism in children.
Scientific Focus
Technology Assessment
The HOPE Center conducts diagnostic performance studies to determine the sensitivity, specificity and receiver operating characteristic (ROC) curves of emerging technologies. Intra and interobserver variability of new diagnostic and therapeutic test are also evaluated.
Decision Analysis Studies
Decision Analysis studies are those structured to assess a specific clinical question or problem over time, by creating a decision tree that illustrates sequential choice points for action and for information gathering, and when specific outcomes occur. The flow of the decision tree information is based on the available literature. Decision Analysis studies determine the best choice of diagnostic tests or treatments for specific diseases.
Error Prevention and Quality Improvement System
Medical error is one of the seven leading causes of death in the United States of America. The HOPE Center emphasizes the use of computerized simulators and education as important tools in the prevention of medical error and the improvement of our patient's quality of care.
Cost-Effectiveness Analysis
Cost-effectiveness analysis (CEA) provides information so society can prioritize the use of our limited healthcare resources. Ideally, CEA should be done from a societal prospective with long-term outcomes such as life years saved, or quality-adjusted life years saved. These long-term CEA outcomes allow comparison of different health care diagnostic studies and interventions.
Evidence-based Medicine and Imaging
The physicians and the medical staff should base medical decisions and actions on the best scientific evidence available. The HOPE Center performs extensive literature review, operational and research studies to provide our patients with the most updated medical information. Guidelines and decision trees are developed to optimize the diagnostic and therapeutic strategies for our patients.
Staff
- L. Santiago Medina, M.D., M.P.H. - HOPE Center Director
- Nolan R. Altman, M.D. - Director and Radiologist-in-Chief
- David Zurakowski, Ph.D. - Statistician, Harvard Medical School
Publications
The following is a list of the staff's related publications.
Medina LS, Study Design and Analysis in Neuroradiology. A Practical Approach. American Journal of Neuroradiology. 1999; 20:1584-1596
Medina L. S., Frawley K., Zurakowski D., Buttros D., DeGrauw A.J.C., Crone K.R. Children with Macrocrania: Clinical and Imaging Predictors of Surgical Disorder. American Journal of Neuroradiology. In Press.
Medina L. S. Three-Dimensional CT Maximum Intensity Projections of the Calvaria: A New Approach for Diagnosis of Craniosynostosis and Fractures. American Journal of Neuroradiology. 2000; 21:1951-1954.
Medina L. S., Kuntz K.M., Pomeroy S. Children with Headache Suspected of Having a Brain Tumor: A Cost-Effectiveness Analysis of Diagnostic Strategies. Pediatrics 2001. 108:255-263
Medina L. S., Crone K., Kuntz K.M. Newborns with Suspected Occult Spinal Dysraphism: A Cost-Effectiveness Analysis of Diagnostic Strategies. Pediatrics 2001. 108.
Medina L. S., Altman N.A., Establishing a Health Outcomes and Economics Center in Radiology: Strategies and Resources Required. Pediatric Radiology. In Press.
Medina L. S., Aguirre E., Altman N.A. Cost Analysis of Vesicoureteral Reflux in Children by Using Time and Motion Analyses. Submitted to American Journal of Roentgenology (AJR).
Medina L. S. Changes in Brain Water Diffusion Durango the First Year of Life: Finally Starting to Understand the Age-and-Brain Tissue Related Normative Data. Radiology. 2002. 222:316-318
Jayakar P., Bernal B., Medina L. S., Altman M.A. False Lateralization of Language Cortex on Functional MRI After a Cluster of Focal Seizures. Neurology. In Press.
Physician Forms
Below please find below the most frequently requested forms.
Online Forms
PDF Forms
Consent for Release of Information
Physician Forms
Below please find below the most frequently requested forms.
Online Forms
PDF Forms
Consent for Release of Information
Weekly Updates in Pediatrics Newsletter
The Updates in Pediatrics weekly newsletter provides concise information about a broad range of current pediatric topics to enhance the education of practicing primary care pediatricians. The scope includes translational research, infectious disease, neonatology, surgery and other relevant topics concerning the health of children.
 About the Editor
About the Editor
Jack Wolfsdorf, MD, FAAP
Editor-in-Chief, Updates in Pediatrics, formerly International Pediatrics, Nicklaus Children’s Hospital, 2004-present.
Director of Critical Care Medicine, Nicklaus Children’s Hospital, Clinical Professor of Pediatrics, (1984-2004).
Published over 120 articles.
Updates in Pediatrics Yearly Archives
December 2022
November 2022
October 2022
September 2022
August 2022
July 2022
June 2022
May 2022
April 2022
March 2022
February 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
November 2020
October 2020
September 2020
August 2020
July 2020
June 2020
May 2020
April 2020
March 2020
February 2020
January 2020
December 2019
November 2019
October 2019
September 2019
August 2019
July 2019
June 2019
May 2019
April 2019
March 2019
February 2019
January 2019
Editor's Picks for 2018
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
May 2014
April 2014
March 2014
February 2014
January 2014
December 2013
November 2013
October 2013
September 2013
August 2013
July 2013
June 2013
May 2013
April 2013
March 2013
February 2013
January 2013
December 2012
November 2012
October 2012
September 2012
August 2012
July 2012
June 2012
Human Subjects Protection Program
 The two primary organizational components of the Human Research Protection Program at Nicklaus Children's Research Institute, and Institutional Review Board (IRB). All research involving human subjects conducted at Nicklaus Children's Hospital must have approval from IRB. In collaboration with IRB, the Nicklaus Children's Research Institute also assumes certain administrative responsibilities for the Human Research Protection Program at Nicklaus Children's Hospital.
The two primary organizational components of the Human Research Protection Program at Nicklaus Children's Research Institute, and Institutional Review Board (IRB). All research involving human subjects conducted at Nicklaus Children's Hospital must have approval from IRB. In collaboration with IRB, the Nicklaus Children's Research Institute also assumes certain administrative responsibilities for the Human Research Protection Program at Nicklaus Children's Hospital.
Nicklaus Children's Research Institute ensures research participant protection by establishing formal processes to evaluate and continually improve the protection of human research participants, dedicating sufficient resources through exercising oversight of research protection, providing education and training opportunities to investigators and research staff, and, when appropriate, by providing a mechanism to intervene in research and to respond directly to concerns of research participants.
Within Nicklaus Children's Research Institute , the Human Research Protection Program is guided by policies and procedures that specify the roles and responsibilities of research staff in preserving and protecting the safety, rights and well-being of prospective and active research participants in all phases of study from planning through recruitment and conduct of the protocol to conclusion of the study and disclosure or publication of research results.
Search for Open Studies
You can also search for current studies Nicklaus Children's Hospital is participating in ClinicalTrials.gov
Search for Open Studies
You can also search for current studies Nicklaus Children's Hospital is participating in ClinicalTrials.gov
Links and Resources
GME Committee (GMEC)
Scholarly Activity
The Annual Nicklaus Children’s Hospital Scholarship Day
The Nicklaus Children's Hospital Scholarship Day is a yearly event that features the scholarly activities of our pediatric residents, dental residents, pediatric subspecialty fellows, and nursing colleagues. The event is organized by the Nicklaus Children’s Research Institute and the Departments of Medical Education and Nursing. Research projects (original research and case reports) and QI projects are submitted, peer-reviewed, rated, and displayed as poster presentations. Winning abstracts are presented as podium presentations.
Scholarship Day 2020 was canceled due to COVID restrictions. Our 2021 event has been rescheduled as a virtual activity.
Scholarship Week 2021 Activity Schedule
We are pleased to announce the 12th Annual Scholarship Event! This event was postponed for 2020 due to the pandemic but we are happy to bring it back this year in a virtual format. The participating abstracts will be showcased via zoom, starting Tuesday, June 1, 2021 and ending Friday, June 4, 2021, over the course of 6 Sessions.
The sessions are theme/specialty-based. A list of all the available sessions, with zoom meeting information, is available below. Additionally, you can click the following links to download a list of the Abstracts Sorted by Specialty, download a Detailed List of Abstracts, or download the “Schedule at a Glance”.
The winning abstracts will be showcased during the Friday, June 4 Pediatric Grand Rounds session (details below).
Please join us and support our trainees and nurses! Also feel free to or mention this event on social media using the tag #NicklausScholars2021.
Click each tab below to expand and view the meeting details.
Clinical Competency Committees (CCC)
Nicklaus Children's Hospital Department of Medical Education and its training programs are committed to conduct meaningful assessments of their trainees based on multiple sources including formative and summative evaluations, milestones-based assessments based on direct observation, simulation, rating scale, evaluation of scholarly work, and 360 degrees evaluation in compliance with the ACGME requirements. These assessments are meant to provide meaningful performance evaluation and feedback to allow to the program director to design an individualized learning plan aimed at strengthening areas of weakness.
In accordance with the ACGME requirements, each training program is expected to form a Clinical Competency Committee (CCC). The program director appoints the CCC. The CCC must have at least three program core faculty (excluding the program director) who have the opportunity to observe and evaluate the residents. CCC members may also include non-physician members of the health care team, non-MD educators, assessment specialists, or residents in their final year. For example, a small fellowship program may include faculty from the core program or from required rotations in other specialties.
Description of CCC meetings:
- The CCC meets at least semi-annually to review and discuss each individual residents’ performance data (one year programs might need to meet more frequently to give meaningful assessments but they have less number of trainees)
- The program director (PD) and the GME department will prepare Milestones data summary on each resident through reports generated from various sources e.g. 360-degree evaluations, rotation evaluations, Simulations, etc…
- In some situations the residents’ data will be divided among CCC members to review before the meeting and report on during the meeting
- The role of the CCC is to make a consensus decision on the progress of each resident by applying assessment data to the milestones.
- The CCC serves as an early warning system/early identification if a resident fails to progress in the educational program and make recommendations to the program director for resident progress including promotion, remediation, and dismissal.
- Each resident is given a semi-annual assessment on a dashboard in one of the following 5 categories on each of the metrics set by the program: (No Data, Below Expected for training level, Needs Improvement, On Track for training level, Above Expected for training level).
- The CCC will generate a report/ recommendation letter to PD on each resident. The PD will meet with each resident and communicate the recommendation, design an improvement plan, etc..
- Thresholds will be set by the CCC. Interventions a program might consider include assigning a mentor with expertise in a given area of deficiency, additional required readings, sessions in a skills lab, and/or added rotations in a given area. If, after remediation, a resident still fails to advance sufficiently on one or more milestones, a CCC might consider extending education, or counseling the resident to consider another specialty or profession.
- While the PD is part of the CCC meeting, the PD must not chair the meeting and can be available for clarification, etc..
- The program director has final responsibility for the program and trainees’ evaluation and promotion.
- The program director reports the aggregate, de-identified information for all residents in the program to the ACGME in the ADS system.
To view the members of the CCCs, please go to individual programs' website.
View the Roles and Responsibilities of the CCC
Quality Improvement
Tractography Studies
Beyond the basic division of efferent and afferent fiber tracts, there is a more intricate architecture of the cerebral white matter. In addition ot the long tracts that connect the brain ot the rest of the body, there is a complicated 3D network formed by short connections among different cortical and subcortical regions. The existence of these bundles has been revealed by histochemistry and biological techniques on post-mortem specimens. Brain tracts are not identifiable by direct exam, CT or MRI scans. This difficulty explains the paucity of their description in neuroanatomy atlases and the poor understanding of their functions.
Tractography is a procedure to demonstrate the neural tracts. It utilizes special techniques of magnetic resonance imaging (MRI), and computer post-processing. The results are presented in two and 3D images.
The MRI sequences utilized look at the symmetry of brain water diffusion. Bundles of fiber tracts make the water diffuse asymmetrically in a tensor, the major axis parallel to the direction of the fibers. The asymmetry here is called anistropy. There is a direct relationship between the number of fibers and the degree of anistropy.
Research and studies conducted by: Dr. Nolan Altman and Dr. Byron Bernal of the Radiology Department
3D Images of Cerebral Tracts
Acknowledgment
The following images consist of a comparison of brain dissections and 3D images obtained by post-processing DTI fiber tracking. The postmortem brain dissections images are obtained with permission from Dr. Terence H. Williams, MD, PhD. They were downloaded from University of Iowa.
Until now there has never been an exam to demonstrate the superior longitudinal fasciculus. Postmortem dissections are limited to the gross anatomical structure.
Once a given structure can be isolated with imaging, it can be displayed three-dimentionally. Brain fasciculi (tracts) are complex, in that they are oriented in multiple planes. The understanding of the anatomy of these tracts is greatly facilitated with 3D display.
This is accomplished by computer processing of DTI sequences, and corregistered anatomical images. The 3D relation of the tracts within another larger 3D structure (brain) is performed by displaying the tract in an orthogonal view along with a 3D static view at an angle suited to the course of the tract of interest.
Classification of Neural Tracts
Projection Fibers
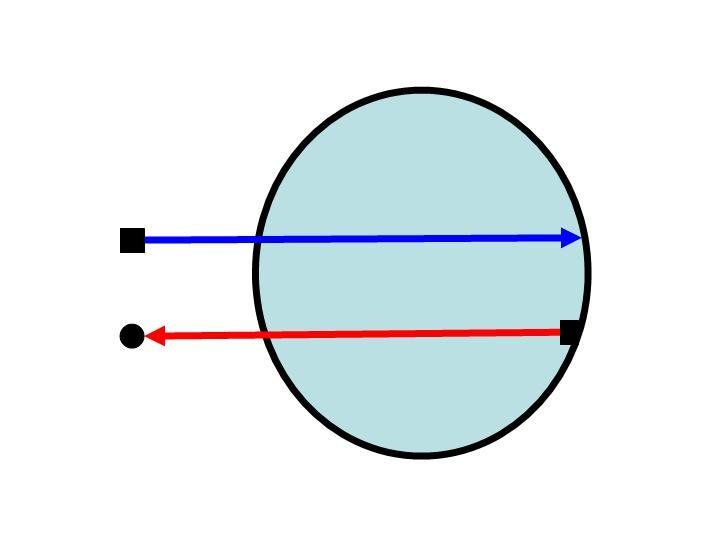 Notice the relationship between these arrows and the wall of the circle. The arrow origin or head may be located at the perimeter of the circle, or outside of the circle. If we replace the arrows for tracks and the circle for the brain (the perimeter the cerebral cortex) we will understand the tracts called "Projection Fibers." They carry information in and out of the brain. Some examples of "Projection Fibers" are: Visual Pathways, and the Cortico-spinal or pyramidal tract.
Notice the relationship between these arrows and the wall of the circle. The arrow origin or head may be located at the perimeter of the circle, or outside of the circle. If we replace the arrows for tracks and the circle for the brain (the perimeter the cerebral cortex) we will understand the tracts called "Projection Fibers." They carry information in and out of the brain. Some examples of "Projection Fibers" are: Visual Pathways, and the Cortico-spinal or pyramidal tract.
Projection Fibers Types
- Efferent (Going away)
- Cortico-spinal tract (Pyramidal tract)
- Cortico-nuclear system
- Fronto-pontine tract
- Afferent (Coming towards)
- Spino-thalamo-cortical tract
- Visual pathway
- Auditory pathway
- Medial Lemniscus system
Associative Fibers
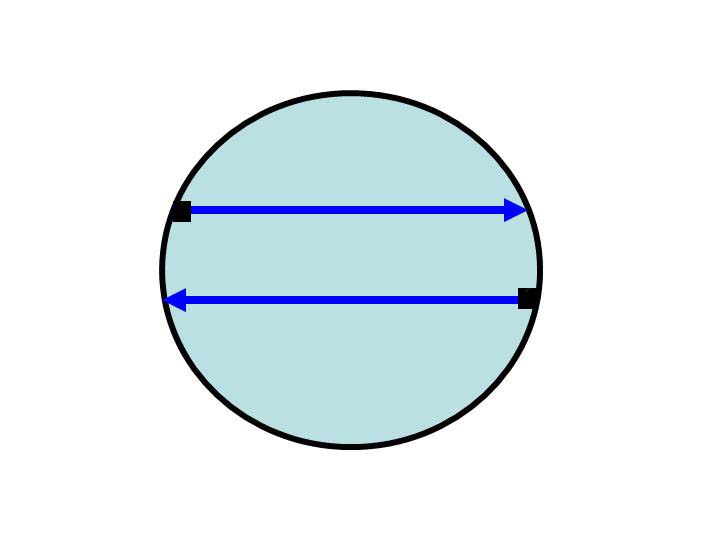
In this other example the arrows have both origin and end point within the circle "connecting" different points of the perimeter. Using the same model, this represents fibers that connect different areas of the cerebral cortex, within the same hemisphere or between them. These types of fibers are called "Associative Fibers." They carry information between similar areas of processing, or from lower to higher levels of cortical complexity. Two examples of these fibers are the Corpus Callosum and the arcuate fasciculus.
Association Fibers Types
- Intrahemispheric
- Superior Longitudinal Fasciculus
- Inferior Longitudinal Fasciculus
- Superior Occipito-Frontal Fasciculus
- Cingulum
- Fornix
- Interhemispheric
- Body of Corpus Callosum
- Forceps Major of Corpus Callosum
- Forceps Minor of Corpus Callosum
- Anterior Commisure
- Posterior Commisure
Integrative Fibers
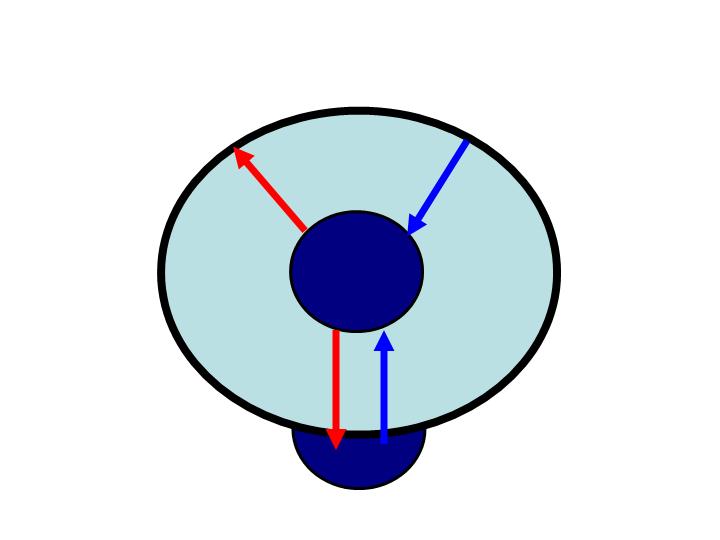 In this model we have arrows that have either the origin or end point within the circle but one of the ends is not located in the perimeter of the circle.
In this model we have arrows that have either the origin or end point within the circle but one of the ends is not located in the perimeter of the circle.
This represents fibers connecting the cerebral cortex with other gray matter areas of the CNS (e.g.: the thalamus, the cerebellum). Fibers connecting cerebral non-cortical gray matter areas are also considered within this group. These are the "Integrative Fibers." Two examples of fibers of this type are the thalamic-frontal fibers and the rubro-thalamic fibers.
Integrative Fibers Types
- Thalamo-frontal fibers
- Fronto-thalamic fibers
- Fronto-striatal fibers
- Thalamo-lenticular fibers
- Rubro thalamic fibers
- Mamilo-thalamic fibers
- Ponto-rubro-thalamic fibers
- Fronto-ponto-cerebellar fibers
- Nigro-thalamo-frontal fibers
- Medial Longitudinal Fascicle
- Many others
Tracts on DTI
DTI stands for Diffusion Tensor Imaging. This is an imaging technique based on the 3D shape of water diffusion. Free diffusion occurs equally in all directions. This is termed "isotropic" diffusion. If the water diffuses in a milieu having barriers, the diffusion will be uneven. In such a case, the relative-mobility of the molecules from the origin has a shape different from a sphere, most frequently an ellipsoid. Barriers can be many things --cell membranes, axons, myelin, etc; but in white matter the principal barrier is the myelin sheath of axons. Bundles of axons provide a barrier to perpendicular diffusion and a path for parallel diffusion along the orientation of the fibers. This is termed "anisotropic" diffusion.
Anisotropic diffusion is expected to be increased in areas of high mature axonal order. Conditions where the myelin or the structure of the axon are disrupted, such as trauma, tumors, and inflammation reduce anisotropy, as the barriers are affected by destruction or disorganization.
Anisotropy is measured in several ways. One way is by a ratio called "fractional anisotropy" (FA). An anisotropy of "0" corresponds to a perfect sphere, whereas 1 is an ideal linear diffusion. Well defined tracts have FA larger than 0.20. Few regions have FA larger than 0.90. The number gives us information of how asymmetric the diffusion is but says nothing of the direction.
Each anisotropy is linked to a orientation of the predominant axis (predominant direction of the diffusion). Post-processing programs are able to extract this directional information.
This additional information is difficult to represent on 2D grey-scaled images. To overcome this problem a color code is introduced . Basic colors can tell the observer how the fibers are oriented in a 3D-coordinate system: This is termed an "anisotropic map." Our software encodes the colors in this way:
- Red indicates directions in the X axis: right to left or left to right.
- Green indicates directions in the Y axis: posterior to anterior or from anterior to posterior.
- Blue indicates directions in the Z axis: foot-to-head direction or vice versa.
Notice that the technique is unable to discriminate the "positive" or "negative" direction in the same axis.
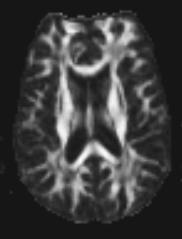 Fractional anisotropy image. White pixels (dots) correspond to high values of fractional anisotropy (FA). Dark pixels correspond to low values of FA. White matter consists of axons, which serve as barriers for free water diffusion, and explains the high anisotropy which is bright compared to cortex where there is less structure and more free diffuse resulting in lower sign.
Fractional anisotropy image. White pixels (dots) correspond to high values of fractional anisotropy (FA). Dark pixels correspond to low values of FA. White matter consists of axons, which serve as barriers for free water diffusion, and explains the high anisotropy which is bright compared to cortex where there is less structure and more free diffuse resulting in lower sign.
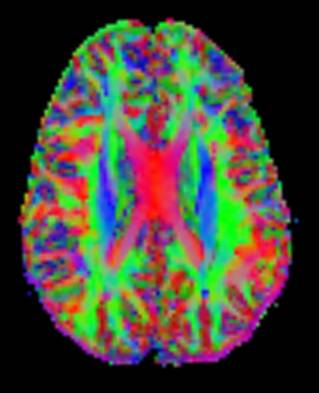 Color coded fractional anisotropy map. Pixels are now displayed in colors to reveal the predominant direction of the diffusion tensor. Green shows fibers oriented anterior-to-posterior or posterior-to-anterior. Red shows fibers oriented right-to-left or left-to-right (e.g.: corpus callosum). Blue shows fibers oriented head-to-foot or vice versa (e.g.: the pyramidal tracts in the corona radiata, lateral to the corpus callosum).
Color coded fractional anisotropy map. Pixels are now displayed in colors to reveal the predominant direction of the diffusion tensor. Green shows fibers oriented anterior-to-posterior or posterior-to-anterior. Red shows fibers oriented right-to-left or left-to-right (e.g.: corpus callosum). Blue shows fibers oriented head-to-foot or vice versa (e.g.: the pyramidal tracts in the corona radiata, lateral to the corpus callosum).
Main Cerebral Tracts on
Orthogonal Fractional Anisotropy Maps
Cerebral tracts may be presented in 2D color images in: axial, coronal, and sagittal planes. The relational topographic appearance of the tracts are better identified in planes that are perpendicular to the major axis of the tract. For example, the corpus callosum which is an axial structure is better defined in the sagittal or coronal view. Thus, tracts going anterior-posterior or posterior-anterior are better seen in coronal view. Descending and ascending tracts are better depicted in axial view (Figure 1).
Figure 1. Axial FA Map. We have targeted blue fibers which encodes for foot-head or head-foot direction.
- Ext: External.
- IC: Internal Capsule
- IOFF: Inferior Occipito-Frontal Fasciculus
- Post: Posterior
- Cort: Cortical
- Thal: Thalamic
- Bulb: Bulbar
- ILF: Inferior Longitudinal Fasciculus
Notice that the portion of the ILF and IOFF shown are just some bundles ascending in the posterior portions as these fasciculi are predominantly posterio-anterior oriented.
Coronal view (figure 2) is better to show the fibers oriented posteior-anterior or anterior-posterior, coded in green.
Figure 2. Coronal FA Map.
- SOFF: Superior Occipito-frontal Fasciculus
- SLF: Superior Longitudinal Fasciculus
- IOFF: Inferior Occipito-frontal fasciculus
- ILF: Inferior Longitudinal Fasciculus.
- SCP: Superior Cerebellar Peduncle
The sagittal plane (figure 3) best provides information on interhemispherical fibers going right to left or viceversa (red) or anterior-posterior (green). These are the corpus callosum and the anterior commissure.
Figure 3. Saggital FA Map. Interhemispheric fibers are red in the midsagittal cut. Horizontal portion of the cingulum above the corpus callosum appears green. The green bundle in the inferior left corresponds to the medial part of the superior cerebellar peduncle.
Subcortical U fibers appear various colors due to multiple intersecting planes.
Patients, Families & Global Community
Mission Statement
To inspire hope and promote lifelong health by providing the best care to every child.
Vision
We will be where the children are, providing comfort through exceptional nursing care.
Philosophy
The philosophy of Nursing at Nicklaus Children's Hospital reflects the vision and values of our organization. We support an environment that promotes professional nursing practice, which emphasizes several key principles:
- The delivery of patient care is guided by comfort principles, family centered, and family directed care.
- Each patient is unique and an integral part of a family unit.
- The delivery of patient care ensures respect for the dignity, values, religious and cultural norms of our children and families.
Nicklaus Children's Hospital Values & Guiding Behaviors
At Nicklaus Children's Hospital, our values and guiding behaviors define how we work together for our patients and families. We have created six statements that reflect our values. Each one has examples of the behaviors that are representative of the value. We call these our values & guiding behaviors. We commit to live, talk and promote these values & guiding behaviors, provide one another with feedback and coaching with respect to the values, and ensure we have observable and consistent progress toward these values being a way of life for all of us at Nicklaus Children's Hospital.
- We Collaborate.
- We take Responsibility.
- We Empower employees to take initiative in making the best decisions for child and family.
- We Advocate.
- We are Transformational, constantly inspiring valuable and positive change.
- We are Empathic while serving the child and family.
Collaborative Relationships
Academic Partnerships
Nicklaus Children's Hospital's goal is to provide a friendly and unforgettable learning experience for nursing students at all levels. By allowing nursing students to rotate within the patient care units, operating room and urgent care centers; they are exposed to the wide array of specialties in nursing and assisted in gaining insight into the development of their future professional goals.
Nicklaus Children's Hospital presents Pediatric Clinical Excellence awards bi-annually honoring exceptional students that rotated through the hospital. Nicklaus Children's Hospital sponsors several community school events. Partnership and participation in community research consortiums. Nicklaus Children's Hospital nurses assume roles as adjunct clinical faculty in various nursing schools throughout South Florida.
Nicklaus Children's Hospital offers a Student Nurse Intern Program (SNIP), which provides nursing students the opportunity to be hired as care assistants to gain insight into the field of nursing. Nicklaus Children's Hospital collaborates with the Nursing Consortium of Florida in hosting "A Day in the Life of a Nurse", a shadowing program to encourage Junior and Senior High School students to consider a career in nursing.
Student Nurse Intern Program
Day in the Life of a Nurse
- Nicklaus Children's Hospital collaborates with The Nursing Consortium of Florida in hosting a "Day in Life of a Nurse," a shadowing program to encourage junior and senior high school students to consider a career in nursing.
Nurse Scholars Program
- Nicklaus Children’s Hospital has partnered with local community accredited nursing academic institutions to offer funding for students accepted to nursing programs. During the program, nurse scholars work as a SNIP to gain insight into the pediatric nursing field and may be offered employment into the Horizon Nurse Residency Program upon graduation.
Collaboration with Clinical and Non-Clinical Departments
Interdisciplinary collaboration remains an integral component of Nicklaus Children's Hospital nursing practice. As nurses, we value collaborative teams co- led within multiple disciplines and believe that effective collaborative teams improve patient care processes and outcomes. Clinical and Non-Clinical Departments that collaborate with nursing are:
Clinical Departments
- Inpatient pharmacy
- Pulmonary Care
- Physical Therapy
- Occupational Therapy
- Preventive Medicine
- Food and Nutrition (Clinical Dietitians)
- Bioethics
- Child Life
- Research Institute
- Infection Prevention and Control
- Ambulatory Units
- Dialysis Unit
- Infusion Unit
- Pediatric Care Center
- Critical Care Units
- Pediatric Intensive Care Unit (PICU)
- Neonatal Intensive Care Unit (NICU)
- Pediatric Cardiac Intensive Care unit (CICU)
- Emergency Department
- Urgent Care Centers
- Inpatient Units
- Pediatric Surgical/Orthopedic Unit
- Psychiatry Unit
- Neurology and Neurosurgical Unit
- Renal/Gastroenterology/Endocrinology Unit
- Respiratory Unit
- Hematology/Oncology and Immunology Unit
- Infant Care Unit
- LifeFlight® Critical Care Transport Program
- Radiology Department
- Surgical Units
- Same Day Surgery Unit
- Cardiac Catheterization Lab
- Operating Room
- Post Anesthesia Care Unit
- Minor Procedure Suite
Nursing Professionalism & Values
Professional Development
Nurse leaders at Nicklaus Children’s Hospital value professional certification and professional development to achieve optimum outcome for patients. Understanding subspecialty certification is proven to increase the quality of care delivery, improve patient safety and outcomes, validate professional experience and strengthen credibility. The organization has created partnerships with various credentialing bodies to provide financial incentives to participate in professional nursing organizations and achievement of national certification.
The organization covers the cost of review courses, allowing nurses to access these study resources free of charge. Professional development is supported through conference participation provided by the Frida Hill Beck endowment fund. Tuition reimbursement is offered to support nurses in advancement of formal education.
Research and Evidence Based Practice
Nursing research is an integral part of nursing practice at Nicklaus Children's Hospital. This research includes quality basic and clinical research focused on understanding health and illness experiences. The nursing shared leadership Research & EBP Council supports and coordinates nursing research activities, and members serve as mentors to staff who conduct research projects.
ANA Code of Ethics
The ANA Code of Ethics for nurses is the fundamental core of nursing practice. The Code of Ethics provides nurses with ethical and legal direction within their profession to ensure optimal quality of care is provided at all times. All nurses are expected to practice in accordance with the ANA Code of Ethics as their professional standard of practice at Nicklaus Children's Hospital.
Florida Nurse Practice Act
The Florida Nurse Practice Act defines the scope of practice for nurses and ensures by licensure that all nurses practicing in the state of Florida meet minimum requirements for safe practice. The Florida Nurse Practice Act represents the laws that govern and regulate nursing’s scope of practice within the state of Florida.
ANA Scope and Standards of Practice
The ANA Scope and Standards of Practice are the standards of professional performance for nurses. These standards describe a competent level of behavior that all nurses in the profession are expected to perform in professional activities within their role appropriate to their education and position. The ANA Scope and Standards direct the profession of nursing and provide the foundation for nursing practice.
Peer Review
The 1988 ANA defines Peer Review as "an organized effort whereby practicing professionals review the quality and appropriateness of services ordered or performed by their professional peers." Peer Review aids in the evaluation of the quality and quantity of nursing care, helps determine strengths and weaknesses of nursing care, provides evidence for change in practice protocols to improve care, and identifies practice patterns that indicate need for more knowledge.
At Nicklaus Children's Hospital there are two forms of peer review. The first form of peer review is incident-based peer review that is evaluated through the peer review committee and the second form is unit-level peer to peer feedback based on objective clinical practice.
Recognition and Rewards
Nursing recognition at Nicklaus Children's Hospital is designed with the ongoing goal of empowerment in nursing through the leadership and dedication of the staff to nursing excellence.
Various employee recognitions are given to staff throughout the year for their consistent dedication to excellence. Some of the various recognitions are:
- Daisy Awards and PETALS
- Certified Nurses Breakfast
- Going the Extra Mile campaign
- Employee Service Awards
- Star of the Month
- External Awards and Recognitions
- Preceptor Recognitions
- Nurse Resident Recognitions
- Management Forum Recognitions
- HAC Recognitions
- Nurse's Week Awards
- Nurse of the Year
- Nurse "Rookie" of the Year
- Outreach Nurse of the Year
- Preceptor Nurse of the Year
- Support Staff of the Year
- Inter-professional Nurse of the Year
- Scholar Nurse of the Year
- Team of the Year
- Nurse Leader of the Year
The departmental recognition programs help to engage employees as well as our patients and family members to recognize each other on a unit level.
Compensation Rewards
- Striving Towards Exemplary Professional Practice (STEPP): the nursing professional ladder that provides staff nurses across all settings with a professional development and monetary incentive to go above and beyond in their practice, education, and professionalism. Nurses are given points in a variety of categories to promote nursing professionalism including: education, professionalism, clinical skills, experience, certification, special projects and councils. These points are accumulated during the nurse’s annual evaluation as one of the components on performance appraisal and merit increases.
- Success Sharing: an employee incentive plan to drive service and clinical excellence. Nicklaus Children's Hospital rewards employees when the hospital achieves its performance targets for patient satisfaction, clinical and operational excellence.
Leadership
Nursing Shared Leadership Council
The Nursing Department of Nicklaus Children's Hospital is competently led by transformational leaders who empower nurses to shape their practice and improve patient care through utilizing their voice within the nursing department via several resources/opportunities within the Nursing Shared Leadership Council (NSLC) Structure.
Nurses across all settings are highly encouraged to become actively involved in membership within the Nursing Shared Leadership Councils enabling them to influence the organizational decision making processes. Staff nurse involvement in the NSLC is pivotal to the success and positive outcomes achieved from these councils. Learn more.
CNO Advocacy
The Chief Nursing Officer advocates for the department of nursing across all levels of the organization. It is through her advocacy with the other members of the Senior leadership team that Nicklaus Children's Hospital has accomplished improving patient outcome, decreasing blood stream infections, increasing patient safety, implementation of patient and family centered care rounds, improved staffing and much more.
The CNO serves as the Patient Safety Officer and is responsible for assuring that the hospital promotes a safety-supportive culture that is consistent with evidence-based practice; identifies and analyzes trends from adverse-events; implements pertinent and preventive patient safety initiatives; provides/supports education related to patient safety; disseminates information, including findings from adverse events or root cause analysis across the organization, and finally, ensures that the organization provides clinical excellence in the safest patient environment.
Some of the mechanisms that the staff are able to communicate with the CNO and allow for the CNO to better advocate for the staff are unit-specific: listening sessions, "Take your CNO to Work Day," and nursing townhalls.
Community & Organizational Leadership
Healthy Connects in Community Schools
This initiative provides preventive and basic school health services in an effort to decrease absenteeism and improve the health outcomes of students. This program provides an Advanced Practice Registered Nurse (APRN)/licensed practical nurse (LPN), licensed clinical Social Worker and two health aides to high-risk schools. Nicklaus Children's Hospital currently services 9 schools throughout Miami-Dade County.
Help for Haiti Hydrocephalus Team
Nicklaus Children's Hospital has a volunteer surgical team that visits Haiti to perform life-saving free of charge corrective surgeries. The surgical team consists of two Neurosurgeons, three Registered Nurses, a Nurse Practitioner, two surgical technicians, one attending Anesthesiologist, one or two certified & nurse anesthetists. The surgical team typically treats 15-20 children in two and a half days; each day consisting of 12-13 hours. Since the program began in 2002, more than 200 children have been surgically treated for hydrocephalus.
Nicklaus Children's Hospital Camps
Nicklaus Children's Hospital nurses participate in activities with children and provide ongoing nursing care in the summer camps that benefit children with special needs. Nicklaus Children's Hospital serves diverse populations of children with chronic diseases. All camps are an interdisciplinary collaboration that offers the children with developmentally appropriate games, crafts, fieldtrips, disease education and support groups. Many of Nicklaus Children's Hospital's nurses are involved in the organization and/or coordination of these camps. Some of the camps are:
Camp U.O.T.S. is an annual weeklong, overnight camp for children with cancer and blood disorders who are treated at Nicklaus Children’s Hospital.
Camp Roaring Sun is a camp exclusively for children with diabetes who are treated at Nicklaus Children's Hospital.
Camp DMC is a summer program for children with special needs run by Nicklaus Children’s Dan Marino Outpatient Center.
VACC Camp is a week-long sleep-away camp that creates unprecedented recreational and fellowship opportunities for children requiring ventilator assistance and their families.
Camp Superstar is a three-day sleep away camp for children with craniofacial conditions.
Succession Planning
Succession planning is one aspect of talent management that identifies and develops employees within an organization with potential, in order to fill in key positions as and when they become available or vacant. The decision to nominate individuals as leaders or high potentials is not an easy task. To identify talent, one must work with individuals identify competencies that they will need to successfully fill a selected role. Leaders also need to provide development opportunities to assess if the potential successor is ready for the role.
At Nicklaus, we provide such opportunities through coaching, mentoring and stretch project programs that help leader determine strengths and opportunities of the potential successor in order to close out gaps before filling the selected role.
Nicklaus Children's offers and opportunity for Clinical Nurses to shadow various roles in nursing through it's L.E.N.S. (Leadership Exploration Nurse Shadowing Experience) Program. We also offer the Emergency Leader Program that provides staff with fundamentals or leadership development.
Preceptorship/Mentoring
All new nurses are assigned a preceptor to help them successfully assimilate into our culture and their new role in our organization. A preceptor is assigned to a new nurse for 8 to 16 weeks of orientation, depending on the type of unit that they work in. In order to ensure that the preceptors are effective, they attend a preceptor development course which teaches them the different roles of a preceptor. An effective preceptor has shown to increase the success of the new hires, increase the retention rate and the overall satisfaction of the new nurses. Once the new nurse is off orientation, the preceptor mentors the new hire to continue to help them grow professionally.
The Horizon Nurse Residency Program has a formalized mentoring program embedded to help foster professional development and enhance organizational enculturation among graduate nurses transitioning to the practice setting.
Patient Care Delivery and Outcomes
Family Centered Care
The delivery of nursing care to children at Nicklaus Children's Hospital is guided by principles of Family-Centered Care. The Nursing Department believes that each child is unique and an integral part of the family unit. Families are involved throughout the course of their child's care and are considered valued partners in the delivery of care. At all times, the nursing team strives to respect the dignity, values, religious and cultural beliefs of children and families.
All aspects of nursing care at Nicklaus Children's Hospital revolve around the concept of incorporating the parent and child's needs into the care of the child. Nicklaus Children's Hospital recognizes that supporting the needs of the patient, their family and their caregivers facilitates their involvement in the planning and delivery of care.
Nicklaus Children's Hospital accomplishes this by utilizing the following:
Comfort Model
The Nursing Department’s Conceptual Framework is Katharine Kolcaba’s Comfort Model. Nurses at Nicklaus Children's Hospital provide comforting measures for patients with an expectation of positive outcomes as described in The Comfort Model. The Comfort Model reinforces the need to comfort nurses. Dr. Katherine Kolcaba’s Comfort theory is embedded within Nicklaus Children's Hospital and its employees. Dr. Kolcaba addresses comfort utilizing the four contexts of holistic human experience listed below:
Physical
- Breaks
- Gym, healthy lifestyle incentives
Psycho-spiritual
- Employee Assistance Program
- Nursing support groups for new nurses
- Leadership support and encouragement
- Schwartz Rounds
- CHAT
- Project Dear
Sociocultural
- iCREATE Way - our organizational culture
Environmental
- Adequate staff and resources to perform job duties
- Healing Garden
- Serenity Rooms
Evidence-Based and Outcome-Driven Practice
The Nursing Department at Nicklaus Children's Hospital supports, engages, and empowers nurses to initiate nursing research, evidence-based practice (EBP) projects, and quality improvement initiatives throughout the organization. Nurses at all levels of care are continuously encouraged to explore and apply the most current and best practices, as well as to generate new knowledge when an identified need arises. Integration of EBP and nursing research into clinical and operational processes aligns with the Nursing Department’s commitment to provide high quality care and positive patient outcomes. Dr. Danielle Altares Sarik PhD, APRN, CPNP-PC directs nursing research through her role as Research Nurse Scientist at Nicklaus Children’s Hospital.
At Nicklaus Children’s Hospital we constantly evaluate, critique, and update nursing practice based on emerging evidence, patient- and family-outcomes, and evolving best practices. In order to guide nursing practice, the Johns Hopkins Evidence-Based Practice Framework is taught to all incoming nurse residents, and continually reinforced to nursing staff, from leadership to bedside. By providing nurses with the tools to evaluate and apply evidence, we create a solid foundation for quality patient care and improved outcomes.
The Department of Nursing, in collaboration with inter-professional stakeholders, reviews and adopts position statements and standards of practice in alignment with groups such as the ANA, Society of Pediatric Nurses, and American Academy of Pediatrics. We provide nursing leadership in the dyad model to the Clinical Effectiveness and Pathways Committee, which reviews and incorporates best evidence into practice at the hospital level.
Each nurse is an advocate for their patients and the families to whom they provide care, and we promote nurse autonomy at Nicklaus Children’s. It is of utmost importance that each nurse is able to practice to the full scope of their license and training, utilizing critical thinking, flexible problem solving, creativity, and scholarship to achieve optimal patient outcomes. We practice in collaboration with our interprofessional partners, and are full and valued members of the care team.
Ethics & Compliance
Nicklaus Children's Hospital has established a compliance department and program to advance the prevention, detection, and correction of violations of federal, state or local law or regulations governing health care and human services programs by employees, contractors or agents. The compliance staff is available as valuable resources in decision-making processes or to answer questions regarding the ethical conduct of practice at Nicklaus Children's Hospital. The Interdisciplinary Bioethics Committee is a forum that is consulted upon to hear complex ethical issues and provides directives for the healthcare team to address and to provide best practice to the ill and hospitalized child.
Magnet Standards
The American Nurses Credentialing Center (ANCC) Magnet Recognition Program recognizes healthcare organizations such as Nicklaus Children's Hospital for exceptional quality in patient care, nursing excellence and innovations in nursing practice. The Nursing Department at Nicklaus Children's Hospital strives to continuously meet and exceed these standards providing high-quality patient care with improved patient outcomes and patient satisfaction.
iCREATE Way
iCREATE Way is a system-wide training program developed with staff input reflecting expected work behaviors and the creation of a positive work environment as well as a positive patient/family experience. The organizational values and guiding behaviors of collaboration, responsibility, empowerment, advocacy, transformation, and empathy are discussed with demonstrations on how to practice these behaviors in the workplace. The iCREATE training empowers nurses to be better professionals that will in turn provide better care; therefore, further improving customer satisfaction.
Horizon Nurse Residency Program
In 2014, Nicklaus Children’s Hospital created the Horizon Nurse Residency Program, an ANCC accredited evidence-based nurse residency program for new graduate nurses. The Horizon Nurse Residency Program provides an extensive orientation that allows nurses to effectively transition into their new role as a registered nurse in an acute care pediatric setting. Training consists of didactic classes, skill training, simulation labs, unit-specific training with a preceptor, and self-directed computer modules. The program offers training within hospital units including the ICU setting, hematology-oncology, Emergency Department, and the ICU Float Pool, with the duration varying by unit of hire. The Horizon Nurse Residency Program prepares graduate nurses in every way possible to create a competent and happy workforce.
Bridge Nursing Program
In the 2016, the Bridge Nursing Program was developed to successfully onboard experienced nurses without acute care pediatric nursing experience. The program was created in alignment with key attributes from the Horizon Nurse Residency Program, which has improved outcomes such as increased retention and engagement. The Bridge Nursing Program training utilizes various educational modalities such as didactic classes, skill training, simulation labs, unit-specific training with a preceptor, competency-aligned performance, and self-directed online modules. Due to the transition nurses’ previous knowledge and experience, these nurses have a shorter clinical orientation time.
The Bridge Nursing Program qualifications includes any registered nurse with less than 6 months of acute care RN experience. The Bridge Nursing Program prepares experienced nurses in every way possible to create a competent and happy workforce.
DAISY Award
 The DAISY Award is an international program that honors excellence in nursing. It was created by The DAISY Foundation to recognize the clinical skills, extraordinary compassion and care exhibited by nurses every day. The award is given monthly to an outstanding nurse in more than 237 hospitals across the United States and around the world. UnitedHealthcare is the co-sponsor of The DAISY Award at Nicklaus Children's Hospital. The DAISY Award to honor nursing was founded in memory of J. Patrick Barnes.
The DAISY Award is an international program that honors excellence in nursing. It was created by The DAISY Foundation to recognize the clinical skills, extraordinary compassion and care exhibited by nurses every day. The award is given monthly to an outstanding nurse in more than 237 hospitals across the United States and around the world. UnitedHealthcare is the co-sponsor of The DAISY Award at Nicklaus Children's Hospital. The DAISY Award to honor nursing was founded in memory of J. Patrick Barnes.
The DAISY Award recipient is recognized at a public ceremony and receives: a framed certificate, a DAISY Award signature lapel pin and a hand-carved stone sculpture entitled A Healer's Touch. Additionally, the unit or department of the recipient will receive cinnamon rolls – a favorite of Patrick's during his illness – with the sentiment that the heavenly aroma will remind them how special they are and how important their work is.
Nominate a Nurse for the Daisy Award
DAISY Award recipients personify Nicklaus Children's Hospital's remarkable patient experience. These individuals consistently demonstrate excellence through clinical expertise, extraordinary service and compassionate care and are recognized as outstanding role models in the nursing community.
The following are examples of qualities and attributes the nurses will possess:
- A positive attitude
- “Patient centeredness” - a consistent focus on meeting patient and family needs
- Collaborates well with all members of the health care team
- Excellent interpersonal skills
- Shows empathy in all situations
Patients, visitors, employees or physicians may nominate a deserving nurse by filling out the nomination form online and submitting it to the nominee's nursing manager.
Tools and Forms
Links and Resources
Educational Resources
- http://www.cebm.utoronto.ca/
The goal of this website is to help develop, disseminate, and evaluate resources that can be used to practice and teach EBM for undergraduate, postgraduate and continuing education for health care professionals from a variety of clinical disciplines.This site also serves as a support for the book entitled, Evidence-based Medicine: How to practice and teach EBM by David L. Sackett, Sharon E. Straus, W. Scott Richardson, William Rosenberg, and R. Brian Haynes
- http://www.med.umich.edu/pediatrics/ebm/
This site is a resource for evidence-based pediatrics provided through the University of Michigan. The site includes a list of CATs, a CAT template (step by step guide on how to create a CAT), guidelines for starting a journal club and links to other websites.
- http://ktclearinghouse.ca/cebm
The Centre has been established in Oxford as the first of several centres around the country whose broad aim is to promote evidence-based health care and provide support and resources to anyone who wants to make use of them.
- StatSoft Electronic Statistics Textbook
- HyperStat Online Statistics Textbook
Tutorials
- http://www.nlm.nih.gov/bsd/disted/pubmed.html
Brief animated tutorials with audio for using PubMed.
- http://www.hsl.unc.edu/services/tutorials/EBM/welcome.htm
This tutorial was developed by the Duke University Medical Center and the health science library at UNC-Chapel Hill. This tutorial is intended for any health care practitioner or student who needs a basic introduction to the principles of Evidence-Based Medicine.
- http://library.downstate.edu/EBM2/contents.htm
SUNY Downstate Medical Center Evidence Based Medicine Tutorial
- http://www.mclibrary.duke.edu/subject/ebm?tab=overview
This website provides links to other tutorials
Databases and Resources
- BMJ clinical evidence
- The Cochrane Library
- DynaMed
- FirstCONSULT
- InfoPOEMS
- PubMed
- Trip Database
- UpToDate
- AskMedline
Review of Resources
- http://library.ncahec.net/ebm/pages/resources.htm
This website lists resources, including databases, journals, and books, that libraries or individuals might want to consider adding to their collections to support the teaching and learning of evidence-based medicine.
- http://weblogs.elearning.ubc.ca/googlescholar/sourcesofevidence.pdf
A list of Web-based resources produced by the University of British Columbia. Provides links to resources and notes whether "open" or "closed" access.
- http://www.myhq.com/public/a/l/alper
A free internet portal designed for physicians that includes more than 100 web sites for finding medical information.
Critically-Appraised Topics on the Web
- CAT Maker
CATmaker is a software tool which helps you create Critically Appraised Topics, or CATs, for the key articles you encounter about Therapy, Diagnosis, Prognosis, Aetiology/Harm and Systematic Reviews of Therapy.
- http://www.med.umich.edu/pediatrics/ebm/Cat.htm
A list of critically appraised topics in Pediatrics produced by the University of Michigan.
Links and Resources
CME Forms (Faculty and Planners)
CME Forms for Faculty/ Speakers:
Helpful Tools and Samples:
CME Forms for Activity Chairs and Planners:
CME Policies and Procedures:
References and Resources:
CME Mission Statement
Nicklaus Children's Hospital's mission is to “inspire hope and promote lifelong health by providing the best care to every child”. As a teaching institution Nicklaus Children's Hospital is committed to supporting the professional and educational needs of its health care providers, and the lifelong learning of the interprofessional team with the aim to provide the best possible care to every child. Continuing medical education (CME) is one of the major ways in which Nicklaus Children's Hospital supports its overall mission.
CME Purpose
Nicklaus Children's Hospital is committed to advancing the knowledge, enhancing the competence and performance in practice of clinicians, with the ultimate goal of improving patient outcomes through the design and delivery of high-quality, evidence-based, race-conscious continuing medical education (CME) programs that focus on patient care, medical knowledge, practice-based learning and improvement (i.e. Quality Improvement, patient safety, research), interpersonal and communication skills, professionalism, and systems-based practice (i.e. Interprofessional education). The CME programs focus on common practice guidelines, advances in medicine, new medical technology, biomedical research, healthcare quality, eliminating disparities in healthcare, promoting health equity and patient-centered care, to meet the constantly changing health care environment.
Content Areas
The CME Committee utilizes the ACGME/ABMS/ IOM core competencies as a platform for content areas. The contents are developed based on annual and continuous needs assessments for the overall institutional CME program and individual activities. The needs assessment process identifies “gaps” in attendees’ knowledge, competence and/or performance. Other sources of content include hospital-specific or national patient care initiatives, peer-reviewed published literature, re-licensure requirements, maintenance of certification or accreditation, hospital committee-identified gaps or needs for improvement, and various practice and referral patterns. CME activities are planned in the context of desirable physician attributes and core competencies to promote dissemination of high quality practice patterns and serve the best interest of the public. Topics are assigned to the activity that is best suited for its target audience and delivery format. The content of Nicklaus Children's Hospital CME activities includes, but not limited to, a) all aspects of patient care (diagnosis, management, and prevention) of children in the areas of primary and subspecialty pediatric problems, b) quality improvement, c) medical ethics d) faculty development e) clinical and translational research, f) business of medicine and risk management g) hot and emerging topics.
Target Audience
Nicklaus Children's Hospital's CME activities are provided to:
- Pediatricians, House Staff physicians, medical students, pediatric subspecialists in medicine & surgery
- Pediatric researchers
- National and international clinicians
- Allied health and members of multidisciplinary/interprofessional teams
- Parents/family representatives
Types of Activities
Nicklaus Children's Hospital offers a range of CME activities including the following:
- Regularly scheduled series (RSS), e.g. Grand Rounds, Faculty Development, Tumor Board, Radiology Conference, Community-Based Educational programs, and Trauma and Cardiology Conferences
- Live Courses: e.g. General Pediatric & Pediatric Critical Care Board Review Courses, Pediatric Post Graduate Course (PPGC)
- Virtual/e-learning/online education – This includes live transmission of courses and/or archived/video-on-demand enduring materials
Expected Results
The expected result of Nicklaus Children's Hospital's CME is to:
- Improve physician competence measured by outcome assessment (including knowledge, skills and attitudes)
- Improvement in performance-in-practice through assessment of intent of behavior change and implementation of practice change
- Improved patient outcomes through self-reported improvement or quality improvement data or EMR data when feasible. It is also hoped that as clinicians improve their competence and performance, this will translate into improvement of patient outcomes meeting ultimately the hospital’s and health system’s mission to “inspire hope and promote lifelong health by providing the best care to every child”.
Last Review – July 2024
CME Committee
| Committee Member |
Role |
Liaison to other committees |
| Rani Gereige, MD, MPH - Committee Chair |
Director of Medical Education |
- GMEC, Chair
- Library Committee, Chair
- Mortality & Morbidity Review Committee, Member
- IT PAG for EMR, Member
|
| Jefry Biehler, MD, MPH |
- Chair of Pediatrics - FIU
- Med Students Clerkship Director
|
- GMEC, Member
- IT PAG for EMR, Chair
- Mortality & Morbidity Review Committee, Member
- Utilization Review and Quality, Physician Reviewer
|
| Beatriz Cunill, MD |
Pediatric Residency Program Director |
- GMEC, Member
- ICU Committee, Member
- IT PAG for EMR, Member
- Quality Pillar/ Blue Chip, Member
|
| Jose Rosa-Olivares, MD |
General Pediatrics - Attending |
IT PAG for EMR, Member |
| Elizabeth Menocal |
Senior Director, Medical Staff Resources |
- Blue Chip on IV Infiltration, Member
- Credentials Committee, Member
- Medical Executive Committee, Member
- Bylaws Committee, Member
|
| Shakeva Swain, RN |
Coordinator, Trauma RSS |
- Trauma Physician Peer Review, Planner
- Trauma Quality Management Committee, Member
- Hospital Safety and Compliance Committee, Member
|
| Gabriela Martinez |
CME Specialist
(e-Learning, Marketing, Social Media, and Website) |
|
CME COMMITTEE MEMBERS ROLES AND RESPONSIBILITIES (Click to view)
Planning Your Meeting
Meeting planners or program chairs wishing to request CME sponsorship from the Department of Medical Education at Nicklaus Children's Hospital for their planned educational activities are required to follow the steps and timeline below in starting the application process. Click on the links below to be directed to a step-by-step planning process for your CME activity.
5 months before activity
Activity Chair, CME Director, and Committee
Activity Chair awaits notification of approval of Activity Request. All COIs should be resolved prior to proceeding with the planning process.
Activity Chair and CME Staff
- Schedule a meeting with CME Staff to discuss steps and CME Checklist deadlines.
- CME Department provides an orientation to the Nicklaus CME website, forms, and roles.
4-5 months before activity
Activity Chair
Once all COIs of activity director and planner are resolved, complete and submit a CME Application Form along with the following documents:
- Draft agenda
- List of confirmed speakers
- Proposed Budget (Contact the CME Department for the template.)
- Marketing Materials (when ready) for review
- AV Request Form
- Proposed Evaluation Forms
If activity is a Regularly Scheduled Series, the activity chair must complete one of the following:
- CME Application Form for the entire series, if the sessions have the same theme
- CME Application Form for the entire series and an RSS addendum for each session, if the sessions vary in theme
CME Staff
The CME Department designs the activity's registration site or dedicated landing page based on feedback from the Activity Chair and Planners.
4 months before activity
Activity Chair
If soliciting educational grants or exhibitor support, submit one of the following:
- Educational grants - A signed Written Agreement for Commercial Support for each commercial entity
- Exhibitors - A signed exhibitor agreement
Please note that there are differences in policy between exhibitors and educational grants. All grants requests and exhibitor agreements MUST be reviewed by CME staff prior to execution in order to ensure compliance.
CME Staff
The CME Department sends letters to faculty to collect faculty disclosures, CVs, and other documents.
2 months before activity
Activity Chair or Planner(s)
OPTIONAL - Submit a revised preliminary budget.
During the activity
Activity Planner(s)
- Maintain accurate sign-in sheets.
- Collect evaluation sheets from attendees:
- Faculty Evaluation
- Activity Evaluation
- Pre and Post Surveys
2 weeks after activity
Activity Planner(s)
Submit all sign-in sheets, evaluations, and forms collected during the event to the CME Department.
1 month after activity
CME Staff
- The CME Department grants CME credits based on attendance records, sign-in sheets, and/or evaluation forms.
- Emails are sent to attendees with instructions on claiming their CME certificates.
2 months after activity
Activity Chair or Planner(s)
- Submit copies of final syllabus and/or handouts.
- Submit a final budget report. (Contact the CME Department for the template.)
CME Staff
The CME staff distributes the Evaluation Summary Reports to CME Director (and optionally, to the Activity Chair).
- Speaker Valuation by Learners
- Event Evaluation by Learners
- Pre/Post Survey Gap Analysis Report
3 months after activity
Activity Chair
If applicable, consider a 3-month Post-Activity Survey to assess practice change.
Clinical Neurophysiology Fellowship
Craniofacial Fellowship
Pediatric Critical Care Fellowship
Pediatric Emergency Medicine Fellowship
Pediatric Radiology Fellowship
Cardiac Intensive Care Fellowship
Pediatric Urology Fellowship
Pediatric Cardiology Fellowship
Pediatric Neurosurgery Fellowship
Meet Our Subspecialty Fellows
Pediatric Surgery Fellowship
Pediatric Hospitalist Fellowship
Appointment Request
Central Scheduling
Search
News
Error Page
rss
rss
Health Information Library
Ana-margarita-duarte-dermatology
anthony-wolfe-plastic-surgery
chad-perlyn-plastic-hand-surgery
rafael-rivas-chacon-rheumatology
roberto-tuchman-dan-marino-center
Trevor J. Resnick, M.D.
aaron-berger-plastic-hand-surgery
alisa-muniz-crim-gastroenterology
rafael-portela-otolaryngology
sandeep-dave-otolaryngology
parul-jayakar-clinical-genetics-and-metabolism
roberto-warman-ophthalmology
israel-alfonso-neurology
jahangir-asghar-orthopedic-surgery
john-ragheb-neurosurgery
miladys-palau-collazo-endocrinology
alejandro-diaz-endocrinology
andrew-labbie-urology
luis-caicedo-oquendo-gastroenterology
mislen-bauer-clinical-genetics-metabolism
rafael-gosalbez-urology
zenia-aguilera
gaston-decardenas-otolaryngology
michael-duchowny-epilepsy
redmond-burke-cardiovascular-surgery
rosa-monte-fernandez-general-pediatrics
ruben-gonzalez-vallina-gastroenterology
stephen-swirsky-orthopaedic-surgery
william-muinos-gastroenterology
adriana-carrillo-iregui-endocrinology
robert-cullen-neurology
erick-hernandez-gastroenterology
madeleen-mas-cardiology
marcel-deray-neurology
maria-franco-pulmonary-medicine
michael-tidwell-orthopaedic-surgery
antonio-rodriguez-pulmonary-medicine
craig-spurdle-orthopedic-surgery
enme-corrales-reyes-neurology
felix-ramirez-seijas-nephrology
john-grossman-plastic-surgery
jorge-hernandez-chaple-psychiatry
luis-gonzalez-mendoza-endocrinology
p-marcelo-laufer-infectious-diseases
richard-arboleda-gastroenterology
andres-orjuela-otolaryngology
carlos-gadia-dan-marino-center
marisa-azaret-behavioral-medicine
vivian-hernandez-trujillo-allergy-and-immunology
yamilet-tirado-otolaryngology
Harry Shufflebarger
cathy-anne-burnweit-pediatric-surgery
International Patient Registration Form
In order to schedule appointments we first need a fully-completed registration form and all related medical records (including any imaging, laboratory, etc). Once Global Health receives all relevant information, your case will be reviewed by the medical staff. Be advised that routine appointments are generally scheduled for dates 2-4 weeks after your case has been initiated with a coordinator. If this is an urgent medical request requiring an appointment within two weeks, please contact Global Health directly.
If you need to reach the Global Health Department, please call:
Local Phone: (305) 662-8281 or Toll-free: (888) 797-6010.
Pre-Registration for a Medical Procedure
If you have any questions concerning the completion of this form, please call 305-663-8413.
On your Admission/Registration day, please bring your prescription, Health Insurance card, other Insurance cards and your Credit Card you may be required to pay a deductible, co-pay, payment or deposit if applicable.
Deposits/Co-payments: Deposits/CO-payments are determined by your insurance company and based on specific plan benefits. For most services, the co-payment will be listed on your insurance card. CO-payments/Patients portions are due at the time of service.
Thank you
Success! Your information has been submitted, and an agent from our staff will be in contact with you shortly.
Thank you for contacting us.
On your Admission/Registration Day
Please bring:
- Prescription
- Health Insurance card, other Insurance cards
- Credit Card (you may be required to pay a deductible, co-pay, payment or deposit if applicable).
Deposits/Co-Payments
Deposits/CO-payments are determined by your insurance company and based on specific plan benefits.
For most services, the co-payment will be listed on your insurance card.
CO-payments/Patients portions are due at the time of service.
Conditions We Treat
login
CME Disclosure Form
Vanity Urls
Xmplify
Victor Center Screening Request
Please fill out this form and we'll be in touch with you shortly!
Victor Center Screening Request
Please fill out this form and we'll be in touch with you shortly!
Victor Center Screening Request
Please fill out this form and we'll be in touch with you shortly!
Thank You
Success! Your information has been submitted. Thank you.
Return to the Victor Center.
Thank You
Success! Your information has been submitted. Thank you.
Return to the Victor Center.
Marino Adapted Aquatics Certification Registration
Thank you for your interest in registering for the Marino Adapted Aquatics Certification!
Thank you
Success! Thank you for registering for the Nicklaus Children's Hospital Marino Adapted Aquatics Certification!
Please allow up to 3 business days for your payment to be processed after you
pay using the buy now button below. Once your payment is processed, you will receive a confirmation email that will contain your exam link and password to access the on-line exam.
Please
download the course manual. You will need to study the manual prior to taking the exam. If you have any questions, please email
Jamie.Tarshis@nicklaushealth.orgKevin Horowitz
john-kuluz-general-pediatrics
ana-paredes-nephrology
gil-wernovsky-cardiac-critical-care
abdulwahab-aldousany-cardiology
abisola-odunmbaku-radiology-house-officer
adam-stuart-general-pediatrics
adolfo-llanos-martinez-neonatology
adriana-cadilla-general-pediatrics
adriana-castro-general-pediatrics
agustin-arrieta-general-pediatrics
alan-chu-otolaryngology
alberto-cotton-pediatric-medicine
alberto-fernandez-otolaryngology
alberto-lopez-ambulatory-pediatrics
alberto-tano-neonatology
alejandro-martinez-general-pediatrics
alessandra-milesi-halle-neurology
alessandro-acosta-neonatology
miguel-castellan-urology
david-coe-behavioral-medicine
david-drossner-cardiology
elza-vasconcellos-neurology
octavio-carreno-otolaryngology
sayed-naqvi-neurology
susan-benenati-allergy-and-immunology
americo-padilla-psychiatry
amit-patange-cardiology
aparna-rajadhyaksha-clinical-genetics-and-metabolism
guillermo-de-angulo-hematology-oncology
kristin-kozakowski-urology
marco-danon-endocrinology
mark-epstein-neurology
moises-simpser-pulmonary-medicine
r-antonio-portela-otolaryngology
ronald-kanter-cardiology
ziad-khatib-hematology-oncology
ian-miller-neurology
carmen-ramos-irizarry-pediatric-surgery
jesse-reeves-garcia-gastroenterology
metee-comkornruecha-adolescent-medicine
nelson-sanchez-neurology
anselmo-cepero-akselrad-nephrology
arelis-martir-negron-clinical-genetics-and-metabolism
arielle-hay-rheumatology
avi-baitner-orthopaedics
james-losito-podiatry
leopoldo-malvezzi-pediatric-surgery
leslie-garrard-adolescent-medicine
michael-brody-pediatric-dentistry
migvis-monduy-neurology
steven-fishberger-pediatric-electrophysiology
toba-niazi-neurosurgery
jose-rosa-olivares-general-pediatrics
nolan-altman-radiology
oscar-loret-de-mola-gastroenterology
yadira-martinez-fernandez-cardiology
robert-vogt-lowell-cardiology
roberto-gomara-gastroenterology
iris-silverberg-general-pediatrics
lorena-siqueira-adolescent-medicine
rose-alvarez-salvat-clinical-psychology
rose-alvarez-salvat-clinical-psychology
danyal-khan-cardiology
enrique-escalon-hematology-oncology
ibrahim-amjad-plastic-surgery
jose-vargas-general-pediatrics
lina-felipez-gastroenterology
marielys-rodriguez-varela-general-pediatrics
michael-geraldi-general-pediatrics
ricardo-restrepo-radiology
anthony-hogan-pediatric-surgery
otto-ramos-infectious-diseases
brandon-korman-clinical-psychology
reuven-bromberg-rheumatology
sarah-jernigan-neurosurgery
fred-telischi-otolaryngology
carlos-diaz-pulmonary-medicine
enrique-acosta-pediatric-dentistry
nancy-dobrolet-cardiology
william-decampli-cardiovascular-surgery
colin-knight-pediatric-surgery
deise-granado-villar-preventive-medicine
john-rock-gynecology
kamar-godder-hematology-oncology
osbel-borges-oral-surgery
oscar-papazian-neurology
ann-hyslop-segeren-neurology
athena-pefkarou-cancer-center
beatriz-cunill-de-sautu-general-pediatrics
carolina-sanchez-vegas-infectious-diseases
enrique-canton-general-pediatrics
gary-kramer-general-pediatrics
janet-rosen-clinical-psychology
jorge-perez-neonatology
juan-carlos-muniz-cardiology
mario-martinez-pediatric-dentistry
mimi-abella-blanco-general-pediatrics
paula-schleifer-neurology
stacey-kruger-ophthalmology
alex-koetzle-neonatology
alvaro-dangond-general-pediatrics
arthur-bregman-psychiatry
cecilio-lopez-cardiology
g-keith-meyer-critical-care-medicine
haneen-abdella-hematology-oncology
holly-neville-pediatric-surgery
jaime-edelstein-general-pediatrics
jefry-biehler-emergency-medicine
juan-ruiz-unger-general-pediatrics
milagros-huerta-endocrinology
norman-ruiz-castaneda-general-pediatrics
sheila-conway-orthopedic-surgery
deirdre-marshall-plastic-surgery
jorge-dediego-general-pediatrics
jose-bengochea-general-pediatrics
amanda-porro-general-pediatrics
iran-niroomand-rad-ambulatory-pediatrics
l-santiago-medina-radiology
manuel-cotilla-infectious-diseases
oscar-arevalo-pediatric-dentistry
robert-hannan-cardiovascular-surgery
jose-garri-plastic-surgery
kathryn-eisermann-rogers-allergy-and-immunology
plato-alexander-cardiac-intensive-care
rayza-cordero-general-pediatrics
w-christian-bauer-anesthesiology
yvelice-villaman-bencosme-general-pediatrics
zubin-panthaki-plastic-surgery
armando-acevedo-general-pediatrics
h-temple-orthopedic-surgery
ramiro-perez-jr-plastic-surgery
steven-melnick-pathology
Volunteer Spotlight
Administrative Fellowship
The Administrative Fellowship at Nicklaus Children's Health System is a one-year opportunity that provides unique and valuable experience for professional growth. The fellowship program establishes a platform for creating meaningful relationships within the organization and the South Florida community. The fellows will be regarded as members of the Executive Leadership Team (ELT) and will have access to key decision-making processes through interaction and observation at leadership, medical staff, community, and Board of Directors meetings.
In addition, the fellows will further enhance their experience and knowledge of Nicklaus Children's Health System and Nicklaus Children's Hospital by conducting core administrative and clinical rotations throughout the organization. The fellows will have the opportunity to rotate through all entities within the health system. Project-related work designed to further develop interpersonal and analytical skills will be customized to meet the interests of the fellows, as well as meeting immediate needs of Nicklaus Children's Health System. The fellows will report directly to the President and CEO of Nicklaus Children's Health System.
2024-2025 Administrative Fellows
Testimonials from our Fellows
Advance Practice Nurses (APN)
An Advanced Practice Nurse (APN) is a nurse with a Master’s degree from an accredited university. The APN collaborates with the healthcare team (s) to develop the plan of care. The APN provides a broad range of health care services, which may include some of the following:
- Taking the patient’s medical history, performing physical examinations, ordering laboratory and diagnostic tests and other procedures as necessary.
- Diagnosing, Treating, and Managing diseases
- Ordering medications and writing prescriptions
- Coordinating referrals
- Providing information on disease prevention and healthy lifestyles
- Performing medical procedures as approved by specific training
- Care Coordination of services
- Education for patients, families, caregivers, other staff and the community
- Clinical support to research teams in order to improve and provide best practice.
- Nursing Informatics: integrating nursing science with computer and information science utilizing the knowledge and wisdom of nursing practice to manage and communicate data through technology.
What titles do Advanced Practice Nurses have?
- ADVANCED REGISTERED NURSE PRACTITIONER
- PEDIATRIC NURSE PRACTITIONER
- FAMILY NURSE PRACTITIONER
- CLINICAL SPECIALISTS
- NURSE EDUCATOR
- CERTIFIED REGISTERED NURSE ANESTHETIST
- NURSE ADMINISTRATOR
- NURSING INFORMATICS
Where do you find Advanced Practice Nurses?
- Hospitals
- Clinics
- Out-patient health centers
- Home health programs
- Teaching in colleges and universities and collaborating
- Research programs
- Governmental agencies
What are the requirements for licensure?
Nurse Practitioners in Florida are required to have board certification through a national nursing organization specializing in adult care, pediatric care, or family health, examples of credentialing organizations are, (American Nurses Credentialing Center, National Association of Pediatric Nurse Practitioners).
andrea-maggioni-general-pediatrics
bonelle-klinger-anesthesiology
bruce-eisenberg-general-pediatrics
diego-pernudi-general-pediatrics
francisco-medina-general-pediatrics
gloria-pelaez-general-pediatrics
isabel-gomez-general-pediatrics
juan-carlos-meneses-paz-general-pediatrics
luis-perez-burnes-general-pediatrics
maria-rivero-general-pediatrics
mark-young-allergy-and-immunology
marty-mcgraw-radiology
peggy-hui-anesthesiology
ramon-maldonado-general-pediatrics
rene-andino-general-pediatrics
rose-gedeon-pediatric-dentistry
sara-rivero-conil-clinical-psychology
tara-loux-general-surgery
teresita-fox-general-pediatrics
valerio-toyos-general-pediatrics
vicente-roger-general-pediatrics
lysette-iglesias-endocrinology
jose-perez-rodriguez-endocrinology
mark-limosani-endodontics
erin-arroyo-pediatric-dentistry
purnahamsi-desai-neonatology
matthew-bordegaray-radiology-house-officer
paul-khalil-general-pediatrics
yedda-gomes-ruane-pediatric-dentistry
jack-bandel-neonatology
rafael-alcalde-oral-surgery
rolando-molina-otolaryngology
jason-katz-pediatric-intensivist
danielle-madril-section-of-cardiovascular-anesthesia
andrew-price-orthopaedic-surgery
beny-rub-general-pediatrics
carmen-alfonzo-general-pediatrics
claudia-arango-general-pediatrics
dibanni-vasquez-general-pediatrics
elizabeth-welch-cardiology
e-oliver-aregullin-eligio-cardiology
eysa-marquez-brito-general-pediatrics
frank-kronberg-otolaryngology
jacqueline-valdes-rafuls-general-pediatrics
jadrien-young-otolaryngology
joaquin-gomez-general-pediatrics
jorge-landa-pediatric-dentistry
jose-herrera-general-pediatrics
kara-del-valle-neonatology
karen-franco-emergency-medicine
m-antonella-denaro-emergency-medicine
maria-gaviria-tobon-ambulatory-pediatrics
maria-gutierrez-general-pediatrics
mark-webman-pediatric-dentistry
melissa-clemente-general-pediatrics
michele-saverin-pediatric-dentistry
michel-nahmad-pediatric-surgery
peter-martinez-noda-general-pediatrics
philip-floyd-general-pediatrics
roberto-cubeddu-cardiology
sandra-rivera-luciano-ambulatory-pediatrics
sebastian-padron-ambulatory-pediatrics
teresa-lozano-oral-surgery
terilee-wunderman-clinical-psychology
vanessa-guerra-general-pediatrics
efren-salinero-general-pediatrics
laura-umbrello-general-pediatrics
maura-cintas-general-pediatrics
melissa-reyes-salgueiro-behavioral-medicine
ricardo-palmquist-radiology-house-officer
sameh-hussein-neonatology
leonard-rothenberg-orthodontics
ausberto-hidalgo-general-pediatrics
fanny-gonzalez-nephrology
gilda-torres-portalatin-general-pediatrics
ania-cabrerizo-pediatric-dentistry
esther-marin-casariego-general-pediatrics
pedro-alquizar-bermudez-orthodontics
antonio-suarez-family-medicine
balagangadhar-totapally-critical-care-medicine
kimberly-kimmel-anesthesiology
luisa-cervantes-radiology
marc-linares-emergency-medicine
margarita-fernandez-pujol-general-pediatrics
maria-chatani-pediatric-dentistry
maria-teresa-gomez-general-pediatrics
martha-toledo-valido-general-pediatrics
romulo-cuy-jr-anesthesiology
andleeb-usmani-dermatology
antonello-podda-hematology-oncology
audina-berrocal-ophthalmology
brian-dougherty-otolaryngology
camilo-zambrano-general-pediatric
esperanza-pacheco-jacome-radiology
fernando-beltramo-critical-care-medicine
frank-wang-anesthesiology
gisele-mardy-general-pediatrics
johannes-lopez-general-pediatrics
jose-bello-neonatology
kevin-fox-family-medicine
maria-milla-general-pediatrics
martha-pernas-general-pediatrics
pedro-sanchez-diaz-general-pediatrics
andre-raszynski-critical-care-medicine
belkys-bonnelly-general-pediatrics
gilda-moreno-clinical-psychology
isidro-lopez-general-pediatrics
joaquin-jimenez-decardenas-general-pediatrics
manuel-soler-general-pediatrics
marcos-mestre-general-pediatrics
mark-ginsburg-general-pediatrics
nina-ramirez-allergy-and-immunology
paola-correa-pediatric-dentistry
stephanie-gonzalez-periodontics
edward-ziga-hematology-oncology
ernesto-valdes-neonatology
pedro-lopez-general-pediatrics
anthony-rossi-cardiology
bernardo-pimentel-neonatology
carole-brathwaite-pathology
clara-lagueruela-general-pediatrics
claudia-fernandez-castro-pulmonary-medicine
claudia-rodriguez-pediatric-dentistry
daniela-egas-bejar-hematology-oncology
dario-lirman-general-pediatrics
david-lowe-emergency-medicine
david-mendez-soto-neonatology
deborah-barbouth-clinical-genetics-and-metabolism
derek-sanders-orthodontics
eduardo-perez-pediatric-surgery
edwin-liu-neurology
emilio-lopez-general-pediatrics
f-amed-soliz-neonatology
f-m-antonieta-schettino-general-pediatrics
francisco-martinez-general-pediatrics
hector-quevedo-radiology
john-oeltjen-plastic-surgery
joseph-michienzi-plastic-surgery
kelli-nayak-general-pediatrics
livia-delgado-general-pediatrics
maggie-fader-hematology-oncology
marcos-akerman-general-pediatrics
margaret-okonkwo-general-pediatrics
aramys-barzaga-psychiatry
michelle-blumstein-emergency-medicine
m-l-d-caroline-hetu-neonatology
sandra-ivanier-temkin-general-dentistry
silvia-sommers-clinical-psychology
vicente-chavarria-allergy-and-immunology
alfredo-murciano-infectious-diseases
barbara-pena-emergency-medicine
claudia-villela-pereira-cardiology
daniela-arroyo-larrea-general-pediatrics
elise-zimmerman-general-pediatrics
giselle-faubel-behavioral-medicine
hernan-cruz-neonatology
isabel-ferreira-general-pediatrics
jorge-luis-bertran-general-pediatrics
luis-llamas-pediatric-dentistry
magaly-diaz-barbosa-neonatology
mario-reyes-ambulatory-pediatrics
mark-gabay-general-pediatrics
mercedes-gonzalez-dermatology
michael-owens-otolaryngology
michelle-smitley-pediatric-dentistry
richard-vivero-otolaryngology
rigoberto-nunez-general-pediatrics
samantha-carella-clinical-psychology
seth-thaller-plastic-surgery
ana-maria-castaneda-ambulatory-pediatrics
ana-maria-paez-emergency-medicine
cristina-montiel-general-pediatrics
maritza-vila-rivas-general-pediatrics
miriam-estevez-general-pediatrics
rodney-baker-emergency-medicine
roger-drew-stoudt-general-pediatrics
sergio-alzugaray-general-pediatrics
daniel-castellanos-psychiatry
daniel-green-emergency-medicine
william-brown-otolaryngology
edwin-cordero-general-pediatrics
maria-behnam-terneus-general-pediatrics
orlando-arce-cardiology
andrew-schell-otolaryngology
claudia-herrera-echeverry-general-pediatrics
doured-daghistani-hematology-oncology
hugo-perez-general-pediatrics
jibin-samuel-anesthesiology
jose-carpio-allergy-and-immunology
jose-fernandez-general-pediatrics
lisa-perez-grossman-general-pediatrics
manuel-pedroso-general-pediatrics
ramon-guevara-general-pediatrics
richard-gelman-endodontics
vincenzo-maniaci-emergency-medicine
elba-iglesias-adolescent-medicine
eric-peterson-neurosurgery
joaquin-fuenmayor-otolaryngology
juan-sola-pediatric-surgery
mario-rub-pulmonary-medicine
daniel-alfonso-orthopedic-hand-surgery
victoria-fierro-cobas-general-pediatrics
william-coombs-iii-emergency-medicine
christopher-tirotta-section-of-cardiovascular-anesthesia
alfredo-torralbas-general-pediatrics
amarfis-garcia-saint-hilaire-pediatric-dentistry
anjeza-chukus-radiology-house-officer
brett-mckeon-radiology-house-officer
carlos-handal-saca-general-pediatrics
corinne-althauser-general-pediatrics
diana-vargas-general-pediatrics
francisco-pernas-otolaryngology
gabriela-saca-general-pediatrics
gloria-riefkohl-ambulatory-pediatrics
harry-aguero-general-pediatrics
ileana-fuentes-general-pediatrics
janellie-ramos-azaret-general-pediatrics
john-dunlop-emergency-medicine
john-rhodes-jr-cardiology
maigrely-abreu-hernandez-pediatric-dentistry
maria-fernandez-general-pediatrics
maria-trujillo-pediatric-dentistry
mayra-capote-general-pediatrics
melissa-meincken-pediatric-dentistry
melquiades-alvarez-radiology
michael-leoncio-critical-care-medicine
muna-azzo-emergency-medicine
nao-sasaki-cardiology
phillip-kaner-orthodontics
rafael-gonzalez-anesthesiology
ricardo-llorente-general-pediatrics
rosie-roldan-pediatric-dentistry
victor-villegas-ophthalmology
betti-hertzberg-ressler-general-pediatrics
christina-morgan-clinical-psychology
jun-sasaki-pediatric-intensivist
oranit-shaked-emergency-medicine
pedro-reimon-general-pediatrics
phillip-newcomm-jr-general-pediatrics
querube-santana-rivas-neonatology
rachel-pevsner-radiology
rafael-gottenger-plastic-surgery
rafael-llanso-general-pediatrics
rani-gereige-general-pediatrics
rasciel-socarras-general-pediatrics
rene-lopez-guerrero-general-pediatrics
sean-horan-psychiatry
seema-khurana-physical-medicine-and-rehabilitation
shabbir-joher-neonatology
shelley-drummond-neonatology
sobia-naeem-general-pediatrics
sravanti-kurada-neonatology
stephanie-dechurch-general-pediatrics
stephen-george-orthopedic-surgery
steven-fletcher-general-pediatrics
steven-tucker-general-pediatrics
sunil-bochare-general-pediatrics
susan-leitner-general-pediatrics
susanna-mendizabal-general-pediatrics
ta-chang-ophthalmology
tamara-biller-ambulatory-pediatrics
thresia-gambon-general-pediatrics
timothy-murray-ophthalmology
tina-carroll-scott-general-pediatrics
tobias-nobigrot-general-pediatrics
toby-ascherman-general-pediatrics
truc-hoang-neonatology
valeria-salinas-sanchez-general-pediatrics
veronica-etinger-general-pediatrics
victor-gonzalez-quintero-gynecology
william-carroll-neonatology
william-pena-pediatric-dentistry
yamile-guerra-negrete-general-pediatrics
yolanda-galarraga-ramirez-general-pediatrics
yosef-kaweblum-general-pediatrics
nora-daniel-general-pediatrics
omar-de-jesus-costa-cruz-neonatology
pamela-larcada-general-pediatrics
parvine-sadeghi-anesthesiology
paul-kleidermacher-otolaryngology
paul-sudack-general-pediatrics
milica-saper-general-pediatrics
mohamed-samy-elhammady-neurosurgery
monica-payares-lizano-orthopedic-surgery
monica-reina-general-pediatrics
muaz-alabd-alrazzak-hematology-oncology
mustafa-tekin-clinical-genetics-and-metabolism
nancy-elazab-general-pediatrics
nayf-edrees-hematology-oncology
nelson-vega-general-pediatrics
nestor-valeron-emergency-medicine
nicole-bailey-neonatology
nilda-acosta-general-pediatrics
nilsa-toledo-pediatric-dentistry
nivia-vazquez-general-pediatrics
maria-egusquiza-general-pediatrics
maria-fajardo-neonatology
maria-gonzalez-diaz-general-pediatrics
maria-plata-neonatology
maria-pol-carballo-general-pediatrics
maria-ramon-coton-general-pediatrics
maria-smith-pediatric-dentistry
maria-vazquez-general-pediatrics
mariela-urbina-general-pediatrics
marie-nicolas-alexandre-general-pediatrics
mariola-idrobo-cordero-general-pediatrics
marla-friedman-emergency-medicine
marshall-lewis-cardiology
marta-ortiz-perez-pediatric-dentistry
marta-perez-silva-general-pediatrics
martha-ballesteros-radiology
marvin-rios-general-pediatrics
michael-rizkalla-emergency-medicine
rocio-romero-pradilla-neonatology
rodolfo-sidron-general-pediatrics
rogerio-faillace-general-pediatrics
rolando-nunez-allergy-and-immunology
rolando-penate-general-pediatrics
rommel-morales-general-pediatrics
rosa-cuen-leon-rapid-care-center
rosa-junco-diaz-general-pediatrics
rozalyn-lenora-paschal-general-pediatrics
sandra-deris-atassi-behavioral-medicine
sandra-mitjans-general-pediatrics
sanford-levin-general-pediatrics
sarah-legorburu-selem-general-pediatrics
raquel-martinez-ambulatory-pediatrics
richard-lagueruela-section-of-cardiovascular-anesthesia
richard-raffaele-emergency-medicine
richmond-darko-general-pediatrics
robert-o-neill-general-pediatrics
roberto-organero-neonatology
jonathan-fox-family-medicine
john-goldberg-hematology-oncology
jonathan-baumgard-general-pediatrics
mairim-de-la-rua-general-pediatrics
manuel-campo-neonatology
manuel-galguera-general-pediatrics
manuel-lovo-general-pediatrics
manuel-vega-general-pediatrics
marc-arel-general-pediatrics
margarita-hernandez-rosado-neonatology
margarita-taboas-general-pediatrics
maria-almanzar-general-pediatrics
maria-alonso-prieguez-general-pediatrics
maria-canel-morera-general-pediatrics
maria-carballosa-general-pediatrics
miguel-jose-lanz-allergy-and-immunology
neil-gershman-allergy-and-immunology
ivonne-correa-rivas-general-pediatrics
jacqueline-salazar-general-pediatrics
jacques-orces-ambulatory-pediatrics
james-blumenthal-family-medicine
jana-myers-general-pediatrics
janice-lima-maribona-dermatology
jeffrey-kleinberg-general-pediatrics
jesus-rodriguez-angulo-general-pediatrics
john-fort-hematology-oncology
lisabet-diaz-general-pediatrics
lisa-miller-general-pediatrics
liset-pelaez-pathology
lorraine-fuentes-general-pediatrics
lorraine-ospina-herrera-general-pediatrics
lourdes-valdes-fernandez-general-pediatrics
luis-concepcion-general-pediatrics
luis-mendoza-anesthesiology
luis-miranda-neonatology
mabel-bohorquez-general-pediatrics
mabel-coro-pediatric-dentistry
madelyn-dones-general-pediatrics
magali-selem-general-pediatrics
magda-rizer-radiology-house-officer
georges-saliba-general-pediatrics
gina-morgan-smith-general-pediatrics
gisela-diaz-monroig-neonatology
gladys-lopez-urizar-general-pediatrics
gloria-lopez-general-pediatrics
gonzalo-dequesada-general-pediatrics
graciela-nearing-clinical-psychology
greg-ross-orthodontics
guillermo-llosa-general-pediatrics
harold-deulofeut-general-pediatrics
heather-smith-neonatology
hector-trujillo-general-pediatrics
helene-lebischak-neonatology
hilda-tejero-general-pediatrics
idalia-lastra-orthodontics
ignacio-zabaleta-neonatology
ileana-romero-bolumen-general-pediatrics
isaac-luzardo-general-pediatrics
israel-alvarez-general-pediatrics
jose-adams-neonatology
jose-pradere-general-pediatrics
jose-pumarino-cardiology
jose-vargas-loayza-emergency-medicine
joshua-zeidenberg-radiology-house-officer
juan-bolivar-cardiac-intensive-care
judith-lederhandler-general-pediatrics
julia-oliveira-general-pediatrics
julie-kantor-general-pediatrics
julio-egusquiza-general-pediatrics
kanchan-mishra-neonatology
karen-kaylee-kuhn-general-pediatrics
kim-murray-otolaryngology
kresimir-aralica-emergency-medicine
kunjana-mavunda-pulmonary-medicine
laila-benbouzid-general-pediatrics
laura-fernandez-ortiz-general-pediatrics
laura-vazquez-general-pediatrics
leanne-shapiro-clinical-psychology
leidiana-figueroa-general-pediatrics
lenore-noel-general-pediatrics
liliane-grand-bois-general-pediatrics
lilia-roque-guerrero-general-pediatrics
alice-blavo-general-pediatrics
alina-siblesz-ruiz-general-pediatrics
andres-bustillo-lopez-otolaryngology
andrew-kairalla-neonatology
angel-junquera-general-pediatrics
angel-san-roman-general-pediatrics
annie-casta-sports-medicine
asim-warsi-general-pediatrics
carolina-akerman-pediatric-dentistry
carolina-escobio-general-pediatrics
danette-torres-general-pediatrics
eduardo-bolumen-general-pediatrics
edward-hillman-otolaryngology
ernesto-erdmann-general-pediatrics
eugene-rivera-otolaryngology
gabriela-rolland-asensi-pediatric-dentistry
jairo-torres-otolaryngology
jason-schulman-general-pediatrics
alfredo-machado-general-pediatrics
allen-lenoir-infectious-diseases
amada-romano-silva-general-pediatrics
andrew-gore-radiology-house-officer
ayleen-pinera-llano-general-pediatrics
carmen-uribe-general-pediatrics
casey-almonte-radiology-house-officer
cyril-blavo-general-pediatrics
edith-davis-general-pediatrics
eduardo-alfonso-ophthalmology
eduardo-diaz-general-pediatrics
ennio-colon-general-pediatrics
eva-hernandez-chin-general-pediatrics
eylin-negrin-anesthesiology
carmen-garcia-paul-orthodontics
angeline-prado-general-pediatrics
barbara-kaszovitz-general-pediatrics
betty-bellman-dermatology
bianca-stefan-general-pediatrics
dayrys-tejeda-pediatric-dentistry
a-jose-wenger-general-pediatrics
carlos-fuster-general-pediatrics
carmen-briceno-crespi-orthodontics
catherine-love-neonatology
celadie-fiallo-jr-general-pediatrics
diana-sredni-general-pediatrics
edward-packer-general-pediatrics
elsie-davila-torres-general-pediatrics
elvira-rives-general-pediatrics
wenliang-geng-general-pediatrics
amelia-armas-general-pediatrics
anish-parekh-otolaryngology
antonia-san-jorge-infectious-diseases
benazeer-jawaid-general-pediatrics
carlos-colon-ambulatory-pediatrics
carlos-guevara-general-pediatrics
christopher-bob-pediatric-dentistry
cristina-pirez-de-cardenas-general-pediatrics
daniel-eason-cardiology
elaine-de-roode-orthodontics
elena-ubals-allergy-and-immunology
erick-naka-mizrahi-general-pediatrics
evelyn-delgado-general-pediatrics
ezequiel-romero-general-pediatrics
fernando-llopiz-martin-general-pediatrics
jonathan-jagid-neurosurgery
efrem-gubieda-general-pediatrics
alicia-serrano-toyos-general-pediatrics
ernesto-prieto-pediatric-dentistry
dhanendra-paramasvaran-neonatology
ha-truong-general-pediatrics
ana-contreras-general-pediatrics
gabriel-chamyan-pathology
Schedule a Test
Allergy & Immunology Fellowship
Pre-operative Surgical Scheduling
Please fill this form in ALL CAPS.
Test Web Form
Board Login
craig-fleishman-cardiology
jessica-kovarik-ophthalmology
joni-leterman-general-pediatrics
serjun-andaya-neonatology
debera-hui-anesthesiology
elyane-haddad-general-pediatrics
felipe-martinez-otolaryngology
Sitemap
eNewsletter
My Nicklaus Children's Patient Portal
To access the Patient Portal you must complete the following steps:
My Nicklaus Children's Portal
If you have not received a Patient Portal invitation by email, please call the HIM department at
305-669-6412
My Nicklaus Children's Patient Portal is available through the My Nicklaus Children's App.
Download it today!
Frequently Asked Questions
Robotic Surgery
Nicklaus Children’s Hospital became the first pediatric hospital in Florida to acquire the da Vinci® Xi™ Surgical System, which can be used across a spectrum of minimally invasive surgical procedures, including general pediatric, abdominal, colorectal, kidney, single-incision, thoracic and urologic surgery.
The da Vinci® Xi™ system offers a three-dimensional high-definition (3D-HD) vision system, special instruments and computer software that allow surgeons to operate with enhanced vision, precision, dexterity and control. The da Vinci instruments have mechanical wrists that bend and rotate to mimic the movement of the human wrist. Physicians in the Department of Pediatric Surgery (Division of Urology) include several who are among the most experienced in the region in performing robotic surgery.
For patients in need of gallbladder, ovarian, and renal surgery, a minimally-invasive option is available thanks robotic single-site incision options. Patients undergo visibly no scarring through this method, which is performed through a small incision hidden within the patients’ navel.
Benefits generally associated with da Vinci surgery include:
- Shorter hospital stay
- Reduced blood loss
- Reduced complications
- Reduced need for narcotic pain medicine
- Faster recovery
- Reduced scarring
Specialized Offerings in Robotics
 A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
 Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Robotic Surgery
Nicklaus Children’s Hospital became the first pediatric hospital in Florida to acquire the da Vinci® Xi™ Surgical System, which can be used across a spectrum of minimally invasive surgical procedures, including general pediatric, abdominal, colorectal, kidney, single-incision, thoracic and urologic surgery.
The da Vinci® Xi™ system offers a three-dimensional high-definition (3D-HD) vision system, special instruments and computer software that allow surgeons to operate with enhanced vision, precision, dexterity and control. The da Vinci instruments have mechanical wrists that bend and rotate to mimic the movement of the human wrist. Physicians in the Department of Pediatric Surgery (Division of Urology) include several who are among the most experienced in the region in performing robotic surgery.
For patients in need of gallbladder, ovarian, and renal surgery, a minimally-invasive option is available thanks robotic single-site incision options. Patients undergo visibly no scarring through this method, which is performed through a small incision hidden within the patients’ navel.
Benefits generally associated with da Vinci surgery include:
- Shorter hospital stay
- Reduced blood loss
- Reduced complications
- Reduced need for narcotic pain medicine
- Faster recovery
- Reduced scarring
Specialized Offerings in Robotics
 A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
 Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Robotic Surgery
Nicklaus Children’s Hospital became the first pediatric hospital in Florida to acquire the da Vinci® Xi™ Surgical System, which can be used across a spectrum of minimally invasive surgical procedures, including general pediatric, abdominal, colorectal, kidney, single-incision, thoracic and urologic surgery.
The da Vinci® Xi™ system offers a three-dimensional high-definition (3D-HD) vision system, special instruments and computer software that allow surgeons to operate with enhanced vision, precision, dexterity and control. The da Vinci instruments have mechanical wrists that bend and rotate to mimic the movement of the human wrist. Physicians in the Department of Pediatric Surgery (Division of Urology) include several who are among the most experienced in the region in performing robotic surgery.
For patients in need of gallbladder, ovarian, and renal surgery, a minimally-invasive option is available thanks robotic single-site incision options. Patients undergo visibly no scarring through this method, which is performed through a small incision hidden within the patients’ navel.
Benefits generally associated with da Vinci surgery include:
- Shorter hospital stay
- Reduced blood loss
- Reduced complications
- Reduced need for narcotic pain medicine
- Faster recovery
- Reduced scarring
Specialized Offerings in Robotics
 A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
A pediatric patient at Nicklaus Children’s Hospital is the first in the U.S. to undergo robotic surgery for renal pelvis reconstruction through a single site incision. Pediatric urologists Dr. Miguel Castellan, Dr. Maurilio Garcia-Maldonado and Dr. Paulo Moscardi used The daVinci® Xi™ Surgical System to perform pyleoplasty surgery through a single site incision in order to reconstruct the child’s renal pelvis and remove an obstruction.
 Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Dr. Ibrahim Amjad, pediatric plastic surgeon, performed the first robotic assisted endoscopic surgery in a child born with an extensive teratoma of naso-oropharyngeal orbital region, a tumor located at the skull base. The surgery, which took place in November 2017, was performed using the daVinci Xi robotic system proctored by Dr. Fuad Alkhoury, pediatric surgeon. This procedure marks the first time a head and neck tumor was successfully removed in a child using the intraoperative robotic surgical system. Using the robot minimized trauma to the patient and provided visualization in high definition, allowing for new views of the surgical site. This novel use of the robotics system created unprecedented access to the location of the tumor permitting precise resection. (Picture from left to right: Dr. Fuad Alkhoury and Dr. Ibrahim Amjad)
Maintenance of Certification (MOC)
Nicklaus Children’s Hospital is approved as a Multi-Specialty Portfolio Sponsor for Maintenance of Certification (MOC) credit through the American Board of Medical Specialties (ABMS) and the American Board of Pediatrics (ABP). This relationship enables Nicklaus Children's Hospital to review and approve ongoing quality improvement projects within the health system that meet the requirements set forth by the ABMS and its boards including the ABP, and the health system’s Portfolio Program Internal Review Committee (IRC).
The ABMS Multi-Specialty Portfolio Program™

- The ABMS Multi-Specialty Portfolio Program™ (Portfolio Program) works with Nicklaus Children's Hospital to recognize the work that physicians are already doing to improve patient care in their practices.
- Physician participation in initiatives approved by the Portfolio Program can earn them Improvement in Medical Practice (Part IV) credit from their ABMS Member Board for the American Board of Medical Specialties Program for Maintenance of Certification (ABMS MOC®).
- Activities in priority QI/PI areas such as communication, efficiency, patient safety, and transition of care, can be submitted directly to the Portfolio Program for consideration. The Portfolio Program's IRC will review the activities according to the standards and guidelines outlined in this document and related to the MOC requirements of the ABMS Member Boards.
Faculty applying for MOC Part 4 credit benefit in multiple ways. Once a project is approved by the internal IRC, MOC credit can be granted to any faculty member who participates and meets minimal requirements for participation. Project applications will be submitted directly to the IRC (instead of the ABP), streamlining the application process for work that we all do to improve patient care. The IRC is available to provide feedback on project proposals to help them reach ABMS and/or ABP MOC standards, if the initial application doesn’t meet the requirements. There is no fee for providers associated with this application for internal projects. Some projects are designated by the Project Leader as restricted for participation to Nicklaus Children's Hospital physicians, and some projects may be opened to external physicians.
Approved Projects
The following projects are currently approved for ABP Part 4 MOC Credit through the Portfolio Sponsorship Program. Unless otherwise stated, these projects are only available to physicians with a relationship to Nicklaus Children's Hospital.
Project Title:
Improve Adherence to the Acute Gastroenteritis Guidelines
Project Expiration Date: June 27, 2023
Approving Board: ABP
Project Description:
There is unnecessary testing being ordered for AGE and unstandardized treatment. The goal of this project is to improve compliance in the ED and Hospitalist Service of AGE guidelines to reduce unnecessary GI laboratory testing and standardized treatment. The goal of this project is to improve compliance with the AGE guidelines by 20% and thus decrease unnecessary GI- specific laboratory testing/antibiotic treatment in children in the ED and Hospitalist Service with the diagnosis of AGE from 3mo to 18y/o by 20%. This project was presented as a poster presentation (after peer-review) at the annual scholarship week. (Poster attached)
Completion Criteria :
Physicians claiming credit must participate in the design, planning, implementation of interventions, review of data, and/or attendance of planning meetings for a minimum of 6 months
To participate, contact the Project Leader: Amanda Leigh Hoffman, MD
Project Title:
Antibiotic Stewardship in the CICU
Project Expiration Date: April 01, 2023
Approving Board: ABP
Project Description:
Overuse of Linezolid in our CICU for empiric Gram positive coverage in situations where Vancomycin is acceptable. Physicians are uncomfortable using linezolid and piperacillin/tazobactam together in patients with healthy kidneys. Culturally, our institution also likes to use linezolid. The aim of this project is to decrease the DOT/1000 days of linezolid within the CICU over the course of two 16 weeks intervention cycles. This is done by developing an algorithm that dictates when linezolid and is not appropriate, educating the CICU team regarding the use of the algorithm and holding antibiotics time-outs to assess ongoing needs for antibiotics. The goal is to decrease to national average the use of linezolid by measuring DOT/1000 days through pharmacy logs in CICU patients over the period of the project.
Completion Criteria :
Participants may claim MOC credit if they actively participated in the planning, implementation of interventions, data review and analysis, attending team meetings over a period of 6 months minimum.
To participate, contact the Project Leader: Jacob Convissar, MD
Project Title:
Improving provider knowledge of current mild traumatic brain injury (mTBI)/concussion guidelines in the Emergency Department (ED)
Project Expiration Date: June 01, 2023
Approving Board: ABP
Project Description:
There are no standardized protocols for the diagnosis and management of mild TBI in the emergency department despite CDC guidelines published in 2018. This is due to a lack of knowledge regarding the new CDC guidelines may be causing this gap. The aim of this project is to improve knowledge of ED providers about current guidelines on mTBI/concussion by 50%. We will obtain pre-and post-intervention surveys of ED staff, provide education to providers on mTBI through education to all emergency department clinicians during staff meeting as well as video and PowerPoint presentations to review mild TBI/concussion guidelines, diagnosis and management.
Completion Criteria :
Physicians can claim credit if they participated in the planning, design, implementation of interventions, data review and analysis and they participated in the QI team meetings.
To participate, contact the Project Leader: Ana Ruiz-Castaneda, MD
Project Title:
Use of Beta-Hydroxybutyrate in DKA Management
Project Expiration Date: May 01, 2023
Approving Board: ABP
Project Description:
Beta-hydroxybutyrate (BHOB) is the predominant ketone body present in patients with DKA. The presence of this ketone body is a useful marker of DKA and can be utilized to monitor resolution. Evaluation of Beta-hydroxybutyrate can help initiate intensive care earlier in patients who are hospitalized with diabetes. Also BHOB functions as a marker of DKA resolution with subsequent de-escalation of intensive care and earlier initiation of subq insulin, possibly leading to decreased hospital admission time for those presenting with DKA. Additionally, this can decrease excessive use of blood gasses and comprehensive metabolic panels in the Pediatric Intensive Care Unit. The aim of this project is to improve DKA management by using/trending beta-hydroxybuturate level in the PICU
Completion Criteria :
Physicians can claim credit if they have participated in the design, planning, or implementation of interventions; or review and analysis of data and attending the QI meeting as a team for a minimum of 6 months
To participate, contact the Project Leader: Gabriela Lins, DO
Project Title:
Improving the Methods for Identifying and Managing Childhood Obesity in PC Setting by an evidence-based approach
Project Expiration Date: March 03, 2023
Approving Board: ABP
Project Description:
Childhood obesity is one of the foremost threats to population health in the United States, which has only increased during the COVID-19 pandemic. The rising prevalence of childhood obesity is associated with the emergence of comorbidities such as obstructive sleep apnea, type 2 diabetes mellitus, dyslipidemia, hypertension, and non-alcoholic fatty liver disease, in addition to psychosocial problems such as low self-esteem, depression, and peer discrimination which carry significant societal and economic burdens. Underdiagnosis of overweight and obese pediatric patients remains a concern. We noticed a potential for improvement of identification and management on the Pediatric Care Center (PCC) at our institution. Identifying obesity and its complications early and initiating appropriate management is crucial in preventing morbidity and mortality. This project will aim at implementing systematization of obesity management in our PCC. We noticed different approaches by varied Resident and Attending physicians. We believe that obesity management could be improved by implementing guidelines and a systematized approach.
Completion Criteria :
In order to claim credits, physicians must participate in the planning, implementation, data analysis, and/ or planning meeting for the QI interventions as part of the team for a minimum of 6 months.
To participate, contact the Project Leader: Eva Maria Glenn Lecea, MD
Project Title:
Implementation of Breastfeeding Curriculum Into Pediatric Residency Training
Project Expiration Date: December 31, 2023
Approving Board: ABP
Project Description:
Exclusive breastfeeding for infants up to 6 months of age is the ideal form of infant nutrition and increasing rates of breastfeeding is a major public health priority. Yet, the AAP has recognized a “lack of knowledge, confidence, and positive attitudes towards breastfeeding counseling” in pediatricians, which is likely due to inadequate education provided during pediatric training. Often mothers encounter problems while breastfeeding and, due to inability or insufficient guidance, they renounce breastfeeding in an earlier stage than recommended. The AAP has developed a breastfeeding residency curriculum that has been successfully implemented at many institutions, however our residency program does not yet have a formal breastfeeding curriculum that will provide the tools to guide mother and families into a successful breastfeeding plan. we aim to address the lack of standardized education in pediatrics residency program.
Completion Criteria :
Physicians may claim credit if they have participated actively in the planning, implementation and evaluation of the project interventions as part of the QI team and attended the QI meetings or participated in the data assessment and analysis.
To participate, contact the Project Leader: Alejandra Frauenfelder, MD
Project Title:
Improving diabetes knowledge in adolescents transitioning form pediatric to adult endocrinology
Project Expiration Date: December 31, 2022
Approving Board: ABP
Project Description:
Adolescents with diabetes mellitus (DM) have knowledge gaps of their condition that persists at the time of transitioning to adult care. The aforementioned adolescents need an opportunity to review this knowledge by means of a dedicated clinic and interactive methods. The aim of this project is:
1. To close important DM knowledge gaps at the time of transition
2. If provided a brief DM knowledge questionnaire, they should be able to improve upon before-intervention scores.
3. Immediately upon completion of education activity and later 3 and 6 months after initial intervention
The intervention involves using an interactive, group educational activity with a certified diabetes educator (CDE) will be held at the transition clinic.
Completion Criteria :
Completion criteria include active participation in the evaluation, administration, or implementation of the intervention and review and analysis of the data and participation in QI meetings over a 6 months period.
To participate, contact the Project Leader: Pedro Pagan Banchs, MD
Project Title:
Increasing Early Hospital Discharge
Project Expiration Date: May 31, 2023
Approving Board: ABP
Project Description:
Hospital crowding and subsequent resource strain have been associated with worse patient outcomes and increased length of stay. As pediatric hospitals face an overwhelming respiratory illness surge in the wake of the COVID pandemic, improving hospital patient flow is all the more critical. Nonetheless, a substantial proportion of patients, nearly 1 in 4 in one pediatric tertiary care study, who are medically ready experience delays in discharge. A growing number of quality improvement initiatives targeting increasing early discharges (EDCs) show promising data on improved emergency department (ED) patient flow without increased readmissions. At our institution, a 309-bed tertiary care pediatric hospital in south Florida, the pediatric hospital medicine team has low early discharge (before 12 pm) rates, with a baseline of 7.6% of all discharges in 2021. We suspect that a combination of workflow, resident comfort-level, and communication challenges contributed to this low percentage. In regards to workflow, attendings and teams round at variable times in the day which often leads to medically ready patients being seen later in the day. Meanwhile, lack of educational support may contribute to residents not identifying discharges early, and preparing them for discharge in a timely manner. Additionally, we identified communication gaps between residents, attendings and the nursing staff once a patient is ready for discharge that contribute to delays. This project aims at increasing early hospital discharges for medically ready Pediatric patients at Nicklaus Children’s Hospital
Completion Criteria :
Attend 3 team meetings, and provide feedback on PDSA cycles during meetings.
To participate, contact the Project Leader: Magi Dickinson, MD
Project Title:
Appropriate Thromboembolic Prophylaxis Therapy in IBD Patients Admitted to the Hospital: A Proposed Risk Stratification Algorithm
Project Expiration Date: Aug 01, 2022
Approving Board: ABP
Project Description:
Thromboembolism (TE) is a potentially life-threatening complication of IBD. The increased risk of TE in adults with IBD is well established, and anticoagulation prophylaxis is being instituted as a standard of care. TE risk in pediatric IBD compared with adults is lower, however studies report an increasing incidence in this population. We aimed to decrease risk in our hospital population given this facts. The aim of the project is to determine the percentage of admitted pediatric IBD patients who received appropriate TE prophylaxis therapy based on a risk stratification algorithm and increase the percentage of IBD patients receiving appropriate prophylactic therapy measured over a 16-week intervention period per cycle.
Completion Criteria :
To claim credit, physicians must be involved in the design, planning, implementation, data collection, analysis, review, or interventions for a minimum of 6 months.
To participate, contact the Project Leader: Maria Susana Lopez Gonzalez, MD
Project Title:
Impact of standardized documentation and migraine treatment on diagnosis, headache burden, and health care utilization in a pediatric population
Project Expiration Date: June 30, 2022
Approving Board: ABP
Project Description:
Migraine headache is a common diagnosis in the pediatric population with a wide variety of both symptomatic presentation and clinical management. Until recently there has been no standardized intervention, and routine neuroimaging is not indicated. Management differs between ER physicians, Hospitalists, and Neurologists based on physician and patient preferences. Furthermore, documentation plays a significant role in accurate diagnosis. Variation is seen in medication management, imaging studies and healthcare utilization. Our quality improvement project will look at the effect of standardizing inpatient migraine treatment and documentation in order to ascertain effects on diagnosis, headache burden and health care utilization.
Lack of standardization in medication management and documentation, contribute to longer treatment duration and suboptimal care. This project aims to improve compliance with a standardized protocol and decrease imaging, length of stay, and readmission rates in this population.
Completion Criteria :
Physicians participating in this project are eligible to claim credit if they have participated in the project design, implementation of intervention, data collection, results review and charting, discussions, or project evaluation over a period of 6 months at least.
To participate, contact the Project Leader: Jacklyn Smith, MD
Project Title:
Improving Depression Screening in Adolescents with Inflammatory Bowel Disease
Project Expiration Date: November 28, 2022
Approving Board: ABP
Project Description:
Patients with IBD have higher depression rates and are at risk for non-compliance, longer inpatient admissions, and complications. Resources (Psychiatry, Psychology, etc.) are available but not all patients with depression can take advantage due to low screening and detection rates. The problem exists because of low index of suspicion and low rates of screening in the outpatient and inpatient settings. The main aim of this project is to increase early detection of depression by 30% in patients > 12 years with IBD admitted to the inpatient unit and provide appropriate resources. Screening is done using the PHQ-9 on all admissions, weekly reminders sent via text to the care team and visual reminders placed in workroom.
Completion Criteria :
Physicians are eligible to claim credit if they participated in the planning, implementation of the interventions, data collection, data analysis, revision of plan, or QI team meetings over a minimum of 6 months.
To participate, contact the Project Leader: Claudia Riera Canales, MD
Project Title:
Improving EBM practice in Pediatric Residency
Project Expiration Date: December 1, 2022
Approving Board: ABP
Project Description:
Evidence-based medicine (EBM) practice is cornerstone for optimal clinical decision making among physicians since it can impact management to benefit the patients with most updated evidence. Residency is a great opportunity to train future doctors in the use of EBM and implement it into their clinical practice. Many barriers exist into EBM practice such as time, knowledge and skills. Identifying those barriers may improve EBM practice among training residents and subsequently improve medical practice. We utilized a standardized EBM questionnaire to obtain a baseline regarding comfort level, knowledge, identify barriers and estimate perceived practice. With the results, a series of workshops were designed to address the identified barriers to EBM application on clinical practice, general knowledge and overall comfort level of residents using EBM resources and terminology. We also implemented an “EBM prescription” reward program that incentivized the formulation of clinical questions and the use of EBM to answer them, which allotted points to residents for each time EBM is used, and were scored using standardized formats by senior residents during rounds.
Completion Criteria :
To qualify for claiming credit, physicians must participate in either the planning, implementation of the interventions, data collection, review of data, data analysis, or QI Team meetings for a minimum of 6 months
To participate, contact the Project Leader: Giancarlo Giovannini, MD
Project Title:
Increasing Awareness of The Montelukast Black Box Warning
Project Expiration Date: March 31, 2022
Approving Board: ABP
Project Description:
In March 2020 the FDA issued a black box warning to montelukast in order to raise awareness among health care providers regarding its potential neuropsychiatric side effects (SE). Montelukast has been associated with both worsened and new-onset suicide, depression, and irritability, among other neuropsychiatric symptoms. Due to the recent nature of the FDA black box warning, we sought to increase provider awareness of black box warning and thereby improve counseling patients regarding the black box warning. This project aims at improving documentation of questioning of pediatric patients of all ages on Montelukast neuropsychiatric effects from (0%) to 50% in one year and improving awareness of black box warning among residents and clinic attendings by 50%.
Completion Criteria :
Physicians are eligible to claim credit if they participated in the design, implementation of interventions, review of the data, or discussions and changes made on the project over a minimum of 6 months period.
To participate, contact the Project Leader: Gabriel Mandel, MD
Project Title:
Standardizing Hearing and Vision Screening in the PCC
Project Expiration Date: March 31, 2022
Approving Board: ABP
Project Description:
The American Academy of Pediatrics (AAP) has put forth recommendations for scheduled hearing and vision screenings. Although screenings at our PCC were being completed, they were not following AAP guidelines regarding recommended ages of screening and subspecialty referral criteria. In addition, if screenings were completed there often was no consistent documentation of the screenings. Inconsistency in documentation made referring to appropriate subspecialties for continuous evaluation and care difficult and it prevented adequate continuity of care. The gap was likely multi-factorial in origin, likely secondary to gaps in education and large patient load/business of the clinic. Our aim was to provide a method to consistently and accurately document hearing and vision screens in order to increase screening rates to 100%. Our time limit was throughout the course of our project, approximately 18 months. Interventions included education of residents, and implementation of note template based on age-specific criteria
Completion Criteria :
To claim credit, physicians should have participated in the project design, planning, implementation of interventions, data collection, analysis of the data, or QI project meetings for a period of minimum of 6 months.
To participate, contact the Project Leader: Elisa Prebble, MD
Project Title:
Improving Pediatric Pain Management Practices Among Hospitalized Patients With Scheduled Non-Opioid Treatments
Project Expiration Date: March 17, 2022
Approving Board: ABP
Project Description:
Pain in the pediatric population is poorly understood and frequently mismanaged. This often leads to prolonged hospitalizations and adverse outcomes. Studies in a variety of populations, especially in the post-operative settings, have shown that scheduled pain medications instead of as needed dosing leads to decreased length of stay, better pain management and decreased opioid use. The aim of this project is to improve the utilization of fixed –schedule acetaminophen/NSAIDs dosing by 20% within the PDSA cycle in hospitalized pediatric patients admitted with skin and soft tissue infections including: cellulitis, abscesses, tonsillitis and gingivitis
Completion Criteria :
Participating physicians are eligible for credit if they participated in the planning, implementation of interventions, measurement of outcomes, review of the data, or feedback and education for a minimum of 6 months.
To participate, contact the Project Leader: Rose Mathews Berry, MD
Project Title:
Improving the Management of Acute Pancreatitis in Keeping With Most Updated NASPGHAN Recommendations
Project Expiration Date: June 01, 2022
Approving Board: ABP
Project Description:
After coming across the 2018 NASPGHAN recommendations released by the NASPGHAN Pancreas Committee for managing Acute Pancreatitis (AP) in pediatric patients, we wondered if our hospital was adequately following these guidelines. We had an idea that we probably were not as we noticed that several AP patients were on only 1x MIVF instead of the recommended 1.5 - 2 x MIVF. We also believed that our attendings tended to fare more on the conservative side of pain management and wondered if this may have an negative impact on adequately managing pain in these patients with AP. Overall, we believe the cause of this gap is due to lack of knowledge regarding the updated guidelines and conservative management practices.
This project aims to increase adherence to NASPGHAN guidelines >90% in 4 domains:
- Early initiation of enteral feeds
- No prophylactic antibiotic use in AP
- Adequate administration of IVFs
- Optimization of pain management
This project was presented at several meetings based on peer-review. Poster and Pathway included as attachments.
Completion Criteria :
In order to be eligible to claim credit, participating physicians must be part of the project through an active role including implementation of the intervention(s), or review of the data, or designing future interventions for the project over a minimum of 6 months period.
To participate, contact the Project Leader: Annette Roberts, MD
Project Title:
Improving adherence to AAP 2011 Febrile seizure guidelines
Project Expiration Date: January 01, 2021
Approving Board: ABP
Project Description:
Work up for simple febrile seizures can be unnecessarily extensive and costly. There is a lack of adherence to AAP 2011 febrile seizure guidelines. The goal of this project is to improve adherence by physicians at NCH to the 2011 AAP guidelines for simple febrile seizures. This is done through (1) Correctly identifying patients who meet criteria for simple febrile seizures and thereby minimizing unnecessary lab work.
Baseline data identified 62.5% of patients who fit the study criteria did not undergo unnecessary labs/imaging, our goal is to increase this to 75% over 12 months period. Interventions included (1) Education about the guideline at the ER staff meetings and residents lecture and show the baseline data with statistics on overuse of labs. (Cycle 1) and (2) Review the data collected monthly and continue to provide the report card/feedback via email to the staff using visual representation. (Cycle 2)
Completion Criteria :
To qualify for credit, physicians must participate in either the care of patients, implementation of the intervention, review and analysis of the data and feedback about future interventions.
To participate, contact the Project Leader: Ana M. Ruiz-Castaneda, MD
Project Title:
Improving Transport Efficiency of Mechanically Ventilated Pediatric and Neonatal Patients through Protocol Implementation
Project Expiration Date: October 29, 2021
Approving Board: ABP
Project Description:
Time at bedside for transport of mechanically ventilated pediatric patients being transported by the Nicklaus LifeFlight Team is impacted by complexity of patients, call back to medical command (accepting physician), excess blood gases leading to delays. This project is ongoing and is in its third cycle. (1) The 1st cycle – Included baseline data and performing a process map with all stakeholders (Process measure) and lead to the creation of a transport protocol which was implemented. (2) 2nd cycle - A 30 day implementation trial and data collection on the new protocol. (3) 3rd cycle - The protocol was expanded to include all mechanically ventilated patients (not just HFOV patients, excluding cardiac patients, <32 weeks gestation, any concern for raised ICP) and collected post-implementation data for 6 months after implementation (in progress). The project aim is to reduce bedside time at outside institution by 10% (from fall of 2019 to fall of 2021) for pediatric and neonatal patients (excluding infants < 32 weeks and cardiac patients) on high frequency oscillatory ventilation by the transport team by instituting new transport protocol.
Completion Criteria:
Active participation in the planning, implementation, data collection, and/or analysis for 6-12 months with participation in the meetings
To participate, contact the Project Leader: Manette Ness-Cochinwala, MD
Project Title:
Addressing COVID-19 Vaccine Hesitancy in Hematology-Oncology Patients
Project Expiration Date: March 31, 2022
Approving Board: ABP
Project Description:
As of December 2020, the FDA approved Pfizer COVID-19 vaccine to populations 16 years and older. Immunization is specifically recommended for populations at high risk of developing severe COVID-19 infection, amongst which are included patients with chronic conditions. In our institution, we follow 25 patients above the age of 16 with Sickle Cell Disease (SCD), of which only 7 have received the COVID-19 vaccine. Also noted by the specialists, the oncology patients have an apparent higher immunization acceptance, so we would determine the acceptance of the vaccine in these two populations and inquire about the social determinants that impact the vaccination rate, such as race or religion.
Recently, vaccine administration was approved for children 12-15 years, increasing the population to be included in our project. This gap could be due to first and foremost lack of adequate information and knowledge about vaccine eligibility, recommendations, and benefits. There could also be a lack of offer from primary care physicians.
Completion Criteria:
Participate in the planning or implementation of intervention and/or data collection and/or analysis. Attend the scheduled QI team meetings. Active meaningful participation for a minimum of 6 months.
To participate, contact the Project Leader: Andrea Montano Ballesteros, MD
Project Title:
ED Headache Protocol
Project Expiration Date: June 29, 2020
Approving Board: ABP
Project Description:
There is inconsistent decision making for treatment, and additionally delays and subsequent prolonged length of stay with patients diagnosed with migraines or headaches. Through our experience, that there is currently no standardization for the care of patients in the ED who present with the primary diagnosis of headache or migraine. With the implementation of a protocol and order set, we plan to decrease the return visits to the ED for patients with the diagnosis of migraine or headache by 10% by the end of 2019. This will be done by the implementation of a protocol in conjunction with the Neurology team, educating the physicians in the ED about the protocol, and subsequently creating a Power Plan within Cerner (EHR).
Completion Criteria:
Participation in either the design, planning, implementation / intervention, data review, analysis and /or QI meetings for a minimum time of 6 months.
To participate, contact the Project Leader: Amanda Cruz-Deweese, DO
Project Title:
Improving Asthma Control Test Use in the Pediatric Care Center
Project Expiration Date: April 29, 2021
Approving Board: ABP
Project Description:
Poor asthma control is a risk factor for further exacerbations and impacts greatly patients’ quality of life. Current asthma recommendations include assessing patient’s level of control. The Asthma Control Test (ACT) is one of several validated asthma questionnaires to evaluate control in pediatric and adult patients. This questionnaire has been validated in patients over the age of four with the aim to identify poorly controlled individuals in need of treatment escalation. The established cutoff value of ACT scores of 19 or less, identifies patients under poor control. Additionally, these patients would benefit most from having a formal Asthma Action Plan (AAP).
The gap is lack of knowledge of staff regarding test importance and knowledge of accessing test and documentation. The aim of this project is to improve ACT documentation in patients with asthma diagnosis at Well Child Checks to 25% over 6 months period
Completion Criteria:
Physicians must participate in the planning, implementation of interventions, data collection, or data analysis and interpretation over a minimum time of 6 months.
To participate, contact the Project Leader: Daniel Urschel, MD
Project Title:
Increasing Appropriate Albuterol Use in the PICU
Project Expiration Date: December 30, 2020
Approving Board: ABP
Project Description:
The inhaled nebulized albuterol use in our PICU is significantly higher than the national average. This might be due to the fact that inappropriate albuterol use/ overuse- for instance for bronchiolitis or for those with URI and no reactive airway or asthma history. The interventions will include posting Classes for Appropriate use in the Fishbowl, as well as share over WhatsAapp and in emails the same information. Emails, WhatsApp messages, discussions, and education with residents, fellows, attendings, pharmacists, nurse practitioners, and respiratory therapists.
The project will be monitored with weekly updates to the fellows and attendings including the reminder of what is and isn’t appropriate albuterol use. data will be tracked and analyzed.
Completion Criteria:
Completion criteria includes active participation in either the design or implementation of interventions, or review and analysis of the data, or providing feedback on the project.
To participate, contact the Project Leader: Deidre Anastas, MD
Project Title:
Improving Transition of Care after Discharge from the NICU: Implementing a Post-discharge Telemedicine Visits
Project Expiration Date: May 30, 2021
Approving Board: ABP
Project Description:
Transition of care from the NICU to home generates significant issues that may lead not only to increase length of stay but also higher post-discharge healthcare utilization, due to hospital readmissions and emergency department visits. This transition is recognized as critical to address opportunities to promote patient safety and high-quality of care. The growth and evolution of telemedicine are opening new avenues for efficient, effective, and affordable pediatric health care services. Outcome studies have shown high parent satisfaction, reduction in absenteeism due to illness, decrease travel time and costs, high rates of visit completion, and reduction in ED and urgent care (UC) visits. The NICU at NCH is a quaternary care children’s hospital providing care to critical patients who are discharged home with medical complexities requiring multiple health care services. Implementing a post-discharge telemedicine visit is aligned within the “Ins and Outs” project’s goal, primary and transition drivers and added to the set of change ideas already implemented for this project. The unit has implemented two post -discharge telemedicine services. One provided by KIDZ Medical Services, the hospital outsourcing company that provides the medical services and academic training to the residents in the NICU. Another telemedicine service is provided by nurses with the project entitled “Baby Step: A telehealth Nursing Intervention to Improve the Transition to Home” supported by a Grant from Florida Blue Foundation.
We identified an opportunity for pediatric residents to participate in the NICU telemedicine activities. Residents will engage with live telehealth learning experiences, explore the role of telemedicine in improving the transition of care for NICU graduates, and embrace the changing models of care resulting from advancing telehealth technologies.
Completion Criteria:
Participants are expected to be an active participant in QI meetings, implementing the intervention, documenting and reviewing data. Meaningful participation/ completion require minimum of 6 months participation
To participate, contact the Project Leader: Adolfo Llanos, MD
Project Title:
Early administration of long-acting insulin during acute diabetic ketoacidosis in children
Project Expiration Date: May 30, 2020
Approving Board: ABP
Project Description:
There is a substantial time lag for reaching the desired home administration time for long acting insulin analog after hospitalization for diabetic ketoacidosis. The patients need to shift their long acting insulin administration time every day by 1-2 hours until they reach the home desired time. Our hospital follows the protocol of long acting insulin administration at the transition time. There are published studies providing the long acting insulin analogs at a fixed times without any complications which can prevent the time lag to reach the home administration time.
Our goal was to reduce the time lag for reaching the home long acting insulin time by 50% in qualifying patients by May 2020 by implementing an electronic medical record (EMR) power plan and medical staff education.
We implemented an EMR power plan in Cerner PowerChart by modifying the Pediatric ICU DKA power plan with tagged protocol, medication dosing and times. All patients admitted for DKA excluding patients < 5 years of age, anyone with concerns for cerebral edema, on home insulin pump, or hemodynamically unstable. We provided education and feedback to medical staffs monthly. We used PDSA to analyze outcomes and implement new interventions.
Completion Criteria:
Physicians participating in the project meet completion criteria if they participated in implementation of the intervention, data collection, analysis or review, and participated in the meetings.
To participate, contact the Project Leader: Kalpana Singh, MD
Project Title:
Clinical Effectiveness Program for the Treatment of Uncomplicated CA-PNA
Project Expiration Date: June 01, 2021
Approving Board: ABP
Project Description:
There is lack of knowledge regarding antibiotic guidelines for uncomplicated CA-PNA. Our chart review revealed that in pediatric patients, greater than >6m, who are hospitalized with uncomplicated community-acquired PNA, we treat with ampicillin only 43.1% of the time. Our goal is to seek improvement in antibiotic stewardship and judicious use of antibiotics in fully-immunized patients, with uncomplicated CA-PNA, meeting inpatient criteria. Our SMART aim is: To increase the use of ampicillin in this population to 50% by August 2020, and to 75% by December 2020. The plan is to achieve that through education, creation of a new CA-PNA HP, and development of PNA pathway with the Clinical Effectiveness Program.
Completion Criteria:
Physicians are eligible for MOC points if they meet the following criteria: Participation in the QI meetings, project review, data review, interpretation, analysis, implementation of the interventions, and / or education of the stakeholder team.
To participate, contact the Project Leader: Sophia Hassor, MD
Project Title:
Improving Venous Thromboembolism (VTE) Prophylaxis in the Pediatric Intensive Care Unit
Project Expiration Date: December 31, 2019
Approving Board: ABP
Project Description:
There is a lack of appropriate prophylaxis (mechanical or pharmacologic) for venous thromboembolism in our PICU. Inadequate education and national guidelines. Mechanical prophylaxis (SCDs) is a low risk, low effort intervention, but there is a not a culture of ordering and implementing them in our unit.
Our goal was to improve VTE prophylaxis (mechanical or pharmacologic) to >75% in qualifying patients (≥12 years of age) by December 2019 by implementing an electronic medical record (EMR) pop-up and automatic order for sequential compression devices in patients who qualify. We implemented an EMR pop-up in Cerner PowerChart with a VTE screening tool to assess risk in patients in the PICU. We then attached an auto-order for SCDs after multiple PDSA cycles to improve appropriate prophylaxis. We used PDSA to analyze outcomes and implement new interventions. The project was completed and was peer-reviewed by my SOC Committee and the DIO (Dr. Gereige) who directs and evaluates the quality of the QI Projects
Completion Criteria:
Participating physicians meet the completion criteria if they participated in the planning, implementation of intervention, review and analysis of the data, and/or assisting with the imporvment process and connection to stakeholders (Via education or practice)
To participate, contact the Project Leader: John Kotula, MD
Project Title:
Standardization of Post-operative Management after Fontan Procedure
Project Expiration Date: June 01, 2020
Approving Board: ABP
Project Description:
Overall mortality and the incidence of early failure after the Fontan operation has significantly decreased over the last few decades, however perioperative morbidities still exist and a considerable number of patients require prolonged hospitalization after the procedure. The aim of this study was to describe our Fontan playbook (a standardized care pathway) and compare the postoperative outcomes with our institutions historical data. Specifically, this study aims at: (1) Describing our Fontan playbook (a standardized care pathway) and compare the postoperative outcomes with our institutions historical data (2) Improvement or goal is to decrease duration of chest tube placement and length of stay (3) The time limit for assessment is on a 6 month basis. Interventions include: 1) Create an algorithm pathway that can be followed by bedside nursing and the primary team to ensure patient is following an expected path of recovery. 2) Introduction of intervention: meeting with RT, nursing, physicians and ensure buy-in to pathway and answer questions prior to each fontan admission. 3) Training in proper use of pathway with flexibility. Ensure copy of pathway is available at bedside.
Completion Criteria:
Physicians must participate in the project for a minimum of 6 months. Participation may include attending QI meetings, reviewing the data collected, and/ or participating in implementation and design of the interventions.
To participate, contact the Project Leader: Kamalvir Gill, MD
Project Title:
Cardiac Arrest Prevention (CAP) Quality Initiative
Project Expiration Date: May 01, 2021
Approving Board: ABP
Project Description:
Cardiac arrest in the cardiac intensive care unit is high and is associated with poor outcomes. Being able to detect early signs of an impending cardiac arrest can allow bedside providers to intervene prior. By implementing the elements of the CAP bundles, bedside providers are able to identify signs of impending decompensation as well as be better prepared if the patient arrests. This project aims at implementation of the 5 elements of the cardiac arrest bundle: twice daily huddles, vital signs posted at bedside, presentation discussion, weight specific epinephrine at bedside, formal review of all arrests Interventions include:
- “CAP SAFETY HUDDLE” – MULTIDISCIPLINARY DISCUSSION OF CA PREVENTION 2 TIMES/DAY, (AM SHIFT, PM SHIFT, CALL HAND-OFF) –GOALS AND PLANS POSTED AT BEDSIDE
- PATIENT-SPECIFIC VITAL SIGN GOALS ESTABLISHED AND ALARM PARAMETERS ADJUSTED & COMMUNICATED/POSTED AT BEDSIDE
- PRE-SEDATION DISCUSSION FOR NOXIOUS STIMULI
- EMERGENCY MEDICATIONS (EPINEPHRINE) AVAILABLE AT BEDSIDE 5.FORMAL REVIEW OF ALL CARDIAC ARREST EVENTS
Completion Criteria:
Physicians who participate in this project will need to meet the following criteria for completion: Participation in meetings of the team, implementation of intervention, review of the data, and/or designing new interventions.
To participate, contact the Project Leader: Kinjal Parikh, MD
Project Title:
Improving Efficacy and Safety of Pediatric Intensive Care Unit Patient Transfers
Project Expiration Date: May 25, 2016
Approving Board: ABP
Project Description:
Patient transfers from the Pediatric ICU were largely inefficient. Time to floor transfer ranged from hours to multiple days. Due to delays, initial handoff from ICU to floor team was inaccurate at the actual time to transfer and transfer orders were obsolete, thus increasing risk of medical errors. While awaiting floor bed, some patients were discharged home from the PICU, but floor team was never notified and patients continued to be counted in the floor team census affecting resident physician-to-patient ratios. This project aims to decrease the time lapse between the notification of PICU transfer to the floor team and actual arrival of the patient to the floor to <120 minutes within one year.
Completion Criteria:
Physicians participating in the project are eligible for MOC Credit if they meaningfully participate in the QI meetings, data review, design and implementation of interventions. Participation for a minimum of 6 months in the project is also a criterion.
To participate, contact the Project Leader: Bhavi Patel, MD
Project Title:
Brief Resolved Unexplained Events (BRUEs)
Project Expiration Date: October 12, 2020
Approving Board: ABP
Project Description:
BRUEs are a relatively new diagnosis, created from the AAP clinical guideline published in 2016. There is currently no data on whether this diagnosis is being correctly applied or on whether patients are being correctly classified as higher or lower risk. There is also no data on whether the recommendations for lower risk patients are being followed (minimal testing, no admission needed) and whether these recommendations are improving clinical outcomes. the Global Aim of this project is: To improve the care and management of infants presenting with BRUE by improving the recognition and classification of BRUE.
This is done using the following interventions proposed:
- Creation of a note template for inpatient H&Ps with BRUE characteristics and risk classification included.
- Conduct education with ED providers, hospitalist attendings and NPs and residents to review BRUE diagnosis, risk classification and recommendations for management.
- Creation of a method for ED providers to give specific discharge instructions for patients with BRUE including information about CPR training.
Completion Criteria:
Physicians participating in the project are eligible for MOC Credit if they meaningfully participate in the QI meetings, data review, design and implementation of interventions. Participation for a minimum of 6 months in the project is also a criterion.
To participate, contact the Project Leader: Kathleen Murphy, DO
Project Title:
Assessment of HIV Screening in Adolescent Patients: A QI Project
Project Expiration Date: June 23, 2019
Approving Board: ABP
Project Description:
Universal HIV screening is recommended in all health-care settings after the patient is notified, unless the patient declines (opt-out screening). HIV screening was not being routinely offered in our institution’s Adolescent Medicine clinic. Residents feel uncomfortable approaching patients regarding sexual behaviors. Ignorance of HIV testing guidelines. Lack of EMR reminders. The Plan Do Study Act method of quality improvement was used. Baseline assessment consisted of a survey to evaluate residents’ knowledge regarding HIV screening guidelines, and a review of patient medical records for 2 weeks pre- intervention looking for documentation of HIV risk factors, previous HIV testing, and discussion/offering of HIV testing. Three PDSA cycles were completed. The aim of this project was to increase the rate of HIV screening offering and discussion to 90% of all patients seen in the adolescent clinic in our hospital in the 2 weeks following the interventions, with the overall goal of increasing rate in the following year.
Completion Criteria:
Physicians participating in the project are eligible for MOC Credit if they meaningfully participate in the QI meetings, data review, design and implementation of interventions. Participation for a minimum of 6 months in the project is also a criterion.
To participate, contact the Project Leader: Michell M. Lozano Chinga, MD
Project Title:
Implementation of a Toolkit for Transition Readiness Assessment in Patients with JIA: A QI project
Project Expiration Date: June 23, 2019
Approving Board: ABP
Project Description:
The American College of Rheumatology (ACR) has recommends assessment of transition readiness (TR) with previously validated tools, for all patients starting at 14 years of age, and interventions to achieve transition readiness by age 21. The Rheumatology clinic at our institution did not have a policy in place for transition readiness assessment. A smooth transition process has been associated with greater rates of patient satisfaction, empowerment and loss of follow up. The project aims to change lack of awareness of the need of a transition policy, lack of EMR reminders. Two cycles were performed. The aim was to increase the rate of TR assessment to 90% during visits to the Rheumatology clinic for patients with JIA, by launching the implementation of a TR toolkit (including GotTransition questionnaire) and advance notification to clinic staff.
Completion Criteria:
Participation in QI meetings, data review, design and implementation of interventions, and feedback.
To participate, contact the Project Leader: Diana Sofia Villacis Nunez, MD
Project Title:
Increasing Discussions on Early Peanut Introduction - A Quality Improvement Project
Project Expiration Date: October 31, 2018
Approving Board: ABP
Project Description:
Resident’s working in our continuity clinic were not aware of the LEAP addendum guidelines therefore they were not practicing these guidelines or discussing peanut introduction at well visits in our clinic. Through the use of education and visual cues, we wanted to increase resident knowledge on the LEAP guidelines. We wanted to improve discussions on peanut introduction at well visits which will include documentation. Lastly we wanted to have appropriate referral for patients that met criteria for the LEAP protocol. Our timeline included 12-18 months- 6 months of pre intervention data and 3 months for each cycle (2 cycles in total). Our goal is to improve documentation at 4 and 6 months well visit on peanut introduction.
Completion Criteria:
Physicians must be involved in the planning/ implementation/ data review/ or discussions of the various aspects of the project. The physicians involvement will be subject to attestation by the project leader.
To participate, contact the Project Leader: Priyanka Seshadri, MD
Project Title:
Improving Pediatric Resident Education at Nicklaus Children’s Hospital NICU
Project Expiration Date: May 31, 2019
Approving Board: ABP
Project Description:
The Accreditation Council for Graduate Medical Education (ACGME) states that for the resident, the essential learning activity is interaction with patients under the guidance and supervision of faculty members who give value, context and meaning to those interactions . With increasing pressures to treat patient as efficiently as possible, teaching of medical students and residents has become a challenge for neonatologists working in the neonatal intensive care unit (NICU). The introduction of the electronic health records has added further burden to the teaching process by shifting focus from the patient to the computer screen. Factors unique to the NICU environment that make the process of teaching more demanding compared to other pediatric rotations are: 1)Opportunities to learn NICU specific material not found in other rotations. 2)Reduction in the number of work areas and NICU rotations required by ACGME. 3)High patient acuity and complexity create a highly stressful NICU environment with fewer opportunities for formal resident education. Factors that are relevant to the NICU at NCH include: 1) Lack of labor & delivery and nursery services which limit the teaching to level IV NICU setting. 2) Lack of a fellowship program. 3) Teaching responsibilities assumed by a group of private practicing neonatologists. 4) Limited knowledge for participant neonatologists about the their teaching responsibility as required by ACGME 5) Two different Electronic Heath Record System for documentation in the NICU creating an additional burden to residents and neonatologists.
Completion Criteria:
Physicians will meet completion criteria by having a 6 months participation period in the project, participation in the review of the data, implementation of the various interventions.
To participate, contact the Project Leader: Adolfo R. Llanos, MD
Project Title:
Improving Vaccination Rates in Premature Infant in a Freestanding Children’s Hospital
Project Expiration Date: May 31, 2019
Approving Board: ABP
Project Description:
The AAP/CDC guidelines recommend that at 60 days of age, infants should receive diphtheria and tetanus toxoids and acellular pertussis (DTaP) vaccine, Haemophilus influenza type b (Hib) vaccine, inactivated polio vaccine (IPV), and hepatitis B virus (HBV) vaccine. The first dose of HBV vaccine is dependent on infant birth weight (BW) and maternal hepatitis B surface antigen (HBsAg) status. Only monovalent hepatitis B vaccine should be used for PT or FT younger than 6 weeks. Administration of a total of 4 doses of hepatitis B vaccine is permitted when a combination vaccine containing hepatitis B vaccine is administered after the birth dose. Because all preterm infants are considered at increased risk of complications of influenza, 2 doses of inactivated influenza vaccine, administered 1 month apart, should be offered for all preterm infants beginning at 6 months of chronologic age as soon as influenza vaccine is available. (Saari, & the Committee of Infectious Disease, 2003; Schillie et al, MMWR 2018; AAP Committee on infectious Disease Red Book, 2018). Suboptimal immunization rates in NICU graduates has been widely reported in the literature. Delayed or non-immunization during hospitalization has been also related to an increased risk for delayed immunizations after discharge. Children who are under immunized at 2 months of age are more likely to remain under immunized at 6 months, 24 months, and 36 mont1 of age. (Macintosh et al. 2017). Improving vaccination rates in NICU setting is a complex process requiring a multidisciplinary approach. A quality improvement (QI) project could be helpful in identifying and overcoming barriers related to real-time recognition of vaccine eligibility, addressing clinician’s perceptions of side effect associated to vaccine, and use of information technology and innovative solutions to improve care. This QI project aims to improve immunization rates in the NICU at Nicklaus Children’s Hospital (NCH NICU). Process and outcome measures will be assessed after various interventions targeting barriers. This pilot targets patients cared by pediatric residents and excluded admission from the emergency department.
Completion Criteria:
To be eligible for credit, physicians must have substantial participation in key activities of the projects from reviewing data, to interventions, or to measurement of outcomes.
To participate, contact the Project Leader: Alejandro Frade Garcia, MD
Project Title:
Improving Time to Antibiotic Administration in Patients with Fever and Neutropenia in the Emergency Department
Project Expiration Date: November 30, 2016
Approving Board: ABP
Project Description:
Patients with fever and neutropenia are at a high risk of developing sever life-threatening infections. Studies have shown that administration of IV antibiotics within one hour of arrival to the ED can potentially abrogate this serious event. Our initial impression was that this was not achieved at our institution due to multiple barriers. In fact our baseline data showed only 3% compliance (97% non-compliance). The aim of this project is to decrease the time to antibiotic (IV) administration in patients with fever and neutropenia presenting to the ED to < 60 minutes and lower the rate of non-compliance by 50% from baseline by tracking the rate Q 3 months for 2 years. This was achieved through multiple stakeholders and interventions including: ER flow, EMR Power Plan, Pharmacy, IV Team, Physicians, Nursing, and ER staff. Project completed with increase in compliance rates. Process was hard-wired into the ED Flow.
Completion Criteria:
Completing 2 cycles, participation in data review, interventions, and / or process implementation.
To participate, contact the Project Leader: Kamar Godder, MD
Project Title:
Work Flow Analysis and Efficiency in a Pediatric Cardiac Intensive Care Unit
Project Expiration Date: January 15, 2016
Approving Board: ABP
Project Description:
The following interventions were implemented Cycle 1: After recording the time spent rounding on each patient for a few weeks, (Baseline data), all stakeholders were gathered for a brainstorming session to decide what items needed to be covered for every patient admitted to the CICU (during and before rounds) and round flow was standardized step-by-step. Intervention 1: Agreeing on the standard process/steps - Then, team members and intensivists realized that there are inputs that were upstream to the Contributors to Quality, which could not be captured by these flow sheets, but that still needed to be addressed to help reduce to a minimum the variation in rounds. Factors were listed Intervention 2: Education & following/adoption of the standard steps: Individual Patient Encounter Work Flow Sheet (Tool Designed) & Daily Rounds Flow Sheet (Tool for Rounds and Pre-Rounds Designed)
Completion Criteria:
To qualify for Credit completion, team members should have contributed to the QI project through attending the educational sessions, team meetings, reviewing the data, implementation of the tools, and revising the tool as needed.
To participate, contact the Project Leader: Darline Santana-Acosta, MD
Project Title:
Initiative to Decrease Length of Stay in the Emergency Department for Patients with Orthopedic Injuries
Project Expiration Date: November 30, 2018
Approving Board: ABP
Project Description:
Implementation of a nursing initiative where a trained group of nurses will place appropriate X-Ray orders for patients with orthopedic injuries before the physician sees the patient. Nurses will have a didactic instruction on orthopedic injuries and will see and examine at least one patient per type of injury. Once checked off by a physician, they will be able to order X-rays.
Completion Criteria:
Participating physicians will complete the project and obtain credit if they: 1) Actively participate in implementation of the intervention(s) - education/ training 2) Collect and/or analyze and review data
To participate, contact the Project Leader: David A. Lowe, MD
Project Title:
Maximizing ED Communication for Ensuring Safe Transition for Admitted Patients to the Floor
Project Expiration Date: October 1, 2018
Approving Board: ABP
Project Description:
Admitted emergency department patients are sometimes sent to the floor by nursing without the knowledge of the treating emergency department physician. Nursing priorities include transferring patients to the floor as soon as a bed is assigned to the patient and this sometimes supersedes appropriate communication between emergency department physicians and nurses. This project aims at improving communication. Through the implementation of a check mark in the electronic medical record to be completed by the physician. This checkmark verifies that the physician is okay with the patient being sent to the floor. Monthly reminders will be given to nurses at their meetings. Physicians working in the ED will be provided with daily reminders to complete the checkmark. The SMART aim includes: Within 6 months 90% of admitted patients will be approved by the treating physician before being sent to the floor by the nurse.
Completion Criteria:
Physicians are eligible for credit if they: 1) Participate in the implementation of the intervention related to the project 2) Actively participated in data collection and/or review and analysis.
To participate, contact the Project Leader: David A. Lowe, MD
Project Title:
End of Life Palliative Care in Oncology Patients with Non-Curative Cancer
Project Expiration Date: June 30, 2018
Approving Board: ABP
Project Description:
The aim of this project would be to involve end of life palliative care upon identification of patients with terminal or advanced cancer, encourage discussions about end of life care and decrease the incidence of ICU deaths in this population in the hopes to reduce aggressive interventions that may not provide reasonable benefit to patient. This is achieved through the planned steps: Development of a screening tool: Using various screening tools that are published or obtained from other hospitals we have reviewed and developed our own screening tool. The screening tool is enclosed. Development of a palliative care consultation form: With inputs from various physicians and palliative care team members we have developed a palliative care consultation form. Involvement of palliative care team nurse: Changes included early consultation with palliative ARNP and referrals on 6T floor admissions by resident scoring system and notifying MD whether palliative consult needed. Periodic education of residents rotating through 6T and 3T (PICU): PL3 and the Chief Pediatric Resident involved in this improvement project have prepared educational materials and have provided education every block with new residents arriving for the rotation in 6T and 3T. Additional educational sessions were conducted when the compliance was lower. Educational material is included. Education of oncology attendings: We have improved awareness of the aim of the project among oncology faculty through presentations in their Division Meetings. In addition, we have presented monthly updates on the progress of the project in their meetings. Presentation of data and education to PICU attending: We have presented periodic updates on the progress of the project in the Critical Care Division faculty meetings.
Completion Criteria:
Completion criteria include physician involvement in the project for 6-12 months as a team participant in either screening, implementation, or review and providing input on the project results.
To participate, contact the Project Leader: Balagangadhar R. Totapally, MB, BS
Project Title:
Depression Screening in Adolescents with Type 1 Diabetes Mellitus
Project Expiration Date: June 1, 2018
Approving Board: ABP
Project Description:
Patients with diabetes mellitus are at increased risk for depressive symptoms and disorders, particularly female patients. About 1 in 4 patients with diabetes suffer from depression. Therefore, there is a consensus on the need for periodic screening for depression in this population. At the same time, it appears that integrating mental and physical health care may improve outcomes. It was noted that formal mental health screening was not part of the visit for diabetic patients. This project aimed at increasing (to >90%) the rates of mental health screening using a validated Quality of Life tool PHQ-9 of adolescents with Type 1 DM and consequently increase mental health referrals to >90% of those who screen positive. Interventions included Education of providers, automated text in EMR for documentation , email reminder to staff. The project was peer-reviewed and accepted for presentation as a poster at the AAP Florida Chapter Annual meeting.
Completion Criteria:
Attend QI Team meetings, participate in data collection, review or intervention.
To participate, contact the Project Leader: Alfonso Hoyos Martinez, MD
Project Title:
Increasing Meningococcal Booster Vaccination in a Primary Care Practice: A Quality Improvement Initiative
Project Expiration Date: May 28, 2018
Approving Board: ABP
Project Description:
Age appropriate MCV#2 (booster) vaccination rates (68%) in the pediatric care clinic are noted to be well below our MCV#1 vaccination rates (94%) resulting in missed doses of MCV#2 vaccinations. This is due to incomplete EMR vaccination schedule and decreased awareness of vaccination recommendations. The aim of this project is to increase the rate of MCV#2 booster vaccination for 16-17 year old patients in our pediatric care clinic with a goal to match our MCV#1 vaccination rates over the course of 1 year. The poster was presented at the Annual Scholarship Day (peer-reviewed) and at the Florida AAP Chapter annual meeting (Peer-reviewed)
Completion Criteria:
Participation in implementation of the interventions, data review or analysis. Attends QI team meetings.
To participate, contact the Project Leader: Raphael Sturm, MD
Project Title:
Pediatric Residents' Knowledge and Proficiency of Epinephrine Auto-injector Administration and Handling: A QI Project
Project Expiration Date: May 31, 2017
Approving Board: ABP
Project Description:
Patients diagnosed with anaphylaxis are often discharged from the hospital with prescriptions for epinephrine autoinjectors (EAI). The purpose of this study was to evaluate the baseline knowledge of pediatric residents regarding proper handling and administration of EAI, and to assess their knowledge after providing them with a formal one-on-one training at the time of discharge. Since education among providers and patients is needed, we believe that efforts to improve the correct use of EAI among providers responsible for training is an essential component to ensuring that patients and families receive the most accurate guidance on how to use this life saving device. The goal of this project is: To increase the percentage of residents who are confident in how to properly use and care for an Epinephrine auto-injector from baseline to 70% or higher over a 3 week period All residents participating on the study will receive one-on-one education by Allergy and Immunology Fellow of the proper administration and handling of Epinephrine autoinjector. Materials and tools Used: Attached can be found the training tool (questionnaire) used for measuring resident’s knowledge on the proper use and handling of epinephrine autoinjector.
Completion Criteria:
Completing of 2 cycles, Participation in meetings, review of the data or implementation of the plan.
To participate, contact the Project Leader: Hanadys Ale, MD
Project Title:
Decreasing Empiric Use of Vancomycin in Late Onset Sepsis
Project Expiration Date: March 30, 2017
Approving Board: ABP
Project Description:
Starting in the 3rd week of October 2016, we educated residents on unit guidelines for LOS at the onset of the NICU rotation and implemented a LOS checklist to assess provider behaviors in the evaluation and treatment of episodes of suspected LOS (see attached checklist and guidelines). The lead resident in the project met with each group of residents at the beginning of their NICU rotation to explain the importance of adherence to LOS guidelines, including the limited indications for the use of vancomycin as well as the adverse effects associated with the overuse of this antibiotic. We then explained the methodology of data collection including the indications to fill out a LOS checklist and where to find it and return it. We engaged the residents by providing reminders in their workstations to fill out the checklist for cases of suspected LOS (stickers on the computers). The residents would then be prompted to bring the checklist to rounds, thus prompting a discussion with the attending about appropriate evaluation for LOS and the choice and duration of antibiotic treatment. The checklist included an area that had to be filled out 48 hours after initiating antibiotics, thus prompting the resident to discuss with the attending if it was appropriate to continue antibiotic treatment depending on whether or not there was a microbial indication.
Completion Criteria:
Completing of 2 cycles, Participation in meetings, review of the data or implementation of the plan.
To participate, contact the Project Leader: Jessica Barreto, MD
Project Title:
Decreasing Antibiotics Use by Standardizing Diagnosis and Management of Ventilator Associated Infection in the NICU
Project Expiration Date: May 31, 2019
Approving Board: ABP
Project Description:
We will target activities related to the primary drivers “hospital ASP and ID consultant participation” and improving “adherence to unit guidelines”.
- Intervention 1: Develop algorithms for diagnosis and management of VAI The existing literature does not offer specific criteria for the diagnosis and management of VAI in the newborn period. Diagnosis of VAP is based on the definition provided by the Center of Disease Control for infant <1 year, which requires a combination of radiologic, clinical and laboratory criteria. Additionally, we developed an algorithm for the management of infant with suspected VAI adapted from the “Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-Associated Pneumonia” created by the American Thoracic Society Documents.
- Intervention 2: Education and discussion of algorithm with staff. Conduct an educational campaign with the nursing staff, residents and attending physicians on the appropriate diagnosis and treatment of ventilator associated infection following the developed diagnosis criteria and management algorithm. The educational objective will highlight the difficulties.
- Intervention 3: Implementation of Guidelines We will use the checklist that was developed in October of 2016 for the iNICQ project. The checklist was modified to evaluate if the presence of a prior ETA positive culture was included in the decision of selecting the empiric antibiotic treatment for infant with VAI.
Completion Criteria:
We anticipate conducting a minimum of 6 PDSA cycles during the 6-months period starting July 1st 2017. Completion Criteria include: - Participation in one of more of the interventions - Attendance of QI meetings to review data and provide feedback - Educating staff and fellows re. the interventions and its tools/checklists/ criteria.
To participate, contact the Project Leader: Adolfo R. Llanos, MD
Project Title:
Improving Accuracy of Location of Peripherally Inserted Central Venous Catheters Using a Tip Locating System (TLS) During Placement
Project Expiration Date: May 31, 2019
Approving Board: ABP
Project Description:
Studies in adults and adolescents of Peripherally Inserted Central Catheters (PICC) found a right atrial malposition rate of 18% and other malpositions at 13.4%. in pediatrics, correction of these malpositions is a time consuming process and involves discomfort to the family and patient. Additional time is needed by the bedside and PICC nurses, ordering physicians, radiology techs and radiologists. Furthermore, additional healthcare supplies are used which leads to increased waste and costs. The PICC line tip termination point is determined by external measures on the patient body (estimates) rather than real time tip location devices during PICC insertion. The aim of the project is to evaluate and compare the rate of malpositioned PICCs on the first attempt after introduction of an Ultrasound-guided Tip Locating System (TLS) compared to the baseline data gathered before its use.
To participate, contact the Project Leader: Dr. Michael Leoncio
Project Title:
Decreasing the Oversuse of CXR in Children (3y-18y) with Uncomplicated Asthma
Project Expiration Date: June 30, 2018
Approving Board: ABP
Project Description:
Preliminary data from 2016 show that there is overutilization of CXR in the Nicklaus Children’s Hospital Emergency Department (ED) and Urgent Care Centers (UCCs). The numbers of ordered CXR in cases of uncomplicated asthma are significantly higher than the national benchmark. This leads to increased exposure of children to unnecessary radiation and increased cost of care. Despite the presence of Asthma national Guidelines, there is lack of adherence to the guidelines. This could be due to multiple factors including: (1) Lack of education of providers (2) Perceived expectations of parents by the providers and (3) other historic practice patterns (4) Fear of missing diagnosis (5) Fear of litigation. This project aims at decreasing the number of CXR ordered for children with uncomplicated asthma.
To participate, contact the Project Leader: Dr. Mario Reyes
Project Title:
Decreasing the Oversuse of CXR in Young Children (1m - 1 y) with Uncomplicated Bronchiolitis
Project Expiration Date: June 30, 2018
Approving Board: ABP
Project Description:
Preliminary data from 2016 show that there is overutilization of CXR in the Nicklaus Children’s Hospital Emergency Department (ED) and Urgent Care Centers (UCCs). The numbers of ordered CXR in cases of uncomplicated bronchiolitis are significantly higher than the national benchmark. This leads to increased exposure of children to unnecessary radiation and increased cost of care. Despite the presence of new AAP Bronchiolitis Guidelines since 2015, there is lack of adherence to the guidelines. This could be due to multiple factors including: (1) Lack of education of providers (2) Perceived expectations of parents by the providers and (3) other historic practice patterns (4) Fear of missing diagnosis (5) Fear of litigation . The aim of this project is to decrease the number of CXR ordered in patients with uncomplicated bronchiolitis between 1m-1year of age. This project is only opened to hospital physicians staff.
To participate, contact the Project Leader: Dr. Mario Reyes
Project Title:
Improving Documentation of Newborn Screen in a Free Standing NICU
Project Expiration Date: December 31, 2015
Approving Board: ABP
Project Description:
Newborn Screening (NBS) is a highly successful public health program that requires timely confirmatory testing, diagnosis, and clinical management so that optimal long-term outcomes can be achieved. NICU population represents a challenge for the eddcative implementation of NBS. Contrary to infants admitted to the regular newborn nursery, who are born healthy, full-term and > 2500g; infants admitted to the NICU are sick and/or premature and/or low birth weight with a prolonged hospital stay. The interventions routinely used in these settings such as blood transfusions, NPO, and TPN solutions have the potential to affect the NBS results and may lead to delay in diagnosis and clinical management. Our analysis of NBS documentation in the NICU in January 2015 revealed a 35% rate of documentation of NBS obtained during hospitalization. The aim of thsi project is to improve the NBS documentation in the NICU to 90% over the next 12 months.
To participate, contact the Project Leader: Dr. Magaly Diaz-Barbosa
Project Title:
Improvement in the Safe and Efficient Management of Acute Scrotal/Testicular Pain
Project Expiration Date: December 31, 2017
Approving Board: ABP
Project Description:
Delays in the definitive diagnosis of testicular torsion can lead to poor outcomes and loss of function. All members of the Emergency Department team may not recognize the acute and emergent nature of this condition. Baseline data indicate that there is room for improvement in the time from presentation to the ED until final U/S read and report. The goal of this project is to improve the time required between presentation to Nicklaus Children's Hospital ED and the time of definitive diagnosis for patients presenting with acute scrotal pain to rule out testicular torsion. An institutional standard pathway is created and the project will aim at increasing adherence to the standard pathway.
To participate, contact the Project Leader: Dr. Jefry Biehler
Project Title:
Severe Sepsis Bundle Implementation at Nicklaus Children’s Hospital
Project Expiration Date: May 31, 2019
Approving Board: ABP
Project Description:
Sepsis is a dangerous systemic infection that often leads to poor patient outcomes, including mortality. Severe sepsis is a significant problem among acutely ill children. A bundle for recognition, initiation and continuation of treatment of severe sepsis based on national guidelines has been created at Nicklaus Children's Hospital but not yet implemented. The goal of the project is to Implement severe sepsis bundle at Nicklaus Children's Hospital thereby improve sepsis-related outcomes.
To participate, contact the Project Leader: Dr. Bala Totapally
Forms & Resources
Internal Review Committee (IRC)
The Internal Review Committee (IRC) is comprised of physicians (General Pediatrics & Subspecialists), representatives from hospital leadership, Quality Department, Nursing, the Lean Office, the Research Institute, and Information Technology.
The role of the IRC
- Review applications submitted by Project Leaders for original QI projects for feasibility
- Approve Project Leaders' Applications against ABP Standard Checklist
- Review Individual Physician Project Participation Requests that are approved by the Project Leaders and submitted to the IRC
- Receive periodic updates from the Project Leaders on the status of approved projects
Nicklaus Children's Hospital Portfolio Sponsor Program IRC Chair Responsibilities
- Ensuring projects follow ABP standards throughout the planning and project implementation period
- Reviewing projects to determine the strength of QI (ie, Does the project know what they are trying to improve [QI aim statement], do the measures provide information to participants about whether or not they are seeing an improvement, and do the measures relate back to the QI aim)? Work with groups to develop sound QI protocols. Provide feedback to applicants project leaders to improve their proposals.
- Serving as an appeal process for unresolved disputes with attestations.
- Signing Project Leader attestation forms, to attest that they met the project leader requirements set forth by the ABP (ie, materially involved in the design and implementation of the project, involved for minimum of 12 months, understands principles of QI).
IRC Members
- Jefry Biehler, MD, MPH - Chair, FIU Dept of Pediatrics - Medical Director of Quality
- Beatriz Cunill-De Sautu, MD - Director, Pediatric Residency Program
- Michael Gagnon, MA, MBA - Manager, Quality, Safety & Innovations
- Rani S Gereige, MD, MPH - Director of Medical Education & DIO; Portfolio Manager; IRC Chair
- Laura M. Hernandez, DNP, ARNP, CPN, FNP-C
- Sharon Larson, RN, LHRM - Administrative Director, Risk, Claims & Insurance Management; Quality, Patient Safety & Innovations
- Jennifer McCafferty-Fernandez, PhD, CHRC, CHPC, CHC, CCEP - Director, Nicklaus Children's Research Institute
- Marcos Mestre, MD - Chief; Division of Pediatric Hospital Medicine
- Jacques Orces, DO - Chief Medical Information Officer
- Jason Stiles - Senior LEAN Process Leader
- Bala Totapally, MD, DCH, MRCP - Fellowship Program Director; Pediatric Critical Care Medicine
- Jessica Williams, PhD, MPH, APHN-BC
QI Coaches
QI Coaches are Physicians nominated by their Division/Specialty to be the "Go-To" person as Project Leaders are designing their QI projects and preparing their applications for submission for MOC part 4 Approval. QI Coaches are trained coaches to fulfill their roles.
Roles and Responsibilities of the QI Coaches
- Attend QI Coaches training sessions
- Keep up to date on all updates from the MOC Part 4 Portfolio Sponsor Program
- Be familiar with the Postfolio Sponsor Process
- Act as a "coach" or mentor for Project Leaders within their own Division/ Specialty to ensure successful application submission process and provide continued mentorship for ongoing and approved projects
QI Coaches Nominated by their Division/Specialty
| Division/Specialty |
QI Coach(es) |
| Adolescent Medicine |
Metee Comkornruecha, MD |
| Gastroenterology |
Alisa Muniz-Crim,MD |
| General Pediatrics |
Jose Rosa-Olivares, MD
Amanda Porro, MD
Gloria Riefkohl, MD |
| Hospitalist |
Veronica Etinger, MD
Melissa Clemente, MD
Claudette Gonzalez, MD |
| Neonatology |
Adolfo Llanos, MD |
| Neurology |
Ian Miller, MD |
| Pediatric Critical Care |
Fernando Beltramo, MD |
Project Guidelines
Physicians Certified by the ABP
The following project guidelines apply to projects with participating physicians who are board certified in General Pediatrics and/or in subspecialties certified by the American Board of Pediatrics:
| Adolescent Medicine |
Ped Emergency Med |
Hospitalist |
| Ped Neurology |
All Specialties |
Ped Endocrinology |
| Ped Inf Diseases |
Ped Pulmnology |
Ped Cardiology |
| General Pediatrics |
Medical Toxicology |
Ped Rheumatology |
| Child Abuse Peds |
Ped Gastroenterology |
Neo-Perinatal Med |
| Sleep Medicine |
Ped Critical Care |
Ped Hem/Onc |
| Ped Nephrology |
Sports Medicine |
Devel & Behav Peds |
| Hospice & Palliative Care |
Neurodevel Disabilities |
Transplant Hepatology |
Please note, each project is worth
25 points towards MOC Part IV. Recertification for MOC requires >25 points, so you will likely have to complete more than one project during your 5 year cycle to meet ABP requirements.
Physicians Certified by the ABMS
Relationship of Portfolio Program Participation and Member Board Recognition for MOC Part IV Improvement in Medical Practice
| Anesthesiology |
Traditional MOCA: 1 Part IV Case Evaluation
MOCA 2.0: Up to 20 Part II Points for Participants
MOCA 2.0: Up to 25 Part II Points for Leaders |
| Dermatology |
1 Part IV practice assessment QI module |
| Emergency Medicine |
1 patient care practice improvement activity |
| Family Medicine |
1 module or 20 points depending on certification year |
| Internal Medicine |
20 Practice Assessment points |
| Medical Genetics and Genomics |
1 clinical practice module |
| Obstetrics and Gynecology |
1 Part IV assignment (max allowed per calendar year) |
| Ophthalmology |
1 practice performance module |
| Orthopaedic Surgery |
1 Performance in Practice (PIP) Clinical Module (10 SAE credits).
1 PIP feedback module for QI activities involving a patient or peer survey (10 SAE credits) |
| Otolaryngology |
1 performance improvement module |
| Pathology |
1 Part IV activity |
| Pediatrics |
1 Part IV activity or 25 points depending on certification year |
| Physical Medicine and Rehabilitation |
1 practice improvement project |
| Plastic Surgery |
1 Practice Assessment in Plastic Surgery (PA-PS) Tracer Procedure module |
| Preventive Medicine |
1 practice performance assessment |
| Psychiatry and Neurology |
1 Improvement in Medical Practice (PIP) Clinical Module |
| Radiology |
1 Practice Quality Improvement (PQI) project |
| Surgery |
1 quality assessment program or participation in a national, regional, or local outcomes database |
| Thoracic Surgery |
1 activity or quality assessment program |
| Urology |
1 MOC-PS activity |
General Guidelines
To be approved to confer credit for MOC Part 4, a QI project must include the following components:
- Impact on one or more of the Institute of Medicine quality dimensions: safety, effectiveness, timeliness, equity, efficiency, and patient‐centeredness.
- Use of accepted quality improvement methods, including:
- Aim statement (target population, desired numerical improvement, timeframe) S.M.A.R.T. Aim
- Performance measures, collected over time, preferably nationally endorsed; if not, must have documentation of the evidence base, measure specifications, and development process
- At least one balancing measure, to indicate unintended consequences of changes
- Comparison of performance to benchmarks
- Use of a systematic sampling strategy and appropriate sample size
- Include a minimum of 10 data points in each cycle (projects with larger samples [eg, hand hygiene] should use larger sample sizes)
- Systematic implementation of changes
- Use of data for improvement; analysis of measures over time
- At minimum, 1 baseline and 2 follow‐up data cycles
- Reporting data in graphical display over time
- Monitoring data quality – clear measure definitions and adequate data validation
- Regular reporting of project‐wide and physician‐ or practice/unit‐level data to all participants (typically, monthly) and executive leaders/sponsors and other key stakeholders (at least bi‐annually and at project completion)
- Development of physicians’ demonstrated competency in quality improvement methods, by including training and educational resources on QI methods (e.g. seminars by QI experts, coaching by QI consultants, web‐based curriculum)
- A documented organizational structure including a project leader, who is responsible for adjudicating any disputes regarding participation and MOC credit and use of Local Leaders, for multi‐site collaboratives. Also to include institutional governance, specified start date, appropriate staffing and financial support, documented policies and procedures for management of project, system to track physician participation, and HIPAA compliance.
- A process for collecting, reviewing, and signing Attestation Forms, and resolving disputes
- A system to maintain up‐to‐date documentation and retain the documentation for 7 years after the project’s completion (to include project results; methods; participation monitoring, including completion data tracking; local leader acknowledgement forms if applicable)
- Demonstrate improvements in care – score of at least 3.0 (modest process improvements) on the ABP’s Improvement Progress Scale
Physician "Meaningful Participation" Requirements for QI projects approved for MOC Part 4
- Participate during current certificate period or MOC cycle
- Plays an active role in the project over an appropriate period of time.
- Active role means that the pediatrician must:
- Provide direct or consultative care to patients as part of the QI project.
- Be intellectually engaged in planning and executing the project.
- Implement the project’s interventions (the changes designed to improve care)
- Collect, submit and review data in keeping with the project’s measurement plan.
- Collaborate actively by attending at least four project meetings.
- Appropriate Period of participation means:
- ABP looks at the project leader to set requirements for length of participation based on the nature and needs fo the project
- Most MOC approved projects have required 6-12 months of participation
Project Leader's Responsibilities
- Designing a project that addresses the above components for MOC Part 4
- Determining if the project is research and obtaining appropriate IRB approval if it is
- Completing and submitting an Project Leader MOC Application form to the Part 4 Portfolio IRC
- Establish a process to work with Nickluas Childrens Hospital Portfolio Sponsor IRC (Internal Review Committee) to provide oversight to the project
- On Approved Projects:
- Provide feedback data reports to the physician participants on a regular basis
- Collect and retain Local Leader Acknowledgement Forms if appropriate
- Attest for physician participants by signing their Attestation Forms; and handle any disputes that arise in the attestation process
- Send physician completion data to the Nicklaus Childrens Hospital MOC Manager (Dr. Gereige)
- Complete the reports associated with project approval including bi-annual reports that will be reviewed by the IRC, a final report at the close of a project; and, if selected by the ABP for an annual review, an annual report.
Portfolio Sponsor Institutional Responsibility on Approved Projects
- Creating a system to track and monitor physician participation; monitor physician participation to ensure the above standards are met
- Maintaining all project documentation for 7 years (including methods, results, participation, and leadership)
Download the Nicklaus Children's Hospital MOC 4 Portfolio Sponsor Flyer
Financial Assistance Program
Our Mission is to inspire hope and promote lifelong health by providing the best care to every child. As part of our mission, it is of upmost importance to help those in need. We provide gratuitous care to patients who do not have insurance and meet requirements for our financial assistance program.
Financial Assistance Policy Summary
The Nicklaus Children’s Hospital Financial Assistance Policy was established in order to identify and assist patients who lack the financial resources to meet all or part of their financial liability for services rendered and to determine their eligibility for financial assistance. This is a summary of the Financial Assistance Policy.
The Financial Assistance Policy assures that patients who are unable to pay hospital charges are evaluated for financial assistance eligibility on a nondiscriminatory basis. The policy is consistent with the mission and values of Nicklaus Children’s Hospital and takes into account each patient’s ability to pay the cost of his or her care. Nicklaus Children’s Hospital is committed to ensuring
a financially sound organization so that it may continue to provide outstanding medical care with a highly skilled work force employing the latest advances.
Patient Eligibility and Discounts Offered
Patients will be considered for 100 percent financial assistance if their family income for the past 12 months is 200 percent or less of the federal poverty guidelines. Patients will also be considered for 100 percent financial assistance if the patient’s combined responsibility for hospital and/or affiliated physician services from a single episode of care exceed 25 percent of annual family income. All attempts at insurance reimbursement must be exhausted before financial assistance eligibility can be considered. Certain geographical residence requirements may apply. No patient eligible for financial assistance will be charged more for emergency or other medically necessary care than the amounts generally billed to individuals who have insurance coverage.
The criteria for determining financial assistance eligibility is reviewed annually by Nicklaus Children's Health System.
What services are eligible for financial assistance?
- The Financial Assistance Policy applies to charges for emergency or other medically necessary services provided by Nicklaus Children’s Hospital (and its affiliated physicians), and at all Nicklaus Children’s ambulatory care centers. Elective services are not eligible.
Other Governmental Programs Available
Florida KidCare offers healthcare coverage for children under the age of 19 who qualify. Applications are accepted all year long! Learn more today.
Financial Application Process and Forms
Nicklaus Children’s Health System is committed to providing charitable care to those in need. The Financial Assistance program provides assistance to uninsured patients for medically necessary health care services. It applies only to facility charges and employed physician charges. The policy does not apply to private-practicing physician charges or other independent company billings.
Your eligibility is based on your household income and other resources. The Financial Evaluation & Request for Financial Assistance must be completed in its entirety so that we may determine if you are eligible for assistance. We are happy to assist you with the application process.
In order to process your application, photocopies of one of the following documents are required for every member of your household. Your application will not be reviewed until this documentation is submitted.
- W-2 withholding forms (most recent).
- Paycheck stubs (dated within the last 60 days).
- Income tax returns (for most recent year).
- Forms approving or denying unemployment compensation or workers’ compensation (dated within the last 12 months).
- A written verification of wages from employer (dated within the last 60 days).
- A written verification from public welfare agencies or governmental agency which can attest to the income status for the past 12 months.
Also required are photocopies of the following proof of identification and address.
- Valid photo identification
- Proof of current address
Application Documents
- Financial Assistance Policy | Spanish | Creole
- List of Providers (Attachment B)
- Financial Evaluation Application (Attachment C)
- Financial Assistance Policy Summary
The completed application and supporting documentation should be mailed to:
Nicklaus Children's Hospital
ATTN: PFS - Public Benetfits
3100 SW 62 Avenue
Miami, Florida 33155
Press Releases
Conditions We Treat
Pediatric Conditions We Treat
Health Information Library
Search
Registration Documents
At Nicklaus Children's, we understand that a trip to the hospital can be an emotional, and sometimes worrisome, experience for parents and their children. To make your registration a quicker and smoother process we have developed Rapid Registration. Rapid Registration is an initiative established in order to minimize the steps involved during your visit to Nicklaus Children's Hospital by gathering all the needed items prior to your appointment date. If the patient qualifies, you will be receiving a call from one of our dedicated Rapid Registration team members who will verify your demographic information, explain your insurance benefits along with any responsibilities due at time of service.
Below are helpful links with additional information.
Parking and Entrance to the Hospital
Documents and Forms
Registration Documents
At Nicklaus Children's, we understand that a trip to the hospital can be an emotional, and sometimes worrisome, experience for parents and their children. To make your registration a quicker and smoother process we have developed Rapid Registration. Rapid Registration is an initiative established in order to minimize the steps involved during your visit to Nicklaus Children's Hospital by gathering all the needed items prior to your appointment date. If the patient qualifies, you will be receiving a call from one of our dedicated Rapid Registration team members who will verify your demographic information, explain your insurance benefits along with any responsibilities due at time of service.
Below are helpful links with additional information.
Parking and Entrance to the Hospital
Documents and Forms
robots.txt
MEC Login
StartHere
Additional Resources
Adult Application
Adult Volunteer Applicant Requirements
Adult volunteers agree to a minimum commitment agreement as stated below.
Volunteer hours will be verified and signed off only once the minimum commitment is fulfilled.
Time Commitment
- Fulfill a SIX-MONTH and 80-HOUR MINIMUM COMMITMENT
- Volunteer once a week for a scheduled 3-hour shift
- Two absences are allowed every three months
Application Procedure
You will apply using the link above. Please upload your immunization records into our volunteer portal.
- MMR vaccines (two doses, or titers showing immunity)
- Varicella vaccines (two doses, disease year documented, or titers showing immunity)
- Tdap vaccine
- PPD skin test or TB Quantiferon
- Flu vaccine required during season
- All vaccinations are fully required to volunteer.
Orientation & Training
An online orientation will be required, which will provide further details on the volunteer program, policies, and rules. Additional assignment-specific training may be required.
Interview
Applicants will be interviewed after completing the online volunteer orientation. The purpose of the interview is to introduce the applicant to the Volunteer Resources staff, and to discuss schedules, position availability, and applicant skills, experience, and interest. Acceptance into the program is decided at that time, as well as the volunteer assignment and schedule. Volunteer assignments and schedules are not guaranteed and are based on availability and the outcome of the interview.
Background Check
A social security number is required to complete an online criminal background check at the interview. If you do not have a social security number, please contact Volunteer Resources at volunteer.resources@nicklaushealth.org.
Teen Application
Our High School Program is now closed. Please check back frequently for updates on the next application cycle.
Application Procedure
When the teen program application is open, please email your completed application as one PDF document to volunteer.resources@nicklaushealth.org.
A confirmation email will be sent once all documents have been received.
Required documents to be submitted with application in PDF format:
- Immunization records for:
- MMR vaccines (two doses, or titers showing immunity)
- Varicella vaccines (two doses, disease year documented, or titers showing immunity)
- Tdap vaccine
- PPD skin test or TB Quantiferon
- Flu vaccine required during season
- All vaccinations are fully required to volunteer.
- Most recent report card (all academic and conduct grades must be a B or better to be eligible for the program)
- Copy of birth certificate or proof of age (14 year old minimum requirement)
NOTE: Due to the high level of applications we receive, we cannot guarantee acceptance. Qualified applications are received on a first-come, first-serve basis until capacity is reached.
Verification of Hours
Volunteer hours will be verified and signed off only once the minimum commitment is fulfilled.
Orientation & Training
An online orientation will be required, which will provide further details on the volunteer program, policies, and rules. Additional assignment-specific training may be required.
Interview
Applicants will be interviewed after completing the online volunteer orientation. The purpose of the interview is to introduce the applicant to the Volunteer Resources staff, and to discuss schedules, position availability, and applicant skills, experience, and interest. Acceptance into the program is decided at that time, as well as the volunteer assignment and schedule. Volunteer assignments and schedules are not guaranteed and are based on availability and the outcome of the interview.
KidsCrownAwards
Sports Medicine Newsletter
We are eager to share our Sports Health newsletter. This piece is designed to provide patients and families with an overview of the latest sports medicine news, research studies, and injury prevention tips.
paul-evans-general-pediatrics
nazly-montano-general-pediatrics
vinay-bhatia-radiology-house-officer
maria-medina-capote-general-pediatrics
rafael-cardenas-rapid-care-center
alan-swartz-general-pediatrics
jesus-negrette-general-pediatrics
juan-martinez-jr-general-pediatrics
rebecca-lenard-pediatric-dentistry
richard-zakheim-cardiology
Heart Institute News
Patient Forms
English Forms
Spanish Forms
Patient Stories
US News & World Report
Camps
Contracted Partners and Physician Groups
The hospital contracts with non-employed physician groups to provide pathology and neonatology services. These groups will bill insurance and patients separately for any services they perform:
PICU
Wolfsdorf, Raszynski and Sussmane PA
Children's Critical Care Specialists
Contact - 305-662-2639
Pathology
MCH Pathologists, PA
Contact - Med Receivables 305-503-6320
Neonatology
Kidz Medical
Contact – Calev Jimenez 305-661-1515
South Dade Neonatology
Contact – Heidi Quintero 305-441-7179
 Nicklaus Children's Pediatric Specialists
Nicklaus Children's Pediatric Specialists
Pediatric specialties employed by Nicklaus Children's Pediatric Specialists (NCPS), a physician group practice that is part of Nicklaus Children's Health System, will bill insurance and patients separately for any services they perform. NCPS accepts the same insurance plans Nicklaus Children's Hospital accepts.
Pay Your Bill
Patients at Nicklaus Children’s Hospital may receive separate bills for services provided by the health care team. Whether as part of a hospital stay, emergency care, or doctor’s office visit more than one bill may be sent based on the date and the type of service.
For your convenience, we offer several methods for paying your bill. Payments can be made online, in person, or over the phone. The service areas you may receive a bill from are listed below.
Chat with a Billing Representative
Billing of Other Services
Payment of charges that are not covered by the patient's insurance carrier (e.g: co-pays and deductibles) are due prior to the time of discharge.
For the convenience of the parent or guardian, the hospital accepts checks, and the following credit cards: Visa, MasterCard, AmericanExpress, Discover.
The following services are not reflected in the hospital statement, these services are billed to the family directly:
- Anesthesiologists
- Pathologists
- Non-employed surgeons
- Private practice physician(s)
Please refer to contracted partners and physician groups for more information.
Financial Assistance
In an effort to assist parents and legal guardians with the financial aspects of a child's hospitalization, Nicklaus Children's Hospital Patient Financial Services Department is available to process billing to insurance carriers when applicable, and explain statements and charges to the financially responsible parties.
Parents or guardians are encouraged to contact the financial counselors from the Patient Financial Services Department during the patient's stay in the hospital to expedite the discharge process.
Learn MorePay Your Bill
Patients at Nicklaus Children’s Hospital may receive separate bills for services provided by the health care team. Whether as part of a hospital stay, emergency care, or doctor’s office visit more than one bill may be sent based on the date and the type of service.
For your convenience, we offer several methods for paying your bill. Payments can be made online, in person, or over the phone. The service areas you may receive a bill from are listed below.
Chat with a Billing Representative
Billing of Other Services
Payment of charges that are not covered by the patient's insurance carrier (e.g: co-pays and deductibles) are due prior to the time of discharge.
For the convenience of the parent or guardian, the hospital accepts checks, and the following credit cards: Visa, MasterCard, AmericanExpress, Discover.
The following services are not reflected in the hospital statement, these services are billed to the family directly:
- Anesthesiologists
- Pathologists
- Non-employed surgeons
- Private practice physician(s)
Please refer to contracted partners and physician groups for more information.
Financial Assistance
In an effort to assist parents and legal guardians with the financial aspects of a child's hospitalization, Nicklaus Children's Hospital Patient Financial Services Department is available to process billing to insurance carriers when applicable, and explain statements and charges to the financially responsible parties.
Parents or guardians are encouraged to contact the financial counselors from the Patient Financial Services Department during the patient's stay in the hospital to expedite the discharge process.
Learn MorePricing and Estimates
Nicklaus Children's Hospital believes you have the right to understand your healthcare options and the cost of care. The prices provided on this website and our facilities are an estimate of charges for most hospital services without complications. There may be variations to prices based on services received (i.e. surgery time) as well as additional supporting areas required (i.e. anesthesia, radiology, etc.). Your final bill will include charges for the actual services provided to you and your financial responsibility. Posted prices are general estimates and do not reflect your personal financial responsibility.
Price Transparency Machine Readable File
The following links contain pricing transparency information for procedures performed at the hospital.
Charge Master (Price Sheets)
The following files contain pricing information for procedures performed at the hospital, urgent care, and outpatient centers.
Request an Estimate
The Corporate Pricing Office (CPO) can provide a patient's estimated financial responsibility. This includes estimates for inpatient care and procedures. Estimates will be provided within 24 hours of receiving the request.
Pricing included in estimates applies to hospital charges only; some provider costs may not be included in this estimate and providers may not be in network. Please contact your health insurance provider to learn more about in-network providers/charges as well as your cost-sharing responsibilities. A lower cost option for a procedure/service can be provided at an urgent care center (UCC) or ambulatory surgery center (ASC).
Nicklaus Children's Health System
{$ NCH.BoilerplateHealthSystem $}
Our vision is to be where the children are. Ultimately, this means being there through all stages of health and life, both physically and emotionally. To be a trusted partner to children and their families, not only in times of illness, but throughout their life journey.
Our mission is to inspire hope and promote lifelong health by providing the best care to every child.
News and Resources
News: Research and Innovation
Diagnostics and Testing
Specialist Programs and Services
Child Life Home
Teleheart2
Community Event Registration
Thank you for your interest in attending a Nicklaus Children's Hospital event, please complete the registration form below.
Thank you
Meet the Pediatric Anesthesiology Team
The Nicklaus Children's Hospital pediatric anesthesia department is staffed with highly-skilled and experienced specialists. Meet the team of pediatric anesthesiologists.
News: Research & Innovation
News
CRM Forms
Videos
Steps to Prepare for Your Child's Surgery
To prepare for your child's surgery at the Kenneth C. Griffin Surgical Tower at Nicklaus Children's Hospital, here is a helpful list of what to expect before, during and after the surgery.
PASSPort: Pre-Admission Surgical Screening
Registration (10 days prior)
- You will receive a text link to the Tonic registration platform, where you will verify your child's information 10 days before the surgery. Please contact the Patient Access Department at 305-663-8410 if you have any questions or issues gaining access to the platform.
Pre-Admission Surgical Screening (PASS) Phone Call (7 days prior)
- A nurse from the PASS team will contact you to review or discuss the child's medical history within 7 days before surgery. If there are any changes in your child's health status (cold, runny nose, etc.) prior to surgery, please contact a PASS nurse as soon as possible by calling 786-624-3404.
Financial Clearance Call (approximately 3 days prior)
- A member of the Pre-Access team will contact you at least 3 days before the surgery to review any financial responsibility and authorizations, if required.
Day Before the Procedure
- The day before the procedure, a member of our Patient Access team will contact you if there are any pending registration documents. Time of arrival and drinking/eating instructions will be sent via text message after 2:30 p.m.
- Diet: Please follow the dietary restrictions instructions for the day before the surgery. If your child does not follow the “no-eating or drinking” instructions as indicated, the surgery will be delayed or cancelled.
Day of Surgery
- ✓ Remember to bring all important documentation including: your child's insurance card, parents'/guardians' identification cards (such as driver's license or passport), and any supporting documents and legal court orders.
- ✓ Add 30 minutes of travel time to account for traffic and parking delays. Patients should have been notified to arrive at least 2 hours prior to their surgery. Please follow the instructions provided in the text message related to the time of arrival.
- ✓ Complimentary valet service is offered 24-hours a day in front of the Central Building (near the Devonshire Boulevard entrance to the campus.) Additional complimentary valet services are available during select hours in the blue and yellow garages.
- ✓ Transportation: Please make sure you have arranged transportation for before and after surgery.
- ✓ Patients 18 years and older must be accompanied by a responsible adult.
- Please make sure your child does not wear:
- Any jewelry (including piercings)
- Contact lenses (bring eyeglasses)
- Make-up and hair accessories
- Hair gel or hairspray
- Nail polish
To help prevent surgical site infections:
- ✓ Bathe with the anti-bacterial soap (such as Hibiclens Antiseptic) as instructed, the evening before surgery. If surgery is scheduled in the afternoon, also bathe the morning of surgery.
- ✓ DO NOT shave surgical site area.
Upon arrival to Nicklaus Children's Hospital, please go straight to the Kenneth C. Griffin Surgical Tower, located near the emergency department, for your surgical check-in and registration. Patients who have completed the expedited registration via text message can visit the electronic kiosk to check-in after obtaining a visitor badge from the security representative. A member of our team will then assist with next steps.
Talking to your child about surgery
Good communication is the best way to prepare your child for a hospital visit. Rather than surprise your child, try to explain the situation in simple terms so that they will understand. This is the best way to earn and keep their trust. Be sure to give your child a chance to ask questions and tell you how they are feeling.
- For infants, the goal is to ensure parents understand the child's medical issues and understand each other's fears and expectations.
- Toddlers are frightened of separation and tend to think that disease and surgery are punishments. They need to be reassured that they are not being punished.
- School-age children may fear anesthesia, pain and even death. They will need reassurance and preparation, including honest answers to their questions.
- For adolescents, empowerment is key. They need to participate in the decision-making process, while still relying on adult support and reassurance. They may not feel it is acceptable to express fear or pain and need to be encouraged to voice their questions and concerns.
Pre-Surgical Orientation with Child Life Department
Our Child Life department is available to help prepare you and your child for what to expect on the day of surgery. It has been noted that patients who participate in this class are more relaxed prior to their surgical procedure. A pre-surgical orientation is available upon request and includes:
- A tour of specific areas to familiarize the patient with the sights and sounds of the hospital
- Helpful information and resources for siblings and parents
- Opportunities to answer questions your child may have about their upcoming hospital experience
The Child Life Pre-Surgical Orientation Program is offered for children ages 3 and up. All attendees must be registered before arrival for the tour.
Steps to Prepare for Your Child's Surgery
To prepare for your child's surgery at the Kenneth C. Griffin Surgical Tower at Nicklaus Children's Hospital, here is a helpful list of what to expect before, during and after the surgery.
PASSPort: Pre-Admission Surgical Screening
Registration (10 days prior)
- You will receive a text link to the Tonic registration platform, where you will verify your child's information 10 days before the surgery. Please contact the Patient Access Department at 305-663-8410 if you have any questions or issues gaining access to the platform.
Pre-Admission Surgical Screening (PASS) Phone Call (7 days prior)
- A nurse from the PASS team will contact you to review or discuss the child's medical history within 7 days before surgery. If there are any changes in your child's health status (cold, runny nose, etc.) prior to surgery, please contact a PASS nurse as soon as possible by calling 786-624-3404.
Financial Clearance Call (approximately 3 days prior)
- A member of the Pre-Access team will contact you at least 3 days before the surgery to review any financial responsibility and authorizations, if required.
Day Before the Procedure
- The day before the procedure, a member of our Patient Access team will contact you if there are any pending registration documents. Time of arrival and drinking/eating instructions will be sent via text message after 2:30 p.m.
- Diet: Please follow the dietary restrictions instructions for the day before the surgery. If your child does not follow the “no-eating or drinking” instructions as indicated, the surgery will be delayed or cancelled.
Day of Surgery
- ✓ Remember to bring all important documentation including: your child's insurance card, parents'/guardians' identification cards (such as driver's license or passport), and any supporting documents and legal court orders.
- ✓ Add 30 minutes of travel time to account for traffic and parking delays. Patients should have been notified to arrive at least 2 hours prior to their surgery. Please follow the instructions provided in the text message related to the time of arrival.
- ✓ Complimentary valet service is offered 24-hours a day in front of the Central Building (near the Devonshire Boulevard entrance to the campus.) Additional complimentary valet services are available during select hours in the blue and yellow garages.
- ✓ Transportation: Please make sure you have arranged transportation for before and after surgery.
- ✓ Patients 18 years and older must be accompanied by a responsible adult.
- Please make sure your child does not wear:
- Any jewelry (including piercings)
- Contact lenses (bring eyeglasses)
- Make-up and hair accessories
- Hair gel or hairspray
- Nail polish
To help prevent surgical site infections:
- ✓ Bathe with the anti-bacterial soap (such as Hibiclens Antiseptic) as instructed, the evening before surgery. If surgery is scheduled in the afternoon, also bathe the morning of surgery.
- ✓ DO NOT shave surgical site area.
Upon arrival to Nicklaus Children's Hospital, please go straight to the Kenneth C. Griffin Surgical Tower, located near the emergency department, for your surgical check-in and registration. Patients who have completed the expedited registration via text message can visit the electronic kiosk to check-in after obtaining a visitor badge from the security representative. A member of our team will then assist with next steps.
Talking to your child about surgery
Good communication is the best way to prepare your child for a hospital visit. Rather than surprise your child, try to explain the situation in simple terms so that they will understand. This is the best way to earn and keep their trust. Be sure to give your child a chance to ask questions and tell you how they are feeling.
- For infants, the goal is to ensure parents understand the child's medical issues and understand each other's fears and expectations.
- Toddlers are frightened of separation and tend to think that disease and surgery are punishments. They need to be reassured that they are not being punished.
- School-age children may fear anesthesia, pain and even death. They will need reassurance and preparation, including honest answers to their questions.
- For adolescents, empowerment is key. They need to participate in the decision-making process, while still relying on adult support and reassurance. They may not feel it is acceptable to express fear or pain and need to be encouraged to voice their questions and concerns.
Pre-Surgical Orientation with Child Life Department
Our Child Life department is available to help prepare you and your child for what to expect on the day of surgery. It has been noted that patients who participate in this class are more relaxed prior to their surgical procedure. A pre-surgical orientation is available upon request and includes:
- A tour of specific areas to familiarize the patient with the sights and sounds of the hospital
- Helpful information and resources for siblings and parents
- Opportunities to answer questions your child may have about their upcoming hospital experience
The Child Life Pre-Surgical Orientation Program is offered for children ages 3 and up. All attendees must be registered before arrival for the tour.
Steps to Prepare for Your Child's Surgery
To prepare for your child's surgery at the Kenneth C. Griffin Surgical Tower at Nicklaus Children's Hospital, here is a helpful list of what to expect before, during and after the surgery.
PASSPort: Pre-Admission Surgical Screening
Registration (10 days prior)
- You will receive a text link to the Tonic registration platform, where you will verify your child's information 10 days before the surgery. Please contact the Patient Access Department at 305-663-8410 if you have any questions or issues gaining access to the platform.
Pre-Admission Surgical Screening (PASS) Phone Call (7 days prior)
- A nurse from the PASS team will contact you to review or discuss the child's medical history within 7 days before surgery. If there are any changes in your child's health status (cold, runny nose, etc.) prior to surgery, please contact a PASS nurse as soon as possible by calling 786-624-3404.
Financial Clearance Call (approximately 3 days prior)
- A member of the Pre-Access team will contact you at least 3 days before the surgery to review any financial responsibility and authorizations, if required.
Day Before the Procedure
- The day before the procedure, a member of our Patient Access team will contact you if there are any pending registration documents. Time of arrival and drinking/eating instructions will be sent via text message after 2:30 p.m.
- Diet: Please follow the dietary restrictions instructions for the day before the surgery. If your child does not follow the “no-eating or drinking” instructions as indicated, the surgery will be delayed or cancelled.
Day of Surgery
- ✓ Remember to bring all important documentation including: your child's insurance card, parents'/guardians' identification cards (such as driver's license or passport), and any supporting documents and legal court orders.
- ✓ Add 30 minutes of travel time to account for traffic and parking delays. Patients should have been notified to arrive at least 2 hours prior to their surgery. Please follow the instructions provided in the text message related to the time of arrival.
- ✓ Complimentary valet service is offered 24-hours a day in front of the Central Building (near the Devonshire Boulevard entrance to the campus.) Additional complimentary valet services are available during select hours in the blue and yellow garages.
- ✓ Transportation: Please make sure you have arranged transportation for before and after surgery.
- ✓ Patients 18 years and older must be accompanied by a responsible adult.
- Please make sure your child does not wear:
- Any jewelry (including piercings)
- Contact lenses (bring eyeglasses)
- Make-up and hair accessories
- Hair gel or hairspray
- Nail polish
To help prevent surgical site infections:
- ✓ Bathe with the anti-bacterial soap (such as Hibiclens Antiseptic) as instructed, the evening before surgery. If surgery is scheduled in the afternoon, also bathe the morning of surgery.
- ✓ DO NOT shave surgical site area.
Upon arrival to Nicklaus Children's Hospital, please go straight to the Kenneth C. Griffin Surgical Tower, located near the emergency department, for your surgical check-in and registration. Patients who have completed the expedited registration via text message can visit the electronic kiosk to check-in after obtaining a visitor badge from the security representative. A member of our team will then assist with next steps.
Talking to your child about surgery
Good communication is the best way to prepare your child for a hospital visit. Rather than surprise your child, try to explain the situation in simple terms so that they will understand. This is the best way to earn and keep their trust. Be sure to give your child a chance to ask questions and tell you how they are feeling.
- For infants, the goal is to ensure parents understand the child's medical issues and understand each other's fears and expectations.
- Toddlers are frightened of separation and tend to think that disease and surgery are punishments. They need to be reassured that they are not being punished.
- School-age children may fear anesthesia, pain and even death. They will need reassurance and preparation, including honest answers to their questions.
- For adolescents, empowerment is key. They need to participate in the decision-making process, while still relying on adult support and reassurance. They may not feel it is acceptable to express fear or pain and need to be encouraged to voice their questions and concerns.
Pre-Surgical Orientation with Child Life Department
Our Child Life department is available to help prepare you and your child for what to expect on the day of surgery. It has been noted that patients who participate in this class are more relaxed prior to their surgical procedure. A pre-surgical orientation is available upon request and includes:
- A tour of specific areas to familiarize the patient with the sights and sounds of the hospital
- Helpful information and resources for siblings and parents
- Opportunities to answer questions your child may have about their upcoming hospital experience
The Child Life Pre-Surgical Orientation Program is offered for children ages 3 and up. All attendees must be registered before arrival for the tour.
STOP Sports Injuries
The STOP Sports Injuries campaign is geared towards providing guidance on healthy and safe athletic participation and should not be considered a replacement for speaking with your physician, athletic trainer or other qualified healthcare provider.
How to Prevent Sports Injuries
Prevention is always the best way to deal with sports injuries. There are several steps you and your children can take for safety's sake.
- For starters, wear sport-specific protective gear. If your son plays football, for example, he'll need a helmet, mouth guard, protective cup, proper footwear and other body pads.
- Another key to preventing sports injuries is to always warm up before practice or a game. Be sure your child's coach includes slow stretching to lengthen players' muscles and increase blood flow.
- To prevent dehydration from the South Florida heat, children also need to take frequent drink breaks (every 15-20 minutes in the hottest months of the year).
STOP Sports Injuries
The STOP Sports Injuries Campaign wants to be sure that you have all the information you need to keep kids in the game for life. Whether you are an athlete, coach, healthcare provider or parent, we have the sports injury prevention tips and tools to make sure safety is your first priority.
There are injuries and issues common to many sports. See our tip sheets on preventing and treating specific athletic injuries and issues.
Help keep kids in the game for life!
Links available in this page are not necessarily endorsed, reviewed, or sponsored by Nicklaus Children's Hospital. By clicking on any of the links, you will be leaving NCH's Website.
To help keep kids in the game for life, STOP Sports Injuries targets the sports that have the highest rates of overuse and trauma injuries.
Check out these helpful sports injury prevention tips that are provided to you by the STOP Sports Injuries campaign (http://www.stopsportsinjuries.org).
Sport Specific Resources
STOP Sports Injuries
The STOP Sports Injuries campaign is geared towards providing guidance on healthy and safe athletic participation and should not be considered a replacement for speaking with your physician, athletic trainer or other qualified healthcare provider.
How to Prevent Sports Injuries
Prevention is always the best way to deal with sports injuries. There are several steps you and your children can take for safety's sake.
- For starters, wear sport-specific protective gear. If your son plays football, for example, he'll need a helmet, mouth guard, protective cup, proper footwear and other body pads.
- Another key to preventing sports injuries is to always warm up before practice or a game. Be sure your child's coach includes slow stretching to lengthen players' muscles and increase blood flow.
- To prevent dehydration from the South Florida heat, children also need to take frequent drink breaks (every 15-20 minutes in the hottest months of the year).
STOP Sports Injuries
The STOP Sports Injuries Campaign wants to be sure that you have all the information you need to keep kids in the game for life. Whether you are an athlete, coach, healthcare provider or parent, we have the sports injury prevention tips and tools to make sure safety is your first priority.
There are injuries and issues common to many sports. See our tip sheets on preventing and treating specific athletic injuries and issues.
Help keep kids in the game for life!
Links available in this page are not necessarily endorsed, reviewed, or sponsored by Nicklaus Children's Hospital. By clicking on any of the links, you will be leaving NCH's Website.
To help keep kids in the game for life, STOP Sports Injuries targets the sports that have the highest rates of overuse and trauma injuries.
Check out these helpful sports injury prevention tips that are provided to you by the STOP Sports Injuries campaign (http://www.stopsportsinjuries.org).
Sport Specific Resources
Parents
Teens
Kids
visitAPCP
Telehealth
Conditions we Treat
Conditions we Treat
Patient Stories
Patient Stories
Videos
Videos
PCICS
Our Healthcare Partners
Baptist Health South Florida
Emergency Department Services
Nicklaus Children's pediatric emergency physicians provide coverage at the Baptist Hospital and Homestead Hospital emergency departments. The doctors you have previously seen and entrusted with your child's care in those two emergency departments transitioned in 2021 to employment by Nicklaus Children's Pediatric Specialists, the medical group practice of Nicklaus Children's. Baptist Health South Florida and Nicklaus Children's shared focus of putting children and families first is a great combination for the families of Miami-Dade County. We are pleased that the physicians in the Baptist Hospital and Homestead emergency departments will continue to offer services to families who have come to know them there, while also engaging with the extensive array of pediatric subspecialists available on Nicklaus' medical staff to support children and families with continuing specialized care needs.
Nicklaus Children's Hospital and Baptist Health South Florida are two of the region's leading healthcare providers, combining clinical and service excellence. “We welcome the Baptist-based pediatric emergency physicians to our Nicklaus Children's family,” said Dr. Marcos Mestre, Vice President and Chief Medical Officer of Nicklaus Children's Hospital.
"As Baptist Health continues to put the healthcare and needs of our patients first, we look forward to our new partnership with Nicklaus Children's Health System. Through this collaboration, you can expect the same high-quality care that you have come to expect from the familiar physicians in the Baptist Pediatric Emergency Department. Our commitment to our pediatric colleagues in the community remains paramount, and we encourage you to communicate directly with us about your patient's needs. Since 1996, you have trusted us with your patients' pediatric emergency needs, and this new relationship will continue to serve our community,” said Dr. Fernando G. Mendoza, Chief of Pediatrics, Medical Director, Baptist Children's Emergency Center.
Inpatient Care Services
Nicklaus Children's Hospital and Baptist Hospital finalized an agreement in April 2020 whereby children receiving care in a Baptist Hospital emergency department who require inpatient admission are transferred to Nicklaus Children's. The agreement helped both organizations adapt as the COVID-19 pandemic surged, enabling Baptist Health to optimize service to the adult population most affected by the pandemic. This partnership stems from the commitment to serve as advocates for the health and wellbeing of the community.
Baptist Hospital and Miami Cancer Institute continue to provide pediatric oncology services on an inpatient and outpatient basis along with other diagnostic, rehabilitation and physician consultation services. Baptist Hospital, Homestead Hospital, South Miami Hospital and West Kendall Baptist Hospital continue to provide neonatal intensive care (NICU) services; and Baptist Hospital, Doctors Hospital, Fishermen's Community Hospital, Homestead Hospital, Mariners Hospital, South Miami Hospital and West Kendall Baptist Hospital continue to see pediatric patients in their emergency rooms. Any pediatric patients seen in the Baptist Health emergency departments in Miami-Dade and Monroe counties requiring hospital admission are transferred to Nicklaus Children's Hospital.
Jupiter Medical Center
As the region's pediatric care leader, Nicklaus Children's is privileged to support colleagues at Jupiter Medical Center in the opening of the new De George Pediatric Unit. The hospital shared policies, procedures, training, competencies, and assisted with selection of equipment and supplies. In addition, Nicklaus Children's supported the development of a child-friendly environment, family-centered operational processes and work flows.
The De George Pediatric Unit is a continuation of a dynamic partnership between Jupiter Medical Center and Nicklaus Children's Hospital, was made possible thanks to an extraordinary gift from the Lawrence J. and Florence A. De George Charitable Trust and the Nicklaus Children's Health Care Foundation.
From newborns and toddlers to adolescents up to age 18, the De George Pediatric Unit is a comprehensive, child-centered environment, featuring advanced medical and therapeutic services. Using the clinical guidelines and staff training developed by Nicklaus Children's Hospital this new facility will serve to advance pediatric care opportunities for families in Palm Beach County.
The De George Pediatric Unit features:
- 12 inpatient pediatric rooms
- Pediatric surgery suites
- Pediatric therapy
- Children's playroom supported by a child life specialist
- Bear's Den for resting, inspired by Jack Nicklaus
Some children may be referred to Nicklaus Children's main campus as needed for some surgical or critical care services. This will be at the discretion of the care team of the De George Pediatric Unit and the patient's family. The care needs and wishes of the child and family are always at the forefront when transfer decisions are made.
Level II De George Neonatal Intensive Care Unit (NICU)
The 16 bed De George Neonatal Intensive Care Unit, made possible through the generosity of the Lawrence J. and Florence A. De George Charitable Trust, is equipped to care for babies born as early as 32 weeks. The unit adheres to policies, procedures, training and competencies shared through the collaboration with Nicklaus Children's. In addition, the unit is staffed around-the-clock by Nicklaus Children's neonatologists, and Nicklaus provides nursing staff oversight.
Features of the unit include:
- Advanced monitoring and technology
- A family lounge
- Treatment rooms
- Two private nesting rooms to foster bonding
- An infant feeding preparation space
Mastroianni Family Pediatric Emergency Department
Jupiter Medical Center and Nicklaus Children's Hospital are making pediatric care even more accessible to residents of Palm Beach and Martin counties with the Mastroianni Family Pediatric Emergency Department. Nicklaus Children's Hospital, the trusted choice for pediatric care in South Florida, continues to share best practices, policies and procedures developed and continuously enhanced over its more than 70 year history.
Experts from both institutions are collaborating to provide world-class pediatric emergency care. The Mastroianni Family Pediatric Emergency Department is a standalone 6,300-square-foot pediatric wing, specifically designed to be a family-focused, child-friendly environment with services/amenities including:
- State-of-the-art Mindray monitoring that communicates with the Electronic Health Record system
- Dedicated pediatric emergency physicians and nurses available 24/7
- Pediatric specific beds and triage rooms
- Child life specialist
- Pediatric paramedics
- Pediatric orthopedic room
- Respiratory therapists trained in pediatrics
- Infant warmer
- Other pediatric subspecialists available
Children will also feel more comfortable and safe with our kid-friendly amenities:
- Interactive light flooring in the waiting room
- Mobile video game systems
- Child-sized furniture
- Remote control cars and little red wagons for transport, if needed
NCH Healthcare System
Visit this partner's website
Nicklaus Children's is collaborating with NCH Healthcare System to provide pediatric medical services at NCH North Naples Hospital with the aim of supporting families in Collier County in receiving top-quality pediatric inpatient care close to home.
Clinicians employed by Nicklaus Children's Pediatric Specialists (NCPS), the physician-led medical group practice of Nicklaus Children's Health System, are staffing inpatient services for the NCH neonatal intensive care unit, pediatric intensive care unit and other pediatric inpatients as well as newborn routine screenings.
The NCH North Naples campus is located at 11190 Health Park Blvd in North Naples.
The BirthPlace NICU
Our 19-bed, Level II Neonatal Intensive Care Unit (NICU) within The BirthPlace is the only neonatal intensive care unit in Collier County. It provides state-of-the-art and compassionate family-centered, developmentally supportive care for premature and ill newborns.
The NICU has 24-hour-a-day board-certified neonatologist coverage (pediatricians who have extra training in taking care of premature and seriously ill newborns) and is staffed with neonatal ICU trained nurses and respiratory therapists. The NCH NICU also features a pediatric pharmacy and pediatric dietary support, along with pediatric occupational therapy services with a certified feeding specialist.
Occupational therapists also provide sensorimotor developmental assessment and intervention and have the capability to follow the babies in our out-patient pediatric rehab clinic.
The NCH NICU also boasts:
- Social service managers to assist you upon discharge.
- Lactation support services are available after your discharge. Breast pumps are located in a private lactation suite within the NICU for your convenience.
- Rooming-in support for parents prior to discharge.
Robert and Marian MacDonald Seacareium
NCPS pediatric intensivists provide care for children receiving intensive care services at NCH's Robert and Marian MacDonald Seacareium. This charming, ocean-themed unit provides care for children hospitalized for a wide range of care needs. The Seacareium features 15 general pediatric rooms and one outpatient room. Four of the general pediatric rooms can be used for progressive care and intensive care. The pediatric unit is equipped with smart room technology, as well as a variety of state-of-the-art equipment to assist in quality care and everyday tasks for our sickest patients.
NCH has served Collier County's children, mothers and families for more than six decades, and proudly provides inpatient and outpatient care for more than 30,000 children annually. NCH is also the only hospital in Collier County offering labor and delivery services and 24-hour pediatric emergency care.
Nursing Scholarships
Nicklaus Children’s Hospital is committed to supporting nursing staff members in meeting individual educational advancement goals. Several scholarships are available to employed nurses who are pursuing advanced training. Scholarships are available for clinical employees who are currently enrolled in a nursing program as well as for RNs seeking a bachelor’s or master’s degree, who are interested in pursuing an online program through West Coast University, one of our nursing education partners.
Why apply to a Nicklaus Children's Hospital Nursing Scholarship?
Scholarships offered through the hospital are granted exclusively to qualified hospital employees. Some scholarships are for online learning programs that are supportive of working nurses in meeting their educational advancement goals.
Who is eligible to apply?
Applicants for the scholarships offered through the hospital must be benefit-eligible employees in good standing of Nicklaus Children’s Hospital and meet the requirements for the individual scholarships.
Available Nursing Scholarships
Bing Wood Scholarship
 The Dr. Maria Lina “Bing Wood Memorial Scholarship Award is sponsored by the Nicklaus Children’s Hospital Nursing Department to promote advanced education within the nursing profession. The scholarship is awarded to current benefit-eligible employees who are enrolled in an accredited nursing program.
The Dr. Maria Lina “Bing Wood Memorial Scholarship Award is sponsored by the Nicklaus Children’s Hospital Nursing Department to promote advanced education within the nursing profession. The scholarship is awarded to current benefit-eligible employees who are enrolled in an accredited nursing program.
Apply for Scholarship
West Coast University Scholarships
The hospital, together with nurse education partner West Coast University, offers a nursing scholarship annually to two West Coast University online learning programs. The scholarships are offered to benefit-eligible registered nurses wishing to attain their advanced degrees in nursing.
Bing Wood Scholarship
The Maria Lina “Bing” Wood Nursing Scholarship and Education Fund was established in honor of Dr. Maria Lina “Bing” Wood, a Nicklaus Children's nurse who embodied a passion for the advancement of nursing education, quality patient care and a culture of safety. Dr. Wood's professionalism, dedication and commitment to life-long learning made her a role model for nurses everywhere.
The fund supports the Dr. Maria Lina “Bing” Wood Memorial Scholarship Award that promotes advanced education within the nursing profession.
Eligibility Criteria
The scholarship is awarded to current benefit-eligible employees who are enrolled in an accredited nursing program. Candidates must:
- Work in a clinical support role or within the nursing department, and be in good standing.
- Maintain employee benefit status, whether full-time or part-time status.
- Hold a current Florida nursing license.
- Have proof of being enrolled in an approved accredited nursing program.
Application Process
- Obtain digital copies of the required documentation.
- Letter of acceptance into the nursing program.
- Two letters of reference.
- Current CV or resume.
- Complete an essay with a minimum of 350 words describing your influence and contributions to the strategic priorities of your unit, department or hospital/system.
- Submit your application and all files via email to Nursing.Scholarships@nicklaushealth.org.
Scholarship Amount
The recipient of the award will receive $2,000 toward his or her educational goals.
Deadline
The deadline for application submission is April 15, 2024.
Pediatric Nursing Courses
BillPay
Successful Online Learning
Able to manage time well, organized, and self-discipline.
- Online courses are convenient and flexible because they usually do not have scheduled class meetings, you must devote as much time for studying, reading, working on assignments, and engaging with peers and the instructor as they would for classroom courses.
- Consciously schedule time to complete the requirements of online course work;
- Are well-organized and can effectively budget time to complete required course learning activities; and
- Know how to "make time" for online course work in their busy lives.
Motivated, proactive, and committed to their learning
- Learning, participation, and engagement in online courses mostly happens asynchronously, which means you, your peers, and your instructor are working on course activities at different times.
- Take responsibility for their work, meeting due dates for required weekly work while preparing for long term assignments, independent research, and collaborative projects.
- Ask questions of the instructor and their peers and inform their instructor of concerns.
- Participate in online discussions and check their course site periodically for updates instructor feedback, and peer interaction.
- Are engaged, motivated, and self-disciplined during the course.
Can communicate well in writing
- Much of the work you do in an online course will require communicating your learning through writing.
- Is comfortable communicating in various forms of writing.
- Express themselves in carefully thought-out worded responses.
- Are able to stay focused on the topic and question in their responses.
- Seek assistance proactively
Have a place to study
- Have a place with enough space for them to work on course activities that is a familiar and comfortable place to retreat to complete online work.
Comfortable Using Technologies
- As an online student some technologies will be familiar to you (like watching internet videos) while other technologies may not (like the course management system, webinar system, or simulations).
- Is comfortable using various kinds of technologies.
- Know how to navigate webpages, open new browser windows, and how to download and upload files and images.
- Know how to use several search engines to locate information, and can install software.
- Know how to find answers to troubleshooting problems by using HELP features, finding contact information, and using searches to find answers to common computer problems.
- Know how to determine the problem and who to contact to get assistance or get it fixed.
Nursing Scholarships Application
Thank You
Success! Your Application has been submitted.
Board Luncheon RSVP
Please fill out the form to confirm your attendance
The Brain Institute
Lunch and Learn Information Sessions
WCU Lunch and Learn Sessions
Join us at one of the Lunch and Learn sesssions to learn more about the scholarships.
2020 Sessions will be announced as deadline dates approach.
Conditions we Treat
VACC Camp
Held each year in Miami during spring break, the Ventilation Assisted Children's Center Camp provides children with tracheostomies (requiring oxygen and ventilators to breathe), along with their families, a week filled with activities such as swimming, boating and bowling regardless of their medical limitations.
The camp activities are all conducted in a medically-safe environment thanks to the help of volunteers and medical personnel from Nicklaus Children’s Hospital who donate their time and services to ensure a safe week for all involved.
The camp is sponsored by Nicklaus Children’s Hospital and is supported by many who donate their time and services to the children of VACC camp. For more information about The Dr. Moises Simpser VACC camp, visit www.vacccamp.com
About the Founder
 Dr. Moises Simpser, pediatric pulmonologist at Nicklaus Children’s Hospital, is the VACC Camp's founder and director; he has led the camp since its inception in 1986. Dr. Simpser has been honored multiple times for his community service and his efforts to improve the quality of life of children afflicted with respiratory conditions.
Dr. Moises Simpser, pediatric pulmonologist at Nicklaus Children’s Hospital, is the VACC Camp's founder and director; he has led the camp since its inception in 1986. Dr. Simpser has been honored multiple times for his community service and his efforts to improve the quality of life of children afflicted with respiratory conditions.
Pricing Estimate Request
By submitting this online form, you are agreeing to the Terms and Conditions of use and the website Privacy Policy.
Thank you
Success! Your Pricing Estimate Request has been submitted.
Estimates are provided within 24 hours of receiving the request.
Please be aware that we read and respond to inquiries only during normal business hours (Monday through Friday, 8:00 a.m. to 5:00 p.m. Eastern Time).
Again, thanks you for choosing us. We wish you well.
Sincerely,
Corporate Pricing Office
Hotel & Lodging Accommodations
Nicklaus Children's Hospital has partnered with Hampton Inn & Suites in Miami and Nuvo Suites in Doral to offer a “home away from home” for families in need of overnight accommodations while receiving care at the 307-bed freestanding pediatric hospital, which is located near Coral Gables.
These 2 preferred hotels offer many types of amenities and conveniences for patient families lodging. Families may reach out directly to the hotel for more information or to make reservations with the hospitals preferred discount rate. Rates may vary by season.
Hampton Inn & Suites Blue Lagoon
This hotel is located less than 3 miles from the hospital and offers a wide range of amenities.
- Complimentary hot breakfast with a to-go option
- Complimentary Shuttle services to and back from the hospital 5am-11pm
- Laundry services
- Pool & Jacuzzi
- Outdoor games
- Business Center
- Fitness Center
Nearby Conveniences
- Nicklaus Children’s Hospital
- Miami International Airport
- Publix Grocery store
- CVS & Walgreens pharmacies
- Fast food restaurants
Hampton Inn & Suites by Hilton Website
Nuvo Suites Hotel
This hotel is located less than 8 miles from the hospital and offers a wide range of amenities.
- Business Center
- Fitness Center
- Pool
- Washer & Dryer
Nearby Conveniences
- Nicklaus Children’s Hospital
- Miami International Airport
- Malls
- Fast food restaurants
Nuvo Suites Website
Other Nearby Hotels
Additional nearby hotels may offer special rates for families with patients at Nicklaus Children's Hospital. Families should reach out directly to these hotels for more information.
Families receiving medical care at our hospital and residing outside of the tri-county area may qualify for the Lodging Program at Nicklaus Children’s Hospital. To be considered for this program, families should reach out directly to the service line coordinating their care to have a lodging referral placed on their behalf.
Hotel & Lodging Accommodations
Nicklaus Children's Hospital has partnered with Hampton Inn & Suites in Miami and Nuvo Suites in Doral to offer a “home away from home” for families in need of overnight accommodations while receiving care at the 307-bed freestanding pediatric hospital, which is located near Coral Gables.
These 2 preferred hotels offer many types of amenities and conveniences for patient families lodging. Families may reach out directly to the hotel for more information or to make reservations with the hospitals preferred discount rate. Rates may vary by season.
Hampton Inn & Suites Blue Lagoon
This hotel is located less than 3 miles from the hospital and offers a wide range of amenities.
- Complimentary hot breakfast with a to-go option
- Complimentary Shuttle services to and back from the hospital 5am-11pm
- Laundry services
- Pool & Jacuzzi
- Outdoor games
- Business Center
- Fitness Center
Nearby Conveniences
- Nicklaus Children’s Hospital
- Miami International Airport
- Publix Grocery store
- CVS & Walgreens pharmacies
- Fast food restaurants
Hampton Inn & Suites by Hilton Website
Nuvo Suites Hotel
This hotel is located less than 8 miles from the hospital and offers a wide range of amenities.
- Business Center
- Fitness Center
- Pool
- Washer & Dryer
Nearby Conveniences
- Nicklaus Children’s Hospital
- Miami International Airport
- Malls
- Fast food restaurants
Nuvo Suites Website
Other Nearby Hotels
Additional nearby hotels may offer special rates for families with patients at Nicklaus Children's Hospital. Families should reach out directly to these hotels for more information.
Families receiving medical care at our hospital and residing outside of the tri-county area may qualify for the Lodging Program at Nicklaus Children’s Hospital. To be considered for this program, families should reach out directly to the service line coordinating their care to have a lodging referral placed on their behalf.
AdolescentDocs
AllergyDocs
CardiologyDocs
CardiologySurgeryDocs
NeurosurgeryDocs
OphthamologyDocs
OralSurgeryDocs
OrthodonticDocs
OrthopedicDocs
OrthopedicHandSurgeryDocs
ENTDocs
PediatricDentists
PediatricSurgeryDocs
PeriodonticsDocs
PlasticSurgeryDocs
PodiatryDocs
PsychiatryDocs
PulmonaryMedicineDocs
RheumatologyDocs
SportsMedicineDocs
UrologyDocs
Audiology Services
Identifying hearing loss at the earliest opportunity is key to helping children achieve their full potential.
Hearing loss can affect your child’s speech and language development, school performance and social relationships.
Our Rehabilitation Services Department provides a multidisciplinary approach to intervention that will alleviate the adverse effects of hearing loss on speech and language development, academic performance, and cognitive development.
We offer the following audiology services:
Your child may need a full hearing evaluation if he or she:
- Did not pass the universal newborn hearing screening at the time of birth
- Is not reaching auditory developmental milestones
- Doesn’t respond to things said, or doesn’t seem to notice when spoken to
- Asks you to repeat things (more for older children than infants)
- Has difficulty locating the direction of a sound or voice
- Starts talking later than children the same age (based on reports by teachers, etc)
- Can’t say words and sentences the right way
- Has difficulty hearing one voice when several people are talking
- Misses quick or soft sounds
- Is performing poorly at school
- Has diseases that can cause hearing loss
- Has been diagnosed with other conditions that sometimes include hearing loss
- Has been taking medical treatments that may have hearing loss as a side effect
- Has parents or grandparents with hearing problems (hearing loss is hereditary)
Are my child’s auditory skills developing normally?
Click each box to learn about auditory developmental milestones in children.
Auditory development in newborns (Birth–3 Months)
- Startles to loud sounds
- Quiets or smiles when spoken to
- Seems to recognize your voice and quiets if crying
- Increases or decreases sucking behavior in response to sound
Auditory development in infants (4–6 Months)
- Moves eyes in direction of sounds
- Responds to changes in tone of your voice
- Notices toys that make sounds
- Pays attention to music
Auditory development in infants (7 Months–1 Year)
- Enjoys games like peek-a-boo and pat-a-cake
- Turns and looks in direction of sounds
- Listens when spoken to
- Recognizes words for common items like "cup", "shoe", "book", or "juice"
- Begins to respond to requests (e.g. "Come here" or "Want more?")
Auditory development in toddlers (1 year to 2 Years)
- Points to a few body parts when asked
- Follows simple commands and understands simple questions ("Roll the ball," "Kiss the baby," "Where's your shoe?")
- Listens to simple stories, songs, and rhymes
- Points to pictures in a book when named
Auditory development in toddlers (2 years to 3 years)
- Understands differences in meaning ("go-stop," "in-on," "big-little," "up-down")
- Follows two requests ("Get the book and put it on the table")
- Listens to and enjoys hearing stories for longer periods of time
Auditory development in children (3 years to 4 years)
- Hears you when you call from another room
- Hears television or radio at the same loudness level as other family members
- Understands words for some colors, like red, blue, and green
- Understands words for some shapes, like circle and square
- Understands words for family, like brother, grandmother, and aunt
Auditory development in children (4 years to 5 years)
- Understands words for order, like first, next, and last
- Understands words for time, like yesterday, today, and tomorrow
- Follows longer directions, like "Put your pajamas on, brush your teeth, and then pick out a book"
- Follows classroom directions, like "Draw a circle on your paper around something you eat"
- Hears and understands most of what is said at home and in school
Auditory Processing Disorder Evaluations
Does my child have an auditory processing disorder?
Signs and symptoms of an Auditory Processing Disorder:
- Difficulty understanding speech in the presence of competing background noise
- Problems with the ability to localize the source of a signal
- Inconsistent or inappropriate responses to requests for information
- Difficulty following rapid speech
- Frequent requests for repetition and/or rephrasing of information
- Difficulty following directions
- Difficulty or inability to detect the changes in rhythm, stress, and intonation in speech
- Difficulty learning a foreign language or novel speech materials, especially technical language
- Difficulty maintaining attention
- A tendency to be easily distracted
- Poor singing, musical ability, and/or appreciation of music
- Academic difficulties, including reading, spelling and/or learning problems
Auditory Processing Evaluation Referral Criteria
- 7 years of age
- English is the main language spoken in the home
- Within normal limits speech and language skills
- Within Normal limits IQ – 90 or above
- Within Normal limits hearing
Audiology Services
Identifying hearing loss at the earliest opportunity is key to helping children achieve their full potential.
Hearing loss can affect your child’s speech and language development, school performance and social relationships.
Our Rehabilitation Services Department provides a multidisciplinary approach to intervention that will alleviate the adverse effects of hearing loss on speech and language development, academic performance, and cognitive development.
We offer the following audiology services:
Your child may need a full hearing evaluation if he or she:
- Did not pass the universal newborn hearing screening at the time of birth
- Is not reaching auditory developmental milestones
- Doesn’t respond to things said, or doesn’t seem to notice when spoken to
- Asks you to repeat things (more for older children than infants)
- Has difficulty locating the direction of a sound or voice
- Starts talking later than children the same age (based on reports by teachers, etc)
- Can’t say words and sentences the right way
- Has difficulty hearing one voice when several people are talking
- Misses quick or soft sounds
- Is performing poorly at school
- Has diseases that can cause hearing loss
- Has been diagnosed with other conditions that sometimes include hearing loss
- Has been taking medical treatments that may have hearing loss as a side effect
- Has parents or grandparents with hearing problems (hearing loss is hereditary)
Are my child’s auditory skills developing normally?
Click each box to learn about auditory developmental milestones in children.
Auditory development in newborns (Birth–3 Months)
- Startles to loud sounds
- Quiets or smiles when spoken to
- Seems to recognize your voice and quiets if crying
- Increases or decreases sucking behavior in response to sound
Auditory development in infants (4–6 Months)
- Moves eyes in direction of sounds
- Responds to changes in tone of your voice
- Notices toys that make sounds
- Pays attention to music
Auditory development in infants (7 Months–1 Year)
- Enjoys games like peek-a-boo and pat-a-cake
- Turns and looks in direction of sounds
- Listens when spoken to
- Recognizes words for common items like "cup", "shoe", "book", or "juice"
- Begins to respond to requests (e.g. "Come here" or "Want more?")
Auditory development in toddlers (1 year to 2 Years)
- Points to a few body parts when asked
- Follows simple commands and understands simple questions ("Roll the ball," "Kiss the baby," "Where's your shoe?")
- Listens to simple stories, songs, and rhymes
- Points to pictures in a book when named
Auditory development in toddlers (2 years to 3 years)
- Understands differences in meaning ("go-stop," "in-on," "big-little," "up-down")
- Follows two requests ("Get the book and put it on the table")
- Listens to and enjoys hearing stories for longer periods of time
Auditory development in children (3 years to 4 years)
- Hears you when you call from another room
- Hears television or radio at the same loudness level as other family members
- Understands words for some colors, like red, blue, and green
- Understands words for some shapes, like circle and square
- Understands words for family, like brother, grandmother, and aunt
Auditory development in children (4 years to 5 years)
- Understands words for order, like first, next, and last
- Understands words for time, like yesterday, today, and tomorrow
- Follows longer directions, like "Put your pajamas on, brush your teeth, and then pick out a book"
- Follows classroom directions, like "Draw a circle on your paper around something you eat"
- Hears and understands most of what is said at home and in school
Auditory Processing Disorder Evaluations
Does my child have an auditory processing disorder?
Signs and symptoms of an Auditory Processing Disorder:
- Difficulty understanding speech in the presence of competing background noise
- Problems with the ability to localize the source of a signal
- Inconsistent or inappropriate responses to requests for information
- Difficulty following rapid speech
- Frequent requests for repetition and/or rephrasing of information
- Difficulty following directions
- Difficulty or inability to detect the changes in rhythm, stress, and intonation in speech
- Difficulty learning a foreign language or novel speech materials, especially technical language
- Difficulty maintaining attention
- A tendency to be easily distracted
- Poor singing, musical ability, and/or appreciation of music
- Academic difficulties, including reading, spelling and/or learning problems
Auditory Processing Evaluation Referral Criteria
- 7 years of age
- English is the main language spoken in the home
- Within normal limits speech and language skills
- Within Normal limits IQ – 90 or above
- Within Normal limits hearing
Patient Stories
Patient Stories
Common Sports Injuries
Conditions we Treat
Programs and Services
News
Conditions We Treat
Conditions We Treat
Patient Stories
Patient Stories
Conditions we Treat
Conditions We Treat
Patient Stories
Prenatal Diagnostic Tests
Specialist Programs and Services
Craniofacial Center Home
Orthopedics Home
Orthopedics Home
Orthopedics Home
Orthopedics Home
Orthopedics Home
Heart Institute Home
Plastic Surgery Home
Sports Health Home
Volunteer Resources Home
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur magni dolores eos qui ratione voluptatem sequi nesciunt. Neque porro quisquam est, qui dolorem ipsum quia dolor sit amet, consectetur, adipisci velit, sed quia non numquam eius modi tempora incidunt ut labore et dolore magnam aliquam quaerat voluptatem. Ut enim ad minima veniam, quis nostrum exercitationem ullam corporis suscipit laboriosam, nisi ut aliquid ex ea commodi consequatur? Quis autem vel eum iure reprehenderit qui in ea voluptate velit esse quam nihil molestiae consequatur, vel illum qui dolorem eum fugiat quo voluptas nulla pariatur?
Fetal Care Home
Music Therapy Home
Music Therapy Students
Music Therapy Student Programs
Practicum
Music therapy practicum opportunities are available at Nicklaus Children’s Hospital for University of Miami students pursuing a bachelor’s or equivalency degree in Music Therapy each Fall & Spring.
To become eligible for our practicum, you must be a music therapy student at the University of Miami-Frost School of Music. Medical Education for clinical students. Students must be in the process of pursuing a bachelor’s degree and have senior level status or are graduate equivalency students earning a degree in a music therapy major. The practicum lasts a minimum of 14 weeks, 2 hours per week, for a total of 28 hours.
Internship
Music therapy internship opportunities will be available at Nicklaus Children’s Hospital for University of Miami students pursuing a Music Therapy degree, beginning in Summer.
Music therapy internships at Nicklaus Children's Hospital are structured to provide students a variety of opportunities for experience and practice in assessment, treatment, and discharge processes. While completing music therapy student clinical hours, interns will be mentored in: providing procedural support, assisting with pain management, supporting both new diagnoses and bereavement situations, facilitating motor, speech/communication and other developmental goals, and increasing a patient’s compliance with medical care. The internship lasts a minimum of 26 weeks, 40 hours per week, for a total of 1,040 hours.
Music Therapy Internship Requirements
To become eligible for our internship, you must be a music therapy student at the University of Miami-Frost School of Music. Medical Education for clinical students. Students must be in the process of pursuing a bachelor’s degree and have senior level status or are graduate equivalency students earning a degree in a music therapy major.
Selection of Music Therapy interns is determined based on a variety of criteria that include: academics, previous experience working with children in or outside of hospital setting, references, and an interview. Please note that due to the number of applicants and limited space, we are unable to grant every applicant an interview.
For those that are interested in learning more about the Music Therapy profession, please follow the links below.
Patient Stories
kristine-j-gulesarian
darline-santana-acosta
madalsa-dipak-patel
reshma-babra-naidoo
tacy-elizabeth-downing
jose-g-calderon
scott-jacob-schoenleber
beatriz-franyie-ladd
claudette-e-gonzalez
lesbia-drukteinis
maria-valcourt-rodriguez
rosemary-prince
suheily-aponte-rodriguez
vanessa-freitas
asit-vora
kyle-luis-solari
joshua-william-tarkoff
shifra-avigail-koyfman
Nursing Conference Registration
Please register below to reserve your seat at "Raising the Bar: Pediatric Nursing Conference Above Par", the 3rd Annual Nicklaus Children's Hospital Pediatric Nursing Conference.
Nutrition Symposium Registration
Event Date: Saturday, September 14st, 2024
Your registration will not be completed until payment is received.
Payments by Credit Card
Please complete your registration and proceed to the Payments page.
Registration Fees*
- Regular registration - $100
- Nicklaus Children's Hospital Employees & SFAND members - $70
- Groups of 5 or more - $85
- Students - $55
*Breakfast and lunch included.Nutrition Symposium Payment
Success! We have received your information.
Thank you for registering for the 6th South Florida Pediatric Nutrition Symposium. Please note that registration will not be completed until payment is received.
Payment by Credit Card
You will be re-directed to Authorize.net to complete the credit card payment.
Regular registration - $100
NCHS Employee or SFAND Member - $70
Groups of 5 or more - $85
Payments by Check
Please make all checks payable to: Miami Children's Health System
Send payment to:
Miami Children's Health System
Attn: Erin Corrigan
Clinical Nutrition Manager
3100 SW 62 Avenue
Miami, FL 33155
diego-jaramillo-radiology
fuad-alkhoury-pediatric-surgery
gloria-diaz-medina-neurology
john peters-gastroenterology
mercedes-bello-neurology
suzanne-hagler-neurology
hugh-ladd-critical-care-medicine
ivana-vukovic-general-pediatrics
leonardo-torres-otolaryngology
michelle-fernandez-clinical-psychology
Saranga-Agarwal-Hospitalist-Services
travis-tierney-neurosurgery
alireza-alam-urology
ana-hernandez-puga-general-pediatrics
brianna-ruiz-varas-general-pediatrics
carmen-molina-general-pediatrics
catricia-tilford-general-pediatrics
christie-de-la-vega-general-pediatrics
Doris-Aguilar-Hospitalist-Services
george-ibrahim-neurosurgery
harvey-chim-plastic-surgery
Jose-Ramon-Azaret-General-Pediatrics
mariselis-rosa-sanchez-nephrology
naiomi-cohen-general-pediatrics
natanya-mishal-neurology
Sherrie-Joy-Baysa-Cardiology
Obioma-Nwobi-Nephrology
nirmal-nathan-plastic-surgery
ana-ojeda-clinical-psychology
annette-parlade-general-pediatrics
asif-suchedina-emergency-medicine
catalina-granada-solis-gynecology
Craig-McKeown-Ophthalmology
joerdan-ricketts-general-pediatrics
luis-blanco-general-pediatrics
mariana-velazquez-oral-surgery
Rosario-Gely-General-Pediatrics
Carol-DaCosta-General-Pediatrics
Maureen-Mendoza-General-Pediatrics
Octavio-Vasconcello-Cohen-General-Pediatrics
sussi-vivar-general-pediatrics
Vijaykumar-Zaveri-Otolaryngolog
m-bianco-batlles-neonatology
michael-finer-general-pediatrics
katherine-lens-general-pediatrics
dominick-figueroa-general-pediatrics
Sports Health Videos
News: Research & Innovation
ismael-morera-general-pediatrics
Gladys-Vazquez
lynn-model
manuel-castellanos
sharon-ramos
Yanetsi-Flores-Landa
Bismark-Gonzalez
Pedro-Sequeira
sherry-levine
beatriz-nazario-lugo
Andrew-Rivera
belkys-bravo
Elliot-Pearson
james-huhta
juan-del-sol
Matthew-Ramirez
padma-gupta
rosario-pinero-correa
ryan-durfee
dana-mcmakin
ashraf-beharrie
liat-corcia
lori-fein
martha-lopez
mohammed-ezuddin
Scott-Raskin
vanessa-celleri-gomezcoello
cynthia-christoph
eugenio-vazquez
Contact Us
Please select the topic that best describes your situation:
En Español
ann-mary-fernandez-general-pediatrics
Avanee-Lobo
jessica-tufino-general-pediatrics
juan-quintero-orthodontics
roberto-uriel-general-pediatrics
roxanna-santana-general-pediatrics
Steven-Siegel-General-Pediatrics
ann-christina-brady-pediatric-surgery
barry-resnik-dermatology
joseph-luka
rene-landa-pediatric-dentistry
tin-mai-radiology-house-officer
hilma-rodriguez-pediatric-dentistry
leonard-feld-nephrology
niyasdeen-dieguez-santiesteban
linda-martinez-general-pediatrics
ramon-oyarzun-general-pediatrics
jessica-cardona-general-pediatrics
ravi-pujara-general-pediatrics
rosemary-ojo-otolaryngology
Giovanna-Ciocca-Dermatology
Krysten-Chin-General-Pediatrics
Maria-Granados-Fornez
Norman-Pevsner-Radiology
airama-padron-general-pediatrics
abigail-pudpud-general-pediatrics
James-Banks-Radiology-House-Officer
dorsey-goosby-general-pediatrics
robert-starke-neurosurgery
Maps and Floorplans of the Hospital Campus
Find printable PDF maps of the hospital building, parking garages, surrounding streets and detailed directions on how to navigate to different departments located on each floor.

Click to download PDF
Are you looking for...?
- ATM - ATM machines are located near the Ambulatory Care Building entrance and near the hospital's cafeteria.
- Cafeteria and Cafés - The Nicklaus Children's Hospital Cafeteria, the Golden Cub Café, is located on the first floor of the Variety wing, we also have several food service facilities on the ground floor offering a variety of meal and snack choices.
- Mail Drop Box - A mailbox is located near the entrance to the cafeteria.
- Nursing/Breastfeeding Room - Facilities available on 2NE, the Neonatal Intensive Care Unit (NICU) and Michael Fux Family Center.
- Pharmacy - The Publix Pharmacy at Nicklaus Children's is conveniently located on the first floor of the central wing, and is easily accessible via the Devonshire lobby entrance.
- Vending Machines - A variety of vending options are available on the ground floor near the cafeteria, in the Advanced Pediatric Care Pavilion lobby as well as near the entrance to the 2North Unit.
- Valet Services - As a convenience to patient families and visitors, Nicklaus Children's Hospital offers complimentary 24/7 valet parking in front of the Central Building, near the Devonshire Boulevard entrance to the campus. Additionally, complimentary valet services are offered in the blue and yellow garages during select hours. For more information visit our hospital parking page.
Medical Departments Floor Plans
Level 1 (Ground Floor) Floor Plan
LabCoats
Blog Posts
About the Bloggers
Subscribe
Blog
Motion Analysis
Our state of the art motion capture technology allows us to analyze sport specific skills to reveal suboptimal biomechanical movement strategies that increase the risk of injury.
Motion Capture technology provides a detailed assessment of joint angles and movement patterns that are used to develop individualized training programs to decrease the risk of injury and improve sport performance.
Motion Analysis Programs:
Hurricane Updates
This page was last updated on: {% DocumentContext.CurrentDocument.DocumentLastPublished |(user)MCH-rherrera1|(hash)0aec6678707b7dce039185d888d8d3ea32b6ef370585b492f52f807d628796b1%}
ENGLISH
Hurricane Milton | Update #4
Because of storm’s impact, we have adjusted our operations as follows:
Thursday, October 10, 2024
- All Miami-Dade locations are open with regular hours of operations.
- All Broward locations including urgent care centers and NCPS offices will open at 1 p.m.
- All Palm Beach locations including urgent care centers and NCPS offices remain closed for the day.
- Palm City location remains closed for the day.
ESPAÑOL
Huracán Milton | Actualización n.° 4
Debido al impacto de la tormenta, hemos ajustado nuestros centros de la siguiente manera:
Jueves 10 de octubre de 2024
- Todas las ubicaciones de Miami-Dade están abiertas en el horario habitual de atención.
- Todas las ubicaciones de Broward, incluidos los centros de cuidados urgentes y los consultorios de NCPS, abrirán a la 1:00 p. m.
- Todas las ubicaciones de Palm Beach, incluidos los centros de cuidados urgentes y los consultorios de NCPS, permanecerán cerrados durante el día.
- La ubicación de Palm City permanecerá cerrada durante el día.
e-PPGC
Videos
nicole-christin-nephrology
monica-dussan-endocrinology
amy-feldman-allergy-immunology
brian-ho-otolaryngology
james-enos-cardiology
patrick-lolo-pediatric-dentistry
kelly-seiler-endocrinology
michael-lopez-cardiology
pedro-pagan-banchs-endocrinology
saoussen-salhi-plastic-surgery
yonit-sterba-rakovchik-rheumatology
Conditions We Treat
Conditions We Treat
Comprehensive Programs and Services
Ion-Channel Epilepsy Program
Part of the nationally recognized
Nicklaus Children's Brain Institute, the Ion-Channel Epilepsy (Dravet syndrome) Program provides comprehensive care for children with genetically based epilepsy referred from all over the country. The multidisciplinary team includes neurologists and genetics specialists and offers diagnostic screening and the latest medical management, including participation in emerging
clinical trials.
Ion-Channel Epilepsy Program
Part of the nationally recognized
Nicklaus Children's Brain Institute, the Ion-Channel Epilepsy (Dravet syndrome) Program provides comprehensive care for children with genetically based epilepsy referred from all over the country. The multidisciplinary team includes neurologists and genetics specialists and offers diagnostic screening and the latest medical management, including participation in emerging
clinical trials.
Rare Chromosomal Disorders Program
Part of the nationally recognized
Nicklaus Children's Brain Institute, the Rare Chromosomal Disorders Program offers a multidisciplinary team of geneticists, neurologists, and other specialists to address the complex needs of children with rare chromosomal disorders that often have multisystem involvement.
Rare Chromosomal Disorders Program
Part of the nationally recognized
Nicklaus Children's Brain Institute, the Rare Chromosomal Disorders Program offers a multidisciplinary team of geneticists, neurologists, and other specialists to address the complex needs of children with rare chromosomal disorders that often have multisystem involvement.
Tuberous Sclerosis Program
Part of the nationally recognized Nicklaus Children's Brain Institute, the Tuberous Sclerosis Program is one of the first comprehensive programs for children in the United States, and offers expertise in multisystem management of uncontrolled epilepsy and cardiac involvement.
Offerings include some of the safest, and least invasive strategies, including laser ablation to cure intractable seizures, management of infantile spasms, as well as use of the ketogenic diet.
Tuberous Sclerosis Program
Part of the nationally recognized Nicklaus Children's Brain Institute, the Tuberous Sclerosis Program is one of the first comprehensive programs for children in the United States, and offers expertise in multisystem management of uncontrolled epilepsy and cardiac involvement.
Offerings include some of the safest, and least invasive strategies, including laser ablation to cure intractable seizures, management of infantile spasms, as well as use of the ketogenic diet.
Tuberous Sclerosis Program
Part of the nationally recognized Nicklaus Children's Brain Institute, the Tuberous Sclerosis Program is one of the first comprehensive programs for children in the United States, and offers expertise in multisystem management of uncontrolled epilepsy and cardiac involvement.
Offerings include some of the safest, and least invasive strategies, including laser ablation to cure intractable seizures, management of infantile spasms, as well as use of the ketogenic diet.
Conditions we Diagnose
Meet the Sports Health Team
When sports and fitness get a little too intense for kids and teens, Nicklaus Children's Hospital, is there to help. We’re proud to be a leader in orthopedic services, specializing in youth sports injuries and general pediatric orthopedics and surgery.
Our doctors, nurses and trainers have diversified backgrounds and unique approaches with an unparalleled understanding of what is required to help their patients return to their optimal level of health and athletic performance. When your child or teen gets hurt, let us help with their care and rehabilitation.
Sports Health Appointment Request
Thank You
Success! This is a confirmation that your submission has been added to our database.
The Nicklaus Children's Coordinator will schedule your appointment within 24-48 business hours.
For more information, you may also call 305-418-SPRT (or 305-418-7778) or toll free at 1-855-624-SPRT(1-855-624-7778)
Conditions We Treat
Nutrition Counseling
Performance Programs and Services
Whether your child is competing as an elite athlete at a national level or just loves to run in the park, our holistic, specialized programs will help them achieve their personal health and fitness goals.
Specialist Programs and Services
Comprehensive Programs
The first step in treating patients with craniofacial differences is to conduct a complete evaluation and make a diagnosis. Since each facial difference is unique, the expertise of a multidisciplinary team of various medical, surgical and rehabilitation specialists is required to develop a systematic, comprehensive treatment plan for each child.
The initial evaluation is conducted during a single appointment attended by a variety of team specialists. Following the assessment, the team members deliver a diagnosis and make recommendations regarding treatment and comprehensive/continuous care.
Conditions We Treat
Leadership Kickoff RSVP
This is an in-person event where all COVID-19 safety protocols will be strictly followed. Please fill in your name and email address to RSVP with all of the details for this event. Once you submit this form you will receive an email confirmation of being added to the guest list.
Thursday, March 10, 2022
Time: 8:30 am to 4:30 pm
Location: Jungle Island, 1111 Parrot Jungle Trail, Miami, FL 33132
Please RSVP by Friday, February 18, 2022.
anamaria-pulido-hospitalist-services
Specialist Programs and Services
Nicklaus Children's Hospital Department of Neurosurgery offers a variety of programs tailored to children, including:
- Bone Dysplasia/Achondroplasia
- Neurofibromatosis Program
- Neural Tube/Spina Bifida
adriana-amelinckx-lacruz-general-pediatrics
mayra-dominguez-burns-general-pediatrics
yurelis-garcia-miras-general-pediatrics
ellie-rakovchik-emergency-medicine
kamilah-ziodeen-general-pediatrics
bhavi-patel-cardiac-critical-care
Support Groups, Therapy Programs and Workshops
To register or for more information regarding support groups, please contact Maday Bonet via e-mail at Maday.Bonet@Nicklaushealth.org or call (786) 624-3566.
Diagnostic Services and Tests
- 3T Tesla MRI
- Bone Densitometry
- Digital Radiography
spreadjoy
Nico's Promise
In Memory of George Lesmes, PhD Fund
Accessibility and Usability
At Nicklaus Children’s Hospital, we are committed to ensuring that individuals with disabilities enjoy full access to our services, whether in-person at our main campus hospital and at our outpatient/urgent care centers, or on-line through our websites.
In recognition of this commitment, Nicklaus Children’s Hospital is in the process of modifying its website, www.nicklauschildrens.org, to increase the accessibility and usability of this website. In making these modifications, we will use the relevant portions of the Web Context Accessibility Guidelines 2.0 (WCAG 2.0) as our standard. Please be aware that our efforts are ongoing.
If, at any time, you have difficulty using www.nicklauschildrens.org, or a particular web page or function on this site, please contact us by phone (305-666-6511) or email (info@nicklaushealth.org) and we will make all reasonable efforts to assist you.
NCYA
ncyaevents
Leadership Kickoff Survey
Procedures and Treatments
The Division of Neurosurgery offers state of the art surgical management of disorders of the nervous system including:
- Minimally invasive removal of brain tumors
- MRI guided laser ablation surgery (Visualase)
- Surgical treatment of Epilepsy
- Inflammatory/Infectious processes of the brain and spine (e.g. brain abscess)
- Peripheral nerve surgery (e.g. Brachial Plexus and Peripheral Nerve Programbrachial plexus repair)
- Surgical treatment of Spasticity (selective dorsal rhizotomy/baclofen pumps)
- Surgical treatment of vascular malformations of the brain and spinal cord
Surgical Excellence
The surgical team is pushing forward the frontiers of pediatric neurosurgery through its active clinical and translational research programs to develop novel treatment approaches for pediatric brain tumors and head trauma and new non-invasive surgical approaches for the treatment of epilepsy.
In addition, the team has clinical expertise using:
- Minimally invasive endoscopic techniques
- Frameless stereotactic guidance
- Intraoperative mapping to preserve normal brain function
Read below for more details about the different surgical procedures offered:
doctorsday
thankyoudoctor
coloringbooks
Renaissance
Camp Superstar
Extra Mile
keytothecloset
lourdes-prieto-cardiology
paul-cardenas-clinical-genetics-metabolism
Citrix
Adolescent Medicine Fellowship
Music Therapy
Bear Hugs
Improv
Vacc Camp
peter-volsky-otolaryngology
ana-victoria-ophthalmology
carmen-alfonzo-general-pediatrics
fernando-diez-general-pediatrics
jason-mishal-anesthesiology
marina-bishai-hospitalist-services
martin-andreansky-hematology-oncology
taj-madiwale-emergency-medicine
thomas-chu-radiology-house-officer
Carlin Prom
carrie-firestone-baum-gastroenterology
arthur-desrosiers-plastic-surgery
hilda-brito-general-pediatrics
lissette-perez-lima-clinical-psychology
Miracle Jeans Day
Bake a Difference
Diamond Ball
Fashion Gives Back
Victor Center Support
Lemonade Stand
Conditions we Treat
Conditions We Treat
Tribute Bricks
Partnerships
Organization Partnerships
- Alper JCC Miami
- Hudson & Hundreds Foundation
- Junior Orange Bowl
- JCC Maccabi Games
- Stephen Tulloch Foundation
School Partnerships
Sports Programs
Planned Giving
NCHS Portal
Conditions We Treat
Ear, nose, throat, head and neck problems are a common occurrence in children of all ages. Our highly-skilled and experienced surgeons not only treat the typical or recurring pediatric otolaryngology problems, they also evaluate and treat facial trauma, provide assistance in overcoming the numerous otolaryngologic manifestations of cystic fibrosis, evaluate and treat head and neck tumors and evaluate and treat complex airway problems.
Audiology
The Craniofacial Center audiologists perform hearing evaluations and monitor any hearing problems during the craniofacial team visits or on a more frequent basis if needed. Newborn infants should have hearing evaluations soon after birth.
Why is an audiology evaluation important?
Studies confirm that between 95.5 and 100 percent of infants born with cleft palate have fluid present in the middle ear space at birth. This condition, known as middle ear effusion, can exist for several years if left untreated.
Normally, the middle ear space, if free of fluid, is filled with air through which sound passes from the vibrating eardrum to the tiny bones in the middle ear. The sounds are then programmed as meaningful sounds through the nervous system to the brain.
When the middle ear does not drain fluid sufficiently, this interferes with the "conduction of the sound" in the middle ear space, and can prevent normal hearing development.

Probably, the most significant impact caused by the inability to hear normally is an adverse impact on development of speech and language. Good hearing is essential to speech and language, and the social and intellectual development of infants and young children.
Adults use their hearing to communicate with other people. Very young children, meanwhile, use their hearing to develop speech and language skills in order to communicate. Any amount of hearing loss in a child can make the learning of speech and language difficult.
Craniofacial Center Pediatric Audiologists
The audiologist is an important member of the craniofacial team. They will be able to test your child's hearing and identify if your child has any hearing loss, regardless of the child's age.
Conditions we Treat
Conditions we Treat
Dental Services
 Cleft lip/palate and other craniofacial anomalies usually affect a child’s dental development. Teeth in the area of the cleft may be missing or improperly positioned. There may also be extra teeth or malformed teeth. In addition, affected teeth may be more susceptible to tooth decay. For these reasons, care of the teeth should begin as soon as the teeth emerge. Preventive practices with regular visits to the pediatric dentist will help to ensure the best dental outlook for your child.
Cleft lip/palate and other craniofacial anomalies usually affect a child’s dental development. Teeth in the area of the cleft may be missing or improperly positioned. There may also be extra teeth or malformed teeth. In addition, affected teeth may be more susceptible to tooth decay. For these reasons, care of the teeth should begin as soon as the teeth emerge. Preventive practices with regular visits to the pediatric dentist will help to ensure the best dental outlook for your child.
Monthly Giving
Speech and Language Pathology
 The speech and language pathologist with feeding experience will assist you with learning how to feed your infant with craniofacial differences. In subsequent visits to the team, the speech pathologist will evaluate speech and language and will make necessary recommendations to ensure that your child’s speech develops correctly.
The speech and language pathologist with feeding experience will assist you with learning how to feed your infant with craniofacial differences. In subsequent visits to the team, the speech pathologist will evaluate speech and language and will make necessary recommendations to ensure that your child’s speech develops correctly.
The first evaluation of your child will probably occur sometime in the first year. As your child grows and develops, the speech pathologist will evaluate the following:
- How well your child understands language and puts ideas into words
- How well your child can make various sounds
- The tone quality of your child’s voice
Speech pathologists are trained to prevent as well as correct speech problems, They can teach children with a cleft palate to develop clear speech and show parents how to perform speech therapy with the child at home. Some children need little to no therapy, while others may need therapy support for several years.
With adequate help, practically all children with cleft lip/palate develop easily understood speech. They may speak as well as their classmates by the time schooling begins.
Pediatric Speech Language Pathologists
Genetics
 The geneticist at the Craniofacial Center specialized in determining the possible reasons why your child was born with a craniofacial difference. The genetics team works with children who have congenital anomalies and/or inherited conditions. They can answer questions such as why cleft lip/palate occurs, the chances of it occurring in subsequent children, and what to expect in the future.
The geneticist at the Craniofacial Center specialized in determining the possible reasons why your child was born with a craniofacial difference. The genetics team works with children who have congenital anomalies and/or inherited conditions. They can answer questions such as why cleft lip/palate occurs, the chances of it occurring in subsequent children, and what to expect in the future.
To help find out what might have caused your child’s craniofacial anomaly, the genetics professional will ask questions about your child’s medical and developmental history as well as at least three generations of your family history.
The geneticist and genetic counselor will also review any medical or genetic testing that your child has had previously. After reviewing all available information and performing a detailed physical examination, the genetics professional will determine if further genetic testing and/or evaluation is necessary. If a confirmed diagnosis is determined, the genetic professional will discuss what this means to your child and family’s future.
Parent and Patient Advocates
Parent advocate are parents who, like you, have a child with a craniofacial difference. They will share with you their experiences and offer valuable advice. They are available for emotional support as well as information regarding insurance coverage, state laws that protect children with craniofacial conditions, parent support group meetings, craniofacial summer camp, and other needs you may have.
Patient advocates are past patients of the Craniofacial Center who can offer support and guidance to parents and patients. Their experiences as patients provide a valuable perspective to families learning to navigate the aspects of craniofacial differences.
Conditions we Treat
Conditions We Treat
Conditions We Treat
Conditions We Treat
Conditions We Treat
Conditions we Treat
Conditions We Treat
RSVP - General Staff Meeting
Please fill out the form to RSVP for the General Staff Meeting.
Tuesday, December 3, 2024 at 6:00 p.m.
See the event invitation.
Thank You
Success! your RSVP has been submitted. Thank you.
GIVE
Prenatal Orthopedic Consults
Prenatal Orthopedic Consults
Wheelchair/Seating and Mobility Clinic
Pediatric Nursing Certification
Please register below to reserve your seat at Pediatric Nursing Certification Review Course.
Classes and Workshops
Nicklaus Children's Hospital extends its expertise through its educational offerings to the community providing classes and courses, in addition to family-centered services to parents, families and professionals. Browse the full listing of events in our
community calendar to discover which upcoming events you would like to attend.
Comprehensive Programs and Services
sanjiv-bhatia-neurosurgery
Conditions we Treat
Conditions we Treat
UVIP Home
UVIP Home
Urodynamic Testing
Urodynamic Testing
CME Relicensure Courses
Earn CME credit that counts towards your license renewal from the comfort of your own home or office!
Nicklaus Children’s Hospital is proud to offer Florida required courses on its on-demand CME platform, iLearnPeds.com. Upon registration and completion of any of the courses shown below, you will receive a CME certificate with the amount of AMA PRA Category 1 CreditsTM shown below.
These courses are offered for a flat fee, rated per CME Credit hour. Discounted rates are available for credentialed staff. A 100% off discount is offered for existing NCHS employees and Geographic Medical Staff. Discounts are also offered to medical students.
Click the links below to be redirected to each online course page.
- Domestic Violence
Issued on: December 8, 2017
Expires on: December 7, 2020
2 AMA PRA Category 1 Credits™
- HIV/AIDS Update
Issued on: January 19, 2018
Expires on: January 18, 2020
1 AMA PRA Category 1 Credits™
- NEW! Prescribing Controlled Substances
(Provided by Baptist Health South Florida)
Issued on: February 1, 2020
Expires on: January 31, 2021
2 AMA PRA Category 1 Credits™

Click the banner above to be view the schedule & pre-register
Accreditation Statement
Nicklaus Children’s Hospital is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Disclosure and Conflict of Interest Resolution
All conflicts of interest of any individual(s) in a position to control the content of a CME activity will be identified and resolved prior to the educational activity being provided. Disclosure about provider and faculty relationships, or the lack thereof, will be provided to learners.
Links and Resources
CME Requirements for Relicensure (FMA)
Florida Special Needs Occupant Protection Program
A project of the Florida Department of Health, Bureau of Emergency Medical Services.
Funded by:
A grant from the Florida Department of Transportation.
In Cooperation with:
Our Mission
To promote injury prevention and advocate for the safety and protection of all children with special needs and their families while riding in motor vehicles.
Dade County Special Needs Technicians:
Physician Details
Our Program
How to Apply
Scholarly Activity
Our City
Our City
Our City
Where We Work
Pediatric Residency Program
Wellbeing
Radiology Home
For Patients and Families
Why personalized medicine? At Nicklaus Children’s, researchers and clinicians are working together to improve the way healthcare is delivered to each child.
What does this mean for me or my child?
We know you may have questions or want to learn more about genetics, genomics and what it means for health and wellness. The Nicklaus PMI provides summary documents, links to other resources, and answers to frequent questions about genetics, genomics and genetic testing.
Frequently Asked Questions about PMI
Q: What is the difference between genetics and genomics?
A: Genetics is the study of inheritance, or the way traits are passed down from each generation. Genes carry instructions that influence traits, for example hair color or height. Genomics is a term used to describe the study of all genes in a person, as well as interactions of genes with an individual’s environment.
Q: I am pregnant or am planning to become pregnant and have questions about prenatal genetic screening. Where can I go for information or services?
A: The
Victor Center at Nicklaus Children’s provides comprehensive services including education, counseling services, and affordable preconception genetic screening.
The American College of Obstetricians and Gynecologists (ACOG) also has helpful online resources.
Q: What should I know about family health history?
A: Your family health history may indicate if you or your child are at genetic risk for certain conditions. It may help your doctor make a diagnosis if your child shows symptoms of a disease or customize health services.
The
Centers for Disease Control (CDC) and
Genetic Alliance have resources that can help you start a conversation about family health history with your health care provider.
Patient Advocacy and Resources
- Genetic and Rare Diseases Information Center (GARD)- GARD provides the public with access to current, reliable, and easy-to-understand information about rare or genetic diseases in English and Spanish.
- Genetic Alliance- Genetic Alliance engages individuals, families, and communities to advocate for access to quality genetic services.
Research Projects Open for Enrollment
For Clinicians
Our mission is to advance knowledge in personalized medicine by translating the newest discoveries into bedside care. As the only freestanding children’s hospital in Southern Florida, Nicklaus Children’s strives to be cutting-edge.
Nicklaus Children’s is one of seven children’s hospitals in the Sanford Children’s Genomic Medicine Consortium, an innovative collaboration of hospitals across the nation inspired by philanthropist Denny Sanford. This partnership allows us to bring the most innovate advancements in personalized care to the families we serve.
Clinician Resources
There is a need for primary care physicians and specialists to incorporate personalized medicine and genomics into their practice. For the primary care physician, taking a detailed family history may offer insight into health conditions for which your patient is at higher risk. For a cardiothoracic surgeon, 3D tissue printing can create a surgical model that allows for smaller surgical incision. Learn more about areas of personalized medicine through our resources.
About Sanford Children’s Genomic Consortium
Nicklaus Children’s Hospital is a member of the Sanford Children’s Genomic Medicine Consortium. This is an innovative collaboration of seven children’s hospitals that are advancing personalized medicine into pediatric healthcare. Members of the consortium include Nicklaus Children’s Hospital, Sanford Children’s, Children’s Hospital Los Angeles, Rady Children’s Hospital- San Diego, Children’s Hospital Colorado, Children’s Hospital and Clinics of Minnesota, and Banner Children’s Tucson.
The consortium utilizes joint research programs across sites to develop new and innovative standards of practice for children in personalized medicine. The participation of sites across the country ensures that these innovations in care are developed with racially and ethnically diverse populations in mind.
CPM Programs
The Center of Precision Medicine is not a separate service of the health system, but is woven into all hospital service lines and outpatient centers to optimize and personalize care.
Salaries & Benefits
Learn More about Genomic Medicine
CPM Home
patcharapong-suntharos-cardiology
CustomerService
Sanjiv Bhatia Endowed Chair
PhysicianReferral
JuanMartinez
nicole-cabbad-plastic-surgery
Gastroenterology Home
JuanMillon
SamSkaff
sajel-kana-geneticist
gregory-hornig-neurosurgery
Neurosurgery (Home)
Conditions we Treat
Conditions we Treat
Colorectal Center Home
Colorectal Center Home
Psychology Videos
Pediatric Orthopedic Spine Fellowship
Neurology (Home)
janeris-loredo-psychiatry
Pain Management
September is Pain Awareness Month. This month-long recognition was created to increase education and awareness within our community about the effects of pain, the available treatments to alleviate pain and the importance of communication with healthcare providers regarding pain-related concerns so that pain can be better understood and treated.
How can you support pain awareness?
- Show your support during September's Pain Awareness Month by wearing PURPLE shirts/jackets/sweaters on Pain Awareness Spirit Days (Monday Sept. 1st & Sunday Sept. 18th).
- Wear PURPLE accessories with your professional attire/uniform during the entire month of September to further demonstrate your Pain Awareness support. Examples of PURPLE accessories include: hair color, make-up, face-painting, ribbons, glasses, jewelry, ties, hair caps, belts, jackets, sweaters, scarves, tutus, masks, socks, and shoes.
How we work together to manage children's pain
Nicklaus Children's partners with parents to assess pain at regular intervals and take measure to reduce discomfort. When appropriate, medications are used to reduce pain, along with the following:

Swaddling and Positioning

Warm blankets

Distraction techniques
(toys, bubbles, games)

Playing favorite music
Learn more

Breathing exercises / Relaxation /Guided Imagery

Favorite comfort items

Bedside volunteers to read and play games

Movement and Exercise
Reducing Procedural Pain
The hospital has many tools to help reduce procedural pain:

Oral sucrose for infants

Pain Ease cold spray

Topical numbing creams

Needle-free J-Tip device
Children experience pain from many causes
The types of pain can be separated into the following:
- Everyday pain, such as skin scrapes and contusions, provide an opportunity for children to learn how to cope with pain.
- Short-term pain, such as ear infections or immunizations, are reported as more painful by younger children than older children.
- Recurrent pain, arises from many factors. Examples including stomachaches, headaches, and leg and back pain are reported to occur in up to 30 percent of children. There are two challenges with this type of pain:
- This type of pain may come and go unexpectedly.
- It is sometimes difficult to find the cause of this pain.
- Disease-related and chronic pain may be a symptom of an underlying problem or may occur secondary to the effects of the disease and/or treatment. Learn more about chronic pain.
Many factors can affect your child's pain
The six most significant factors are:
- Age and developmental level.
- Associated symptoms such as nausea or anxiety.
- Beliefs about the cause of the pain.
- Ability to cope with the pain.
- Previous experiences with pain .
- Observations of how others deal with pain.

Pain assessment tools are available to evaluate pain in all ages of children.
- These tools are specific to the child's age and developmental level and include the child's self-report of pain, the observations of behaviors that may indicate pain and monitoring for physical changes that may indicate pain. Routine use of these pain assessment tools help healthcare providers more effectively identify and treat pain.
- However, in children who are non-verbal or cognitively impaired, pain may be difficult to identify. In a new program called Hand In Hand Together We Can, we partner with parents and caregivers by asking about specific pain behaviors that their child may demonstrate when they are experiencing pain. This information allows us to more efficiently identify and treat pain.
Children may use coping skills to deal with pain.
- Two of the most common coping skills they use are play (distraction) and sleep. Examples of other coping skills that children may use include listening to music, playing videogames, relaxation, breathing techniques and guided imagery.
Most pain can be prevented, treated or at least reduced using a multimodal approach.
- A multimodal approach includes a combination of physical techniques (such as positioning), psychological techniques (such as deep breathing) and pharmacological techniques (including various types of medications).
Pain is dynamic and constantly changing.
- Sometimes levels of pain can change as quickly as the lights changing on a traffic light.
Spirit of Halloween
Dentistry Residency Program
How to Apply
Salaries & Benefits
Where We Work
Who We Are
JaimeEdelstein
ErnestoErdmann
JoaquinJimenezDeCardenas
List of Providers
With nearly 800 attending physicians, Nicklaus Children's Hospital has a combination of employed, contracted, and private physician practices providing services. Please refer to the lists below to find which doctors are employed or not. You may also search in more detail in our online physician directory or view the printable version of this page.
List of Employed Physicians
The following is a list of physicians employed by Nicklaus Children's Pediatric Specialists (NCPS), the physician group practice of Nicklaus Children's Health System. The benefits and coverage of the Financial Assitance Policy applies only to the doctors here listed.
Click the tab to expand.
RafaelLlanso
GabrielaSaca
EfrenSalinero
RogerStoudt
MarthaToledo-Valido
Torch Relay
VolunteerSurvey
Where We Work
Salaries & Benefits
Review-Dr-Khatib
Lice
Nursing Scholarships Home
Horizon Nurse Residency Program
 The Horizon Nurse Residency (Horizon) Program is an ANCC accredited, evidence-based nurse residency program. It’s designed to guide new graduate nurses by bridging the divide between nursing education and nursing practice. The program offers training within hospital units including the ICU setting, hematology-oncology, Emergency Department, and the ICU Float Pool, with the duration varying by unit of hire.
The Horizon Nurse Residency (Horizon) Program is an ANCC accredited, evidence-based nurse residency program. It’s designed to guide new graduate nurses by bridging the divide between nursing education and nursing practice. The program offers training within hospital units including the ICU setting, hematology-oncology, Emergency Department, and the ICU Float Pool, with the duration varying by unit of hire.
Candidate Requirements
- Be graduates of an accredited (ACEN or CCNE) BSN program
- Have a Florida RN license by the date of their panel interview
- Fulfill a two-year agreement in the unit for which they are hired, and three years within the organization
Training Styles
The Horizon Nurse Residency Program focuses on several learning styles which include:
- Didactic classes
- Skills training
- Simulation labs
- Unit-specific training with a preceptor
- Performance demonstration
- Self-learning computer modules
Expectation of Horizon Program Participants
- Obtain a certification within two years
- Author or co-author an evidence-based project or poster presentation
- Participate in a unit and/or hospital- wide committee
Photos of Horizon students during the program:
The Horizon Program selects nurse residents three
around spring, summer and/or fall.
Applications are available at: careers.nicklauschildrens.org
Applications and Deadlines
- Applications for the March 9, 2025 start date should be submitted by January 5-12, 2025.
- Applications for the July 14, 2025 start date should be submitted by May 12-18, 2025.
- Applications for the November 10, 2025 start date should be submitted by September 8-14, 2025.
Student Nurse Intern Program (SNIP)
The Student Nurse Intern Program (SNIP) provides for nursing students to be hired as care assistants to gain insight into the field of nursing. Based on availability, this program supports a smooth transition from nursing student to registered nurse by providing paid hours of mentorship in Emergency, Surgical, Medical-Surgical or Critical Care areas.
A student works alongside another care assistant while under orientation with the goal of completing a list of required competencies. Upon completion of orientation, the intern works alongside an RN and/or under the direct supervision of an RN performing delegatory-type tasks as well as patient-care skilled tasks in different pediatric areas of the hospital.
A SNIP participant will be considered a float and will be flexible with different skills to assist on the unit needed. Applicants must commit to at least one 12-hour shift every two weeks.
Eligibility Criteria includes:
- Completed at least one clinical rotation within their nursing school curriculum
- Completion of Pediatric Nursing rotation is preferred
- The SNIP program selects candidates on a yearly basis
Apply Online
Applications & Deadlines
- Applications will be accepted January 26th— February 2nd, 2025 for the March 31st, 2025 hire date.
For more information
Please contact the Christina Llanez, Nursing Excellence Manager & Magnet/Horizon Program Director.
Art of Nursing
Science of Nursing
The Nursing Department at Nicklaus Children's Hospital supports, engages, and empowers nurses to initiate nursing research, Evidence-Based Practice (EBP) projects, and quality improvement initiatives throughout the organization. Nurses at all levels of care are continuously encouraged to explore and apply the most current and best practices, as well as to generate new knowledge when an identified need arises. Integration of EBP and nursing research into clinical and operational processes aligns with the Nursing Department's commitment to provide high quality care and positive patient outcomes.
Meet Our Team

Director of Nursing Research and Evidence-Based Practice
Dr. Danielle Altares Sarik PhD, APRN, CPNP-PC directs nursing research at Nicklaus Children's Hospital. Additionally, Dr. Sarik facilitates the implementation of evidence-based practice and quality improvement projects for the nursing team. She is a Senior Fellow of the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing, and serves as Research Preceptor or Mentor for DNP and PhD students at local and national institutions. She has held Visiting Research Scholar positions at the University of Miami School of Nursing and Health Studies, and Affiliate Assistant Professor at the University of Delaware College of Health Sciences.
Dr. Sarik has research expertise in health services and outcomes research. Her research focuses on the evaluation of healthcare, with a particular emphasis on factors impacting patient safety and health outcomes, healthcare delivery, and the healthcare workforce. Key areas of interest include: pediatric health services, the transition from hospital to home, the role of advanced practice nurses, and domestic and international health policy and reform. She has served as Principle Investigator or Co-Investigator on multiple grant-funded studies, including AHRQ, Cardinal Health, National Association of Pediatric Nurse Practitioners, and ANCC. Her scholarly work has been presented internationally, and is published in interprofessional peer-reviewed journals including Hospital Pediatrics, Journal of Pediatric Healthcare, Journal of Pediatric Pharmacology and Therapeutics, and Medical Care Research and Review.
She holds a PhD, MSN and BSN from the University of Pennsylvania, and a BA from Cornell University. She is nationally certified as a Pediatric Nurse Practitioner – Primary Care by the Pediatric Nursing Certification Board, and has cared for patients in China, Botswana, and Nicaragua in additional to the US. Dr. Sarik is an active member of the National Association of Pediatric Nurse Practitioners, and she serves as a member on the Health Policy Committee.
For more information about Nursing Research and Evidence-Based Practice at Nicklaus Children's Hospital, please contact danielle.sarik@nicklaushealth.org.
Review-Dr-Dave
Pediatric Critical Care Home
shaketha-gray-adolescent-medicine
Holiday Cards
Endocrinology Home
Endocrinology Home
Endocrinology Home
danette-beitra-psychology
Craniofacial Center
Craniofacial Center
Craniofacial Center
Craniofacial Center
Conditions We Treat
Conditions We Treat
Limb Program Home
Limb Program Home
ILIZAROV Home
ILIZAROV Home
Extended Payment Plans
Nicklaus Children’s offers extended payment plans to patient families via AccessOne®. Available are no-interest and flexible low-interest payment plans that are tailored to individual financial situations. AccessOne is not a traditional credit card or collection agency. Its program covers all patient families regardless of balance or credit history. Information is never reported to a credit bureau. AccessOne customized payment options offer many benefits:
- No credit reporting
- Everyone is accepted
- No hidden fees
- Easy payment methods: online, phone, check, auto pay
- Combined statements that include other medical bills and family members
AccessOne patient advocates will work with you to determine the right plan for your situation, helping you pay in regular low-monthly installments you can realistically manage. To learn more, please speak to an AccessOne patient advocate by calling 888-458-6272 or visit the website at www.AccessOneMedCard.com
Financial Services Home
Give Miami Day
Conditions We Treat
- Conotruncal anomaly face syndrome
-
- Phelan-McDermid syndrome -22q13.3 deletion
Conditions We Treat
- Conotruncal anomaly face syndrome
-
- Phelan-McDermid syndrome -22q13.3 deletion
Conditions We Treat
- Conotruncal anomaly face syndrome
-
- Phelan-McDermid syndrome -22q13.3 deletion
Conditions We Treat
- Conotruncal anomaly face syndrome
-
- Phelan-McDermid syndrome -22q13.3 deletion
22q Clinic Home
22q Clinic Home
22q Clinic Home
22q Clinic Home
Print
Daisy Award Nomination
The DAISY (Diseases Attacking the Immune System) Award is an international recognition program that honors and celebrates the skillful, compassionate care nurses provide every day.
The DAISY Foundation was established by the family of J. Patrick Barnes after he died from complications of the auto-immune disease ITP in 1999. During his hospitalization, they deeply appreciated the care and compassion shown to Patrick and his entire family. When he died, they felt compelled to say “thank you” to nurses in a very public way. Please say thank you by sharing your story of how a nurse made a difference you will never forget!
Fill out the Nomination Form
If you have any questions, please contact Miosotis Falcon at 786-624-3320 or via email at Miosotis.Falcon@Nicklaushealth.org.
Articles
GoogleReviews
YelpReviews
Healthgrades
Programs
Administrative Leadership
Nicklaus Children's Health System Administrative Leadership
thomas-errico-orthopedic-surgery
Board of Directors
Leadership
Accepted Insurance Providers
The Nicklaus Children's Dental Program accepts the following health insurance plans:
Government Insurance plans
- DentaQuest- Medicaid
- DentaQuest- Florida Healthy Kids (FHK)
- MCNA- Medicaid
- MCNA- Florida Healthy Kids (FHK)
- Liberty- (Medicaid)
- Liberty- Wellcare (FHK)
PPO Insurance plans
- Aetna PPO(Out of Network)
- Assurant PPO
- Cigna PPO
- United Concordia PPO
- Delta PPO
- Metlife PPO
Providers List
Press CTRL + P on your keyboard to print this page.
Rheumatology Home
Patient Education Videos
Medical Staff Gala 2019 - RSVP
You and a guest are cordially invited to join us at a
Winter Wonderland
The 19th Annual Medical Staff Gala
Saturday, March 2, 2019
Cocktail Reception – 7:30 PM
Dinner – 8:00 PM
Diplomat Beach Resort – Great Hall
Convention Center – 3rd Floor
3555 South Ocean Drive Hollywood, FL 33019
Formal Attire
Prenatal Cardiology Home
Prenatal Cardiology Home
Prenatal Cardiology Home
Mix and Mingle
RSVP - Global
Por favor llene el formulario para confirmar su asistencia.

Appointment Options
Discharge Instructions
Programs and Clinics
Videos
Meet the Team
Our staff that is trained and dedicated to the care of infants and children. The department is staffed by specialists in all radiology fields. These experts work together with clinical sub-specialists and attending physicians to support the care of infants and children.
CarSeats
Billing and Collections Policy
Scope
System-wide: The Nicklaus Children’s Health System, comprised of Nicklaus Children's Hospital, Nicklaus Children's Hospital Foundation, Nicklaus Children's Pediatric Specialists (formerly Pediatric Specialists of America), other NCHS entities and all employees and contractors of those entities.
Purpose
To ensure Patient Financial Services appropriately uses staff resources and supports the hospital finance department in the accurate and timely reporting of patient Accounts Receivable by transferring uncollectible accounts to bad debt in a timely manner and (if necessary) primary and secondary collection agency activity-only after Nicklaus Children’s Hospital (NCH) makes reasonable efforts to determine whether an individual is eligible for financial assistance under its Financial Assistance Policy (FAP).
Policy
All patient balances generated after time of service for either non-insured patients or insured patients with remaining financial responsibility will be handled in accordance with this policy.
Procedure
- AGB – Amounts generally billed for emergency or other medically necessary care to individuals who have insurance coverage.
- Application Period – means the period during which NCH must accept and process an application for financial assistance under its FAP in order to have made reasonable efforts to determine whether the individual is FAP-eligible. The Application Period begins on the date the caere is provided to the individual and ends on the later of the 240th day after the date that first post-discharge billing statement for the care is provided or at least 30 days after NCH provides the individual with a written notice that sets a deadline after which ECA’s may be initiated.
- ECA’s – Extraordinary Collection Actions are actions taken by NCH against an individual related to obtaining payment of a bill for care covered under NCH’s FAP that require a legal or judicial process or involve selling an individual’s debt to another party or reporting adverse information about the individual to consumer credit reporting agencies or credit bureaus.
- FAP – NCH’s Financial Assistance Policy
- FAP Contact Information – Nicklaus Children’s Hospital Customer Care Center, 9655 N.W. 33 Street, Miami, FL 33172 (888) 538-3036.
- FAP-Eligible Individual – An individual eligible for financial assistance under NCH’s FAP (without regard to whether the individual has applied for assistance under the FAP).
Collection Actions
It is the policy of NCH not to engage in ECA’s against an individual to obtain payment for care before making reasonable efforts to determine whether the individual is eligible for assistance under its FAP.
Subject to the guidelines set forth herein, NCH patient accounts may be subject to the following collection actions:
- Following the initial bill, monthly statements and collection letters are mailed and phone calls are completed in an effort to collect all outstanding balances due.
- Subject to the provisions set forth herein, patient balances generated after time of service for either uninsured or insured patients with remaining financial responsibility may be transferred to a bad debt collection agency within 180 days of discharge. If accounts remain unpaid with 365 days of discharge, they may be placed with a secondary collection agency vendor for further collection efforts.
- ECA’s that may be utilized by NCH (or other authorized party), subject to the provisions set forth herein, include:
- Reporting adverse information about the individual to consumer credit reporting agencies or credit bureaus;
- Commencing a civil action against an individual. Commencement of a civil action will be determined on a case-by-case basis. Legal approval can only be authorized in writing by the Director, Patient Financial Services, or his/her designee.
- NCH will take the following actions at least 30 days before first initiating one or more of the above ECA(s) to obtain payment for care:
- Provide the individual with a written notice that indicates financial assistance is available for eligible individuals, identify the ECA(s) that NCH (or other authorized party) intends to initiate to obtain payment for the care, and state a deadline after which such ECA(s) may be initiated that is no earlier than 30 days after the date that the written notice is provided.
- Provide the individual with a plain language summary of the FAP with the written notice described above.
- Make a reasonable effort to orally notify the individual about NCH’s FAP and about how the individual may obtain assistance with the FAP application process.
- If NCH aggregates an individual’s outstanding bills for multiple episodes of care before initiating one or more ECA’s to obtain payment for those bills, it will refrain from initiating the ECA(s) until 120 days after it provided the first post-discharge billing statement for the most recent episode of care included in the aggregation.
- If NCH defers or denies, or requires a payment before providing, medically necessary care to an individual with one or more outstanding bills for previously provided care, NCH will provide the individual with a FAP application form and a written notice indicating that financial assistance is available for eligible individuals and stating the deadline, if any, after which NCH will no longer accept and process a FAP application submitted (or, if applicable, completed) by the individual for the previously-provided care. The deadline will be no earlier that the later of 30 days after the date that the written notice is provided or 240 days after the date that the first post-discharge billing statement for the previously-provided care was provided. NCH will also provide the individual with a plain language summary of the FAP with the written notice, and make a reasonable effort to orally notify the individual about NCH’s FAP and about how the individual may obtain assistance with the FAP application process. If a FAP application is timely received by NCH, it will process the application on an expedited basis.
Determining Financial Assistance Eligibility
NCH will make reasonable efforts to determine whether individuals are eligible for financial assistance as follows:
- Notify individuals about the FAP before initiating any ECA’s to obtain payment for the care and refrain from initiating such ECA’s for at least 120 days from the date NCH provides the first post-discharge billing statement for the care;
- In the case of an individual who submits an incomplete FAP application during the Application Period, notify the individual about how to complete the FAP application and give the individual a reasonable opportunity to do so as described herein; and
- In the case of an individual who submits a complete FAP application during the Application Period, determine whether the individual is FAP-eligible for the care and otherwise meets the requirements described herein.
NCH will process FAP applications in accordance with the provisions set forth below.
Processing FAP Applications
Submission of Complete FAP Application
- If an individual submits a complete FAP application during the Application Period, NCH will:
- Suspend any ECA’s against the individual (with respect to charges to which the FAP application under review relates);
- Make a determination as to whether the individual is FAP-eligible and notify the individual in writing of the eligibility determination (including, if applicable, the assistance for which the individual is eligible) and the basis for this determination;
- If NCH determines the individual is FAP-eligible, NCH will:
- Provide the individual with a billing statement that indicates the amount the individual owes for the care as a FAP-eligible individual (assuming the individual is eligible for assistance other than free care) and how that amount was determined and states, or describes how the individual can get information regarding, the AGB for the care.
- Refund to the individual any amount he or she has paid for the care (whether to the hospital facility or any other party to whom the hospital facility has referred or sold the individual’s debt for the care) that exceeds the amount he or she is determined to be personally responsible for paying as a FAP-eligible individual, unless such excess amount is less that $5 (or such other amount published in the Internal Revenue Bulletin).
- Take all reasonably available measures to reverse any ECA (with the exception of a sale of debt) taken against the individual to obtain payment for the care.
If the provisions of Section 1 above are met, and NCH has not violated the anti-abuse rule described below, NCH may initiate or resume ECA’s against the individual.
If, upon receiving a complete FAP application from an individual who NCH believes may qualify for Medicaid, NCH may postpone determining whether the individual is FAP-eligible for the care until after the individual’s Medicaid application has been completed and submitted and a determination as to the individual’s Medicaid eligibility has been made.
Submission of Incomplete FAP Application
If an individual submits an incomplete FAP application during the Application Period, NCH will:
- Suspend any ECA’s against the individual (with respect to charges to which the FAP application under review relates);
- Provide the individual with a written notice that describes the additional information and/or documentation required under the FAP or FAP application form that the individual must submit to NCH to complete his/her FAP application and includes the FAP Contact Information with the notice.
- If an individual who has submitted an incomplete FAP application during the Application Period subsequently completes the FAP application during the Application Period (or, if later, within a reasonable timeframe given to respond to requests for additional information and/or documentation), the individual will be considered to have submitted a complete FAP application during the Application Period.
Failure to Submit FAP Application
Unless and until NCH receives a FAP application from an individual during the Application Period, NCH may initiate ECA’s to obtain payment for the care once it has notified the individual about the FAP as described herein.
Miscellaneous Provisions
Anti-Abuse Rule – NCH will not base its determination that an individual is not FAP-eligible on information that NCH has reason to believe is unreliable or incorrect or on information obtained from the individual under duress or through the use of coercive practices.
No Waiver of FAP Application – NCH will not seek to obtain a signed waiver from any individual stating that the individual does not wish to apply for assistance under the FAP, or receive the information described above, in order to determine that the individual is not FAP-eligible.
Final Authority for Determining FAP Eligibility - Final authority for determining that NCH has made reasonable efforts to determine whether an individual is FAP eligible and may therefore engage in ECA’s against the individual rests with the Patient Financial Services Department.
Agreements with Other Parties - If NCH sells or refers an individual’s debt related to care to another party, NCH will enter into a legally binding written agreement with the party that is reasonably designed to ensure that no ECA’s are taken to obtain payment for the care until reasonable efforts have been made to determine whether the individual is FAP-eligible for the care.
Providing Documents Electronically - NCH may provide any written notice or communication described in this policy electronically (for example, by email) to any individual who indicates he or she prefers to receive the written notice or communication electronically.
Morton and Linda Bouchard Healing Garden
The Morton and Linda Bouchard Healing Garden is a space that promotes health and healing at Nicklaus Children’s Hospital. The garden, which is located in an outdoor courtyard within the hospital’s Advanced Pediatric Care Pavilion, provides hospitalized patients and families a quiet space for meditation and respite. Its colorful botanicals, topiaries and dynamic video wall, featuring calming outdoor scenes, combined with the fresh air, enables patients and families to step out of the medical setting into a comfortable zone that complements the recovery process.
Visiting the Morton and Linda Bouchard Healing Garden
- Patients and families coming from the Central Building can use the access entrance that connects from the second floor to the Bed Tower. The badge access to this entrance will be deactivated during the hours of operation for patients and families to access the Healing Garden. Please refer to the hospital map for additional direction information.
- Intercoms have been placed on the east entrance of each unit by the door that connects the Central Building on the second hall of each unit. Patients and families can conveniently access these intercoms to re-enter their unit;from the Healing Garden.
- The Healing Garden is an unsupervised common area monitored by security cameras. Therefore, no child should be left unattended in the Healing Garden. Each child should be accompanied by a parent, a hospital staff member, or a hospital volunteer.
Our Donors
The Healing Garden is made possible through the generosity of Morton and Linda Bouchard as well as Jack and Barbara Nicklaus of the Nicklaus Children’s Health Care Foundation.
Mural
The mural was painted by artist Seth Globepainter and made possible through the generosity of Goldman Global Arts and Jessica Goldman Srebnick.
Request a Second Opinion
What is a Second Opinion?
A second opinion for medical procedures is a consultation from a second physician on a treatment protocol for added reassurance and quality of care.
Why a Second Opinion for Pediatric Surgery?
Pediatric surgery is an important decision – the outcomes can often be life-changing for the child and their family.
At Nicklaus Children's Hospital, our team of physicians and surgeons provide and encourage second opinions.
Second Opinions are a Good Thing
Families often hesitate to reach out to other physicians for second opinions fearing they'll upset the relationship they've established with their current physician or surgeon.
In cases where procedures or surgeries may be sensitive, or potentially life-threatening, second opinions from trusted and recognized medical professionals can make a significant impact in successful surgical results.
A second opinion will allow you as a family to make an informed medical decision for your child by evaluating if the second opinion complements, or differs entirely, from the original treatment plan. In certain cases, a third opinion may even be advisable.
You Have a Right to a Second Opinion
In the state of Florida, patients are entitled to receive insurance coverage for second opinions for certain medical conditions and surgical procedures. In fact, Florida is one of the few states that protects patients in this manner. Learn more about FL 641.51 statute.
Second Opinion Appointments are a Little Different
When you call our Customer Care Department at 1-888-624-2778, our representatives will ask you what type of appointment you're scheduling, and if your appointment is for a second opinion, they'll promptly route you to the appropriate Department or Practice for immediate scheduling.
You can also request second opinion appointments by completing our online form.
Request a Second Opinion
What You Need to Bring
When rush appointments are needed, typically within 24-48 hours, it is vital that the following documentation, (if applicable to your child's surgery or procedure), is brought to the appointment:
- Medical History
- X-Rays or MRI Results
- Lab Results
- Growth Chart
- Insurance Requirements such as prescriptions, referrals, or authorizations
- Any other information relevant to your child's procedure or surgery
What to Expect During Your Visit
One of our physicians or surgeons will review your child's medical history and all previous testing. They may recommend additional testing, or consult with a Nicklaus Children's physician from a different specialty.
Why Nicklaus Children's Hospital?
Whether you choose a Nicklaus Children's Hospital physician for your child's surgery, or you simply need a second opinion for added reassurance of your original treatment plan, our focus is superior patient experience.
We are South Florida's only licensed specialty hospital exclusively for children, with nearly 800 attending physicians, including more than 475 pediatric subspecialists. Our 307-bed hospital is renowned for excellence in all aspects of pediatric medicine with many specialty programs routinely ranked among the best in the nation by U.S. News & World Report since 2008. Nicklaus Children's Hospital is also home to the largest pediatric teaching program in the southeastern United States and has been designated an American Nurses Credentialing Center (ANCC) Magnet facility, the nursing profession's most prestigious institutional honor.
We're ready to be your trusted partner in your family's healthcare journey.
Second Opinion
Advanced Pediatric Care Pavilion
The Advanced Pediatric Care Pavilion (APCP) at Nicklaus Children’s Hospital is a six-story, 213,000-square-foot bed tower that houses the hospital’s critical care offerings and an enhanced care environment for the pediatric population. Of the hospital’s 307 beds, 189 are located in the new tower.
Service offerings by floors:

Family-Centric Amenities
- Several family lounges are available to families throughout the tower and a teen lounge is located on the 6th floor.
- Each floor features spacious family-centric rooms with parental accommodations for sleeping and showering.
- Americans with Disabilities Act (ADA) compliant rooms and restrooms.
- Play spaces equipped for play to support the healing process in hospitalized children and siblings.
- Hair wash stations in the neurology/neurosurgery unit.
State-of-the-Art Medical Innovation
Intraoperative MRI:
Located on the second floor of the pavilion, the intraoperative MRI (iMRI) is mounted on a rail system that allows the equipment to be brought into a specialized neurosurgical suite. The use of the iMRI during surgery improves the completeness of tumor removal, offering the best possible outcomes in the hands of the hospital’s highly skilled neurosurgeons.
Blood and Marrow Transplant Unit:
Located on the sixth floor, this unit will house patients who have undergone blood or marrow transplants while they rebuild their body’s immune systems.
Steris Booms:
These ceiling mounted devices support the provision of minor procedures within the PICU and feature connectivity to lights, power, oxygen and monitoring devices.
eSignage:
Electronic, touch screen LCD panel signs located outside of patient rooms convey isolation precautions to be addressed by staff and persons entering the room.
Pneumatic Tube:
This tube delivery system transports lab specimens and prescription medications between the hospital floors and the lab or pharmacy.
GetWellNetwork:
Located in each room on a large screen, the GetWellNetwork provides parents with electronic information about their child’s stay, including prescription information, educational resources, meal ordering and discharge instructions. Patients and families can also video conference with doctors, specialists and family members through the GetWellNetwork.
Smart Beds with Exit Alarms:
These new state-of-theart beds offer heightened patient protection, notifying staff if patients should attempt to exit the bed without assistance. These technologies support the hospital’s world-famous Humpty Dumpty Falls Prevention Program™ and its philosophies.
Mobile Healthcare Apps:
These provide staff the ability to be constantly connected and aligned through the latest communications and hand-off technology.
Ambiance for healing
- Interior spaces feature inspiring images photographed by South Florida artists that were selected by children and families.
- Images and color schemes help illustrate the individual themes for the various tower floors: Earth, Water, Sun, Air, and Universe.
- Wall frames feature patient artwork, giving children the opportunity to leave their artistic mark on the hospital during their stay.
Advanced Pediatric Care Pavilion
The Advanced Pediatric Care Pavilion (APCP) at Nicklaus Children’s Hospital is a six-story, 213,000-square-foot bed tower that houses the hospital’s critical care offerings and an enhanced care environment for the pediatric population. Of the hospital’s 307 beds, 189 are located in the new tower.
Service offerings by floors:

Family-Centric Amenities
- Several family lounges are available to families throughout the tower and a teen lounge is located on the 6th floor.
- Each floor features spacious family-centric rooms with parental accommodations for sleeping and showering.
- Americans with Disabilities Act (ADA) compliant rooms and restrooms.
- Play spaces equipped for play to support the healing process in hospitalized children and siblings.
- Hair wash stations in the neurology/neurosurgery unit.
State-of-the-Art Medical Innovation
Intraoperative MRI:
Located on the second floor of the pavilion, the intraoperative MRI (iMRI) is mounted on a rail system that allows the equipment to be brought into a specialized neurosurgical suite. The use of the iMRI during surgery improves the completeness of tumor removal, offering the best possible outcomes in the hands of the hospital’s highly skilled neurosurgeons.
Blood and Marrow Transplant Unit:
Located on the sixth floor, this unit will house patients who have undergone blood or marrow transplants while they rebuild their body’s immune systems.
Steris Booms:
These ceiling mounted devices support the provision of minor procedures within the PICU and feature connectivity to lights, power, oxygen and monitoring devices.
eSignage:
Electronic, touch screen LCD panel signs located outside of patient rooms convey isolation precautions to be addressed by staff and persons entering the room.
Pneumatic Tube:
This tube delivery system transports lab specimens and prescription medications between the hospital floors and the lab or pharmacy.
GetWellNetwork:
Located in each room on a large screen, the GetWellNetwork provides parents with electronic information about their child’s stay, including prescription information, educational resources, meal ordering and discharge instructions. Patients and families can also video conference with doctors, specialists and family members through the GetWellNetwork.
Smart Beds with Exit Alarms:
These new state-of-theart beds offer heightened patient protection, notifying staff if patients should attempt to exit the bed without assistance. These technologies support the hospital’s world-famous Humpty Dumpty Falls Prevention Program™ and its philosophies.
Mobile Healthcare Apps:
These provide staff the ability to be constantly connected and aligned through the latest communications and hand-off technology.
Ambiance for healing
- Interior spaces feature inspiring images photographed by South Florida artists that were selected by children and families.
- Images and color schemes help illustrate the individual themes for the various tower floors: Earth, Water, Sun, Air, and Universe.
- Wall frames feature patient artwork, giving children the opportunity to leave their artistic mark on the hospital during their stay.
Second Opinions
Second Opinions are a Good Thing
Families often hesitate to reach out to other physicians for second opinions fearing they'll upset the relationship they've established with their current physician or surgeon.
In cases where procedures or surgeries may be sensitive, or potentially life-threatening, second opinions from trusted and recognized medical professionals can make a significant impact in successful surgical results.
A second opinion will allow you as a family to make an informed medical decision for your child by evaluating if the second opinion complements, or differs entirely, from the original treatment plan. In certain cases, a third opinion may even be advisable.
You Have a Right to a Second Opinion
In the state of Florida, patients are entitled to receive insurance coverage for second opinions for certain medical conditions and surgical procedures. In fact, Florida is one of the few states that protects patients in this manner. Learn more about FL 641.51 statute.
Second Opinion Appointments are a Little Different
When you call our Customer Care Department at 1-888-624-2778, our representatives will ask you what type of appointment you're scheduling, and if your appointment is for a second opinion, they'll promptly route you to the appropriate Department or Practice for immediate scheduling.
You can also request second opinion appointments by completing our online form.
Request a Second Opinion
What You Need to Bring
When rush appointments are needed, typically within 24-48 hours, it is vital that the following documentation, (if applicable to your child's surgery or procedure), is brought to the appointment:
- Medical History
- X-Rays or MRI Results
- Lab Results
- Growth Chart
- Insurance Requirements such as prescriptions, referrals, or authorizations
- Any other information relevant to your child's procedure or surgery
What to Expect During Your Visit
One of our physicians or surgeons will review your child's medical history and all previous testing. They may recommend additional testing, or consult with a Nicklaus Children's physician from a different specialty.
Why Nicklaus Children's Hospital?
Whether you choose a Nicklaus Children's Hospital physician for your child's surgery, or you simply need a second opinion for added reassurance of your original treatment plan, our focus is superior patient experience. We are South Florida's only licensed specialty hospital exclusively for children, with nearly 800 attending physicians, including more than 475 pediatric subspecialists. Our 307-bed hospital is renowned for excellence in all aspects of pediatric medicine with many specialty programs routinely ranked among the best in the nation by U.S. News & World Report since 2008. Nicklaus Children's Hospital is also home to the largest pediatric teaching program in the southeastern United States and has been designated an American Nurses Credentialing Center (ANCC) Magnet facility, the nursing profession's most prestigious institutional honor.
We're ready to be your trusted partner in your family's healthcare journey.
Alan W Smith
Outcomes Reporting Project
Committed to Transparency in Our Cardiac Surgical Results
The Heart Institute at Nicklaus Children’s Hospital has a longstanding commitment to transparency in our clinical outcomes. We believe that patients and parents should have access to validated clinical data in order to make informed decisions regarding pediatric care, and that publicly reporting data is a powerful incentive to quality improvement in care.
In 2001, our Cardiac Program began publishing clinical results on the Internet. In 2013, with more advanced reporting capabilities, we launched an initiative to replace the previous public reporting. We reverse engineered the Society of Thoracic Congenital database queries and inclusion/exclusion criteria in order to provide real time surgical results.
Today, our Real Time Outcome Report replicates the Society of Thoracic Surgeons (STS) results. We then validate the results by hand when the biannual STS report is released. The Real Time Outcomes Report sources dynamic data daily from the directly from the Cardioaccess database. We include non-risk adjusted mortality as well as length of postoperative stay. We believe postoperative length of stay is a surrogate marker for complications and excellence of outcomes: our median Norwood length of stay of 16 days versus the STS length of stay of 49 days indicates a very low incidence of tracheostomy, gastrostomy, or neurological complications. Results are posted electronically and only validated for accuracy without additional editing.
Julio-Barredo
Landing Pages
Planning for Parenthood
seth-crapp
Sarcoma and Solid Tumor Program
saima-aftab
Pediatric Echocardiogram Protocol
Subcostal
- Abdominal Situs (Left & Right Sweep)
Subcostal Long Axis
- 2D/Color Sweep color compare
- 2D/Color Atrial Septum Sweep (Optimize image to focus on septum with narrowing sector width and increase depth/zoom)
Subcostal Short Axis
- 2D/Color Sweep color compare (Beginning at IVC/SVC to LV apex)
- 2D FXN RV & LV (Optimize image/Zoom, Can be used for Area Measurement)
- Descending Aorta color compare/ PW
- 2D/Color compare IVC sweep to level of kidney
Apical
- 2D/Color Sweep Ventricular Septum color compare (Posterior to Anterior sweep) Clip 1 Clip 2
- 2D/Color compare Pulmonary Valve (RVOT)/CW
- 2D/Color compare Tricuspid Valve/ CW
- 2D/Color compare Mitral Valve/ CW
- 2D Left Ventricle (Volume length measurement)
- 2D/Color compare Aortic Valve (Apical 5 Chamber)/CW
- Tissue Doppler, LA volumes and PW MV E/A wave Doppler must be obtained for patients with Hypertension, Cardiomyopathy or Sickle Cell Anemia
Parasternal Long Axis
- 2D/Color sweep color compare (Color box covering membranous septum sweep posteriorly to Tricuspid valve then anteriorly to Pulmonary valve) Clip 1 Clip 2
- 2D/Color compare Pulmonary valve/CW
- 2D/Color compare MV/Aorta
- 2D Aorta Measurements (Aortic annulus, Root, Sino tubular junction and Ascending aorta) *Ascending aorta must be measured at level of Right Pulmonary artery. Can be measured in Ductal view
Parasternal Short Axis
- 2D/Color Sweep Ventricular Septum color compare (Starting at the level of the Aortic valve to the LV apex)
- 2D/Color compare Pulmonary Arteries, Pulmonary Valve/CW
- 2D FXN Left Ventricle (Level of the Papillary muscles for area measurements)
- 2D FXN Left ventricle (Level of the LV apex to look for Hypertrabeculations)
- M-Mode (FS%)
- 2D/Color compare Aortic Valve (Valve leaflet interrogation)
- 2D/Color compare Coronary Arteries (Right and Left Coronary arteries)
- 2D/Color compare Coronary Artery sweep (Color box placed between the Right and Left aortic leaflet. Superior sweep from Aortic valve to Ascending Aorta)
Suprasternal
- 2D/Color compare Ductal sweep (Sweeping from Ascending Aorta to the LPA/Descending Aorta connection. Ascending Aorta measurement can be obtained here. Measure above the level of Right Pulmonary artery)
- 2D/Color compare Left Pulmonary Veins
- 2D/Color compare Right Pulmonary Veins (Right Upper Pulmonary view can also be obtained in the Subcostal short axis view or High Right Parasternal view)
- 2D/Color compare Aortic Arch branching
- 2D/Color compare Aortic arch /CW Proximal Descending Aorta
Quantification
- Left ventricular size & Function Quantification (M-Mode/Bullet method)
- Mitral & Tricuspid valve (Apical 4 view)
- Pulmonary Valve (PLAX)
- Aortic Annulus, Root, Sino Tubular Junction and Ascending Aorta (PLAX) * Ascending Aorta can be measured in Ductal view above the Right Pulmonary Artery
2D/Color compare Aortic arch /CW Proximal Descending AortaKangaroo Care-a-thon
Events Listing
Fetal Care VIP
Insurance List
Enrich
ENRICH Literacy Program
The ENRICH Literacy Program was created in collaboration with clinicians to educate and empower all parents to engage, nurture, and read to infants and children. The program provides resources for parents and educators in our community to increase literacy rates from birth and beyond.
ENRICH aligns with our Nicklaus Children’s Health System mission
“Where your child matters most”
Easy steps to promote literacy from infancy
- Name body parts and the clothing as you are dressing your baby.
- Name foods and talk about the colors of food when you are eating.
- Narrate the story of changing your child’s diaper – explain to your child what you are doing.
- When it’s time to take a bath - sing songs.
- Use a variety of voices for different characters when reading a story.
- Use a mirror to show facial expressions while interacting with your baby.
- While grocery shopping, talk to your baby about the colors, shapes, and sizes of the food you are purchasing.
 ENRICH School Clubs
ENRICH School Clubs
The
ENRICH School Club is our education outreach program. ENRICH School Clubs are eligible to receive books or funding towards ENRICH book purchases, and will have an opportunity to host a Special Event at Nicklaus Children’s Hospital. ENRICH School Clubs must follow an approved book list to receive funding. ENRICH School Club applications are subject to approval by the ENRICH Steering Committee.
How You Can Help
The ENRICH Literacy Program is funded through the generosity of donors like you. The following donation options are available:
- $55 – Baby’s First Bilingual Library
- $50 – Donate 10 new books to ENRICH
- $100 – Donate 25 new books to ENRICH
- Other Donation Amount of your choice
Donate NowBlackbaud test
Fundraising Ideas
Liasion Report
MSL
Patient Stories
Patient Stories
Survivorship Program Home
Survivorship Program Home
BMT Program Home
BMT Program Home
Neuro-Oncology Center Home
Neuro-Oncology Center Home
Neuro-Oncology Center Home
Neuro-Oncology Center Home
Conditions we Treat
Conditions we Treat
Conditions we Treat
Conditions we Treat
Support Services for Patients and Families
Inpatient Care
Children who are hospitalized during the course of their care receive treatment and support in Nicklaus Children's 28-bed dedicated Hematology/Oncology Unit. Patient rooms feature cheerful décor and have been specially designed for patients with weakened immune systems to minimize the risk of infection.
During their stay, children experience the special environment of a dedicated children's hospital, where all care and support personnel are experienced in meeting the needs of sick children.
Highlights include:
What's more, children meet and mingle with other youngsters with similar health issues, often developing lasting bonds that help sustain them throughout their care and recovery.
Families of children at Nicklaus Children's also benefit from the Michael Fux Family Center. This facility serves as a home away from home, offering basic comforts such as showers and laundry facilities, as well as stress relievers, including a small workout gym and massage room, and dazzling family entertainment facilities, including a movie theater and libraries.
Outpatient Infusion Services
The Shaham Cancer and Blood Disorders Institute's infusion center, is a family-centered service designed to provide infusion therapy and short-stay treatments, including chemotherapies and blood transfusions.
The infusion center is a pleasant, comfortable space where children can play, relax and even nap while receiving infusion therapy. The infusion center also provides a setting where children can interact with young people with similar diagnoses. And parents can meet and gain support from other parents in comparable circumstances.
(Children with marked immunosuppression are properly isolated for their protection.)
Pharmacological Services
The Shaham Cancer & Blood Disorders Institute team includes a dedicated clinical pharmacist from the Nicklaus Children's Hospital Pharmacy, who is assigned exclusively to support patients from the Center.
The pharmacist provides patient care recommendations on pharmacotherapy and assesses drug interactions, drug dosages, and drug effects. They accompany the Institute's team on daily rounds and provide counseling to families of patients regarding medication use and administration. They also help with the transition to home care, ensuring that each patient has appropriate medications when leaving the hospital.
The pharmacist is just a phone call away for parents once they are home, providing ongoing support with medications, as needed. The provision of a clinical pharmacist to serve the Institute offers a continuum of care for patients, ensuring that a specialist familiar with each child's unique needs and physiological response is available throughout the course of treatment.
In addition, the hospital's Outpatient Pharmacy supports the Institute by stocking the highly specialized drugs required for the care of cancer patients. The Institute also coordinates the selective use and storage of National Cancer Institute research drugs.
Social Services
Due to the enormous impact a cancer diagnosis has in the life of a patient and his or her family, a team of social workers is an integral part of the cancer support services offered by the Shaham Cancer & Blood Disorders Institute at Nicklaus Children's Hospital.
A social worker is present when the family first meets with the physician to discuss the diagnosis and continues to play a supportive, clinical role throughout the child's treatment. Social workers participate in weekly multidisciplinary meetings to review the care plan of each hospitalized child. Social workers also work individually with patients, parents, siblings and extended family members, assisting them in their adjustment process to illness and hospitalization. When indicated, social workers consult closely with psychiatrists and behavioral medicine specialists for additional clinical interventions.
The social work team facilitates diverse parent support groups and refers families for other cancer support services, such as financial, housing, transportation, day-care and bereavement-related services as needed.
Psychiatric and Psychological Services
Child and adolescent psychiatric consultation is part of an integrated, comprehensive evaluation of many hematology/oncology patients. Chronic pediatric illness of almost any kind with recurrent hospitalization is a psychological risk factor for children. The rate of psychiatric illness in children with both chronic medical conditions and disability is three times greater than non-compromised children.
Every child with a pediatric illness requiring hospitalization experiences a psychological reaction. The degree of reaction varies with the developmental level and the level of function prior to illness, as well as the state and reaction of the family and the severity of the illness. The divisions of Psychiatry and Behavioral Medicine at Nicklaus Children's Hospital offer individual therapy for the patient, family therapy and participate in the patient and family support groups.
Volunteer Services
Volunteer organizations are the lifeblood of any institution. The Shaham Cancer & Blood Disorders Institute, is fortunate to have the support of the United Order True Sisters, Miami #43, since 1958. This entity has a long tradition of providing support services to our cancer and blood disorder patients, including sponsorship of the annual summer cancer camp.
Annual Celebrations
A holiday party in December brings children with cancer together to celebrate the joys of the season with staff and friends and acquaintances from the hospital. A cancer survivor's day celebration is held each June, with dozens of patients and their families in attendance.
Patient Stories
Advanced Treatments and Procedures
Specialist Programs and Clinics
Latest News
Conditions We Treat
Cancer & Blood Disorders Institute Home
Cancer & Blood Disorders Institute Home
Cancer & Blood Disorders Institute Home
Videos
Conditions we Treat
Conditions we Treat
Hemophilia Center Home
Hemophilia Center Home
Patient Stories
Patient Stories
Patient Education
Sickle cell disease is a group of inherited red blood cells disorders. People who have sickle cell disease have an abnormal protein in their red blood cells. In the United States, most people who have sickle cell disease are of African ancestry, but the condition is also common in people with a Hispanic background. Because the disease runs in families, couples planning to have children can have genetic testing.
Early signs and symptoms of sickle cell disease include swelling of the hands and feet; symptoms of anemia, including fatigue, or extreme tiredness; and jaundice. Over time, sickle cell disease can lead to complications such as infections, delayed growth, and episodes of pain, called pain crises. Most children who have sickle cell disease are pain-free between crises, but adolescents and adults may also suffer with chronic, ongoing pain. Over a lifetime, sickle cell disease can harm a patient’s spleen, brain, eyes, lungs, liver, heart, kidneys, penis, joints, bones, or skin.
A blood and bone marrow transplant is currently the only cure for sickle cell disease, and only a small number of people who have sickle disease are able to have the transplant. There are effective treatments that can reduce symptoms and prolong life. Early diagnosis and regular medical care to prevent complications also contribute to improved well-being. Sickle cell disease is a life-long illness. The severity of the disease varies widely from person to person.
Infographics
Explore this Health Topic to learn more about sickle cell disease, our role in research and clinical trials to improve health, and where to find more information.
Patient Education
Sickle cell disease is a group of inherited red blood cells disorders. People who have sickle cell disease have an abnormal protein in their red blood cells. In the United States, most people who have sickle cell disease are of African ancestry, but the condition is also common in people with a Hispanic background. Because the disease runs in families, couples planning to have children can have genetic testing.
Early signs and symptoms of sickle cell disease include swelling of the hands and feet; symptoms of anemia, including fatigue, or extreme tiredness; and jaundice. Over time, sickle cell disease can lead to complications such as infections, delayed growth, and episodes of pain, called pain crises. Most children who have sickle cell disease are pain-free between crises, but adolescents and adults may also suffer with chronic, ongoing pain. Over a lifetime, sickle cell disease can harm a patient’s spleen, brain, eyes, lungs, liver, heart, kidneys, penis, joints, bones, or skin.
A blood and bone marrow transplant is currently the only cure for sickle cell disease, and only a small number of people who have sickle disease are able to have the transplant. There are effective treatments that can reduce symptoms and prolong life. Early diagnosis and regular medical care to prevent complications also contribute to improved well-being. Sickle cell disease is a life-long illness. The severity of the disease varies widely from person to person.
Infographics
Explore this Health Topic to learn more about sickle cell disease, our role in research and clinical trials to improve health, and where to find more information.
Conditions we Treat
Conditions we Treat
Sickle Cell Program (Home)
Sickle Cell Program (Home)
Patient Stories
Conditions we Treat
Dermatology Home
Conditions we Treat
Conditions we Treat
Locations
Nicklaus Children's has several outpatient centers and urgent care centers in Miami to meet the needs of your child. Browse our convenient locations and find directions for your visit.
Virtual Tours
Take a virtual walk of our hospital campus and outpatient facilities.
Virtual Tours
Take a virtual walk of our hospital campus and outpatient facilities.
Virtual Tours
Take a virtual walk of our hospital campus and outpatient facilities.
Primary Care Centers
{$ NCH.Locations.PCCServices $}{$ NCH.Locations.Insurance $}

Pediatric Care Locations
Urgent Care Centers
Outpatient Centers
Outpatient Services
As part of Nicklaus Children's commitment to enhancing service convenience for South Florida families, the hospital has developed several outpatient centers featuring select pediatric services for babies, children, teens and young adults under 21 years old, such as:
- Personalized and prompt care provided by board-certified pediatric physicians, including specialty consultations by appointment.
- Diagnostic services, including walk-in X-ray. Select locations offer MRI and ultrasound. All diagnostic services require a prescription.
- Rehabilitation services for infants, children and teens such as physical, occupational, speech-language, and feeding and swallowing therapies – provided on weekdays by appointment during standard medical office hours.
- Walk-in urgent care, select locations offer urgent care for minor injuries and illnesses from 11 a.m. to 10 p.m daily. Check the wait times.
{$ NCH.Locations.Insurance $}
Urgent Care Locations
Swimming Instruction and Water Safety Program
 At the Nicklaus Children's Dan Marino Outpatient Center, we proudly provide swimming and safety programs. Our swimming pool is enclosed and heated for year-round comfort. Teaching plans are individualized and all children, including infants and children with special needs, will be able to learn.
At the Nicklaus Children's Dan Marino Outpatient Center, we proudly provide swimming and safety programs. Our swimming pool is enclosed and heated for year-round comfort. Teaching plans are individualized and all children, including infants and children with special needs, will be able to learn.
Our instructors are highly trained, experienced and caring professionals who teach with a passion and goal of promoting knowledge and safety to help prevent accidents in the water and drowning incidents. Parents are encouraged to be involved throughout the entire learning process to help their child retain skills.
Why are swimming lessons important?
Teaching children to be safe in and around water is our priority. Here are some reasons why:
- From 2002 to 2006, Broward County records show an average of nine drowning deaths a year among children under the age of 5.
- In 2005, the Florida DOH reported that 68 children between the ages of 1 to 4 drowned in Florida.
- Florida DOH records indicate that 63 percent (43) of the 68 drowning accidents reported in 2005 happened in Florida swimming pools.
While it is crucial to keep an eye on children near a body of water, it is equally important to make sure that they are comfortable in the water and respectful of its dangers. Our Nicklaus Children's Dan Marino Outpatient Center instructors apply the most effective teaching techniques to make learning a fun experience for everyone.
Swimming levels
- Infant Survival Aqua Classes (6 months to 2 years old) - This parent-and-child class helps little swimmers learn at their own pace.
- Preschool Level 1 & 2 (3 years to 5 years old) - This level allows students to gain confidence with existing skills while developing new ones.
- Level 3 (6 years to 21 years old) – This level develops stroke confidence and increases endurance to promote the ability to swim longer distances.
- Level 4 (6 years to 21 years old) -This level will teach students to improve and refine various swimming styles.
Other programs available at the Nicklaus Children's Dan Marino Outpatient Center include:
- Adaptive swimming lessons for special needs children.
- Hands-on training for Marino Swim Central Special Needs Certification.
- Individual and group lessons.
- Infant survival course.
- Nicklaus Children's Dan Marino Outpatient Center Summer Camp (Camp DMC) – recreational and instructional classes.
- Proper stroke and development instruction.
Children excel at their own rate in our classes. Our instructors guide and provide positive, corrective feedback as their students practice, experience success and receive praise for their efforts while developing skills and become safe swimmers.
Adapted Aquatics Certification
Many children with disabilities drown in the State of Florida due to the inaccessibility and unavailability of appropriate swimming programs. Teaching children to be safe in and around water is our priority for the reasons listed below. In previous years:
- Florida Department of Health (DOH) records indicate enough children die each year in water related accidents to fill approximately 4 preschool classrooms.
- Drowning is the leading cause of death and non-fatal hospitalizations for children 1 to 4 years old in Florida according to the DOH.
- Florida DOH records indicate that in 2008, 479 Florida residents drowned. Children between 1 and 4 years of age constituted 13% of those deaths and 47% of those hospitalizations.
While it is crucial to keep an eye on children near a body of water, it is equally important to make sure that they are comfortable in the water and respectful of its dangers. Many individuals with developmental disabilities are attracted to water and lack safety awareness when it comes to dangerous situations. Therefore, swimming instruction for this population is of the utmost importance. However, swimming instructors without experience with children with developmental disabilities may find it challenging to gain their attention, motivate them to follow rules and routines, and to teach basic survival skills.
Teaching basic survival skills to children with developmental delays allow them to experience aquatic activities that may offer unique experiences for the individual with developmental disabilities. Opportunity exists for motor skill acquisition, strengthening, and social/communication skills as well as fun and relaxation. Inclusion in school and community activities for these individuals has created a dramatic increase in their participation in aquatics.
Parents and caregivers of individuals with special needs look to the aquatics community for expert advice and instruction for their child and have created a demand for quality swim instruction by certified teachers with specialized knowledge.
 In order to address this problem, in April of 2006, House Bill 1319 was unanimously passed in both the Florida House of Representatives and the Senate. This Bill requires certification of swimming instructors working with people with developmental disabilities and is imperative to the safety of these individuals. The funding that the Dan Marino Foundation receives will be for the development and implementation of the instructor training program.
In order to address this problem, in April of 2006, House Bill 1319 was unanimously passed in both the Florida House of Representatives and the Senate. This Bill requires certification of swimming instructors working with people with developmental disabilities and is imperative to the safety of these individuals. The funding that the Dan Marino Foundation receives will be for the development and implementation of the instructor training program.
Our instructional manual, the online learning component, and water workshops include mandatory topics for special needs involvement in swimming and water safety. The content is mainly designed to certify instructors working with individuals with developmental disabilities. Swimming instructors completing this certification course will meet the requirements of the State of Florida for working with this population.
The Nicklaus Children's Hospital Marino Adapted Aquatics program gratefully acknowledges the generous support provided by the Dan Marino Foundation, Inc., the State of Florida, and the Broward County Board of County Commissioners.
Steps to becoming certified:
To become certified through the Nicklaus Children's Hospital Marino Adapted Aquatics Certification course, you must review the study materials and pass the Certification exam with a score of 80% or better.
Please follow these steps:
- Register online
- Submit a payment of $75 to Nicklaus Children's Hospital for the course after you register online.
- Download the course manual
- Take the exam once you receive a username and password.
- Your certificate(s) will be mailed to your billing address.
- Once you have reviewed the course materials and are prepared to take the certification exam, you will have access to the course for a duration of 4 hours. If you exceed the time allotted for the exam or do not pass, you will need to contact the Certification Manager and will be granted a chance to re-take the exam free of charge one time. If you do not pass the Certification exam on the second try, you will need to pay the course fee again.
Find a Clinician
Physician Details
Treatments, Test and Procedures
Nursing Presentations
Diagnostic Services
Birthmark Institute Home
Birthmark Institute Home
Meet the International Birthmark Institute Team
Because some birthmarks may grow in sensitive areas such as eyes, throat, nose or genitals; their removal has to be carefully planned so as not to damage any organs and not to cause disfigurement.
The The International Birthmark Institute (TIBI) is composed of a multidisciplinary team of healthcare professionals that span many pediatric disciplines. Our team of specialists can carefully asses and remove birthmarks with precision and care.
Meet the International Birthmark Institute Team
Because some birthmarks may grow in sensitive areas such as eyes, throat, nose or genitals; their removal has to be carefully planned so as not to damage any organs and not to cause disfigurement.
The The International Birthmark Institute (TIBI) is composed of a multidisciplinary team of healthcare professionals that span many pediatric disciplines. Our team of specialists can carefully asses and remove birthmarks with precision and care.
Food and Nutrition FAQ
Do I need a prescription?
Yes, your primary doctor will give you a prescription to see the dietitian. Please bring this prescription with you to your appointment with the dietitian.
Is there a cost for seeing the dietitian?
Some appointments may be covered by your insurance. Costs can be discussed with the scheduling agent when you call to make your appointment.
Do I need to bring my child to the appointment?
Yes! You must bring your child to the dietitian appointment.The dietitian will do a nutritionally focused physical exam and take your child’s height and weight.
Who else should come to the appointment?
Besides your child, any main care-taker of your child should join you. For instance, a grandparent or nanny who is part of their daily care.
How long are the appointments?
An initial appointment will usually run 45 minutes to 1 hour. Follow up appointments are generally 30 minutes.
Should I bring any paperwork?
Yes, please bring any lab work and records from outside physicians and therapists.
Where do I park?
Please use the visitors parking garage or Valet Park at the main entrance. View the Campus map and directions.
Specialty Nutrition Clinics
Ketogenic Clinic
Nicklaus Children's Hospitals Food and Nutrition Department is one of the few in Florida to offer the ketogenic diet. The ketogenic diet is a high fat diet that can control epileptic fits in some patients. Our ketogenic dietitian works closely with the medical team, patients and families to cater meals to accommodate patient’s individual preferences while working within the constructs of the prescribed diet order.
Cystic Fibrosis Clinic
A dietitian is part of the multidisciplinary Cystic Fibrosis team. Patients are evaluated on a consistent basis to monitor their growth and nutritional status. The dietitian focuses on pancreatic enzyme therapy, monitors vitamin and mineral stores and provides individualized nutrition education to every patient. The program is one of two centers in South Florida that participate in referrals from Florida’s newborn screening for cystic fibrosis.
Craniofacial Clinic
A dietitian participates as part of the multidisciplinary team of health professionals that evaluates and manages children with craniofacial anomalies through this state-designated Craniofacial Center. Each child’s unique condition is taken into consideration and nutrition interventions are designed to help each child grow to their full potential
Feeding/Swallowing Team
Patients presenting with eating difficulties may be referred for an evaluation involving specialists who address nutritional, functional/oral motor and behavioral aspects of your child’s eating habits. As a team, the dietitian, speech language pathologist and psychologist specializing in feeding behavior provide a comprehensive evaluation and develop a plan of care to address each individual’s challenges.
Dialysis
All patients on peritoneal dialysis or hemodialysis receive monthly monitoring, education, and specialized meal planning from a dietitian. The dietitian works as part of the multidisciplinary team alongside the nephrologist, social worker, and nurses to develop a plan of care to address individual needs.
Eating Disorders
The Eating Disorders Program brings together a team of specialists to evaluate the child physically and emotionally and create an individualized eating disorder treatment plan. While some children and adolescents can receive treatment on an outpatient basis, others may require hospitalization at Nicklaus Children's. First-time appointments can be made by calling 305-668-5525.
Neurogentic Clinic
Nicklaus Children's Brain Institute offers a Neurogenetics Metabolic Clinic for infants and children with genetic metabolic disorders. Our multidisciplinary team consists of a geneticist, neurologist, metabolic dietitian, and nurse practitioner. The dietitian provides extensive nutrition education during routine outpatient clinic visits and works closely with team to develop an individualized plan of care. This program participates in Florida Expanded Newborn screening incentive to diagnose these disorders early and reduce many of the neurological complications.
NeuroOncology Clinic
Nicklaus Children's Hospital has a clinic especially for children with cancers affecting the brain. The dietitian is part of a multidisciplinary team and provides comprehensive nutrition assessment and interventions for children while undergoing cancer treatment and recovery.
Lipid Clinic
The Lipid Clinic within the Heart Institute at Nicklaus Children’s Hospital is devoted to children and young adults with complex lipid disorders. Our team of pediatric cardiologists will work together with the dietitian on a comprehensive plan including close monitoring, a dietary plan physical activity recommendations and, in some cases, genetic testing or medication to control lipid disorders with the goal of preventing heart disease.
Clinical Nutrition Services by Specialty
- Adolescent Medicine (Eating disorders)
- Cardiovascular Medicine
- Child and Adolescent Psychiatry
- Diabetes and Endocrinology
- Feeding Disorders
- Gastroenterology
- General Pediatrics/Obesity
- Genetics
- Hematology and Oncology
- Immunology
- Intensive Care Unit
- Neonatology
- Nephrology
- Neurology
- Rheumatology
Resources for Patients and Families
Printables for youth
Handouts that kids will love that give basic and general nutrition information.
General Nutrition
Websites that give general nutrition information for healthy youth.
Food Allergy Information
Websites that help parents and kids learn more about living with food allergies and where to buy special foods for kids with food allergies.
Cancer Prevention
Healthy ideas for families to prevent certain cancers.
Sports Nutrition
Websites that help kids learn how to eat to fuel their bodies.
Digestion
Websites for people with gastrointestinal illnesses.
Autism
Ideas for parents whose kids are on the spectrum.
News and Articles
Conditions We Treat
Meet the Brain Institute Team
Nicklaus Children's Brain Institute is home to a unique multidisciplinary team of specialists, nurses, technologists, therapists and caregivers who provide unrivalled care, delivered with compassion and empathy for the children we treat and the families we serve.
Events
As part of our holistic approach to the care of children with neurological disorders, Nicklaus Children's Brain Institute hosts a number of educational and social initiatives throughout the year for parents, patients and physicians.
Camp Boggy Creek

Since 1996, Camp Boggy Creek has made it possible for children with serious illnesses to enjoy a camp experience in a safe, medically-sound environment completely free of charge. Located just a short drive from Orlando, Florida, the 232-acre camp serves children ages 7-16 who have been diagnosed with chronic or life-threatening conditions.
Learn more
Education
The Brain Institute plays host to the annual Pediatric Neurology Course and other pediatric neurology and neurosurgery continuing medical education (CME) programs. It also offers training for physicians from throughout the world who are pursuing fellowships in neurophysiology and care of patients with epilepsy. More than two-thirds of the fellows trained during the past 15 years came from outside the United States. The Brain Institute also hosted the world's first International Pediatric Epilepsy Surgery Symposium in 1989.
Learn more
For more information about upcoming events, please contact the Brain Institute at Brain.Institute@nicklaushealth.org
Patient Stories
Programs
Conditions We Treat
Nicklaus Children's Brain Institute provides state-of-the-art medical and surgical care for a full spectrum of pediatric neurological disorders. We have a comprehensive range of specialists, programs and clinics covering the following conditions:
News: Research & Innovation
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Brain Institute Home
Diagnostics and Treatment
Leading Edge Diagnostics
The Neuromonitoring Center offers world-renowned expertise in invasive brain recording, mapping of critical cerebral function in children, and intra-operative sensory and motor-evoked potential monitoring that contributes to the success of the most challenging epilepsy, brain tumor, cerebral palsy, spina bifida, and brachial plexus reconstruction surgeries. The laboratory offers high-resolution EEG that facilitates detection of even the most subtle abnormalities in the youngest of children. The laboratory also performs an extensive array of routine tests including video-EEG, evoked potentials, and EMG. Polysomnograms and sleep latency tests evaluate sleep and apnea disorders.
The Neuroradiology Center is one of the first in the world to apply functional MRI and tractography to define active brain networks and their connection in children, a capability offered at only a few centers in the nation. The center also has the largest experience nationwide with SPECT scans obtained early during a seizure to locate epileptogenic foci in children. The center offers a full spectrum of neuroimaging diagnostic services, including the latest CT/MRI scan sequences, angiography and ultrasonography to support the detection of even the most subtle brain abnormalities.
Next-Generation Neurosurgical Suite
Neurosurgeries are conducted in a state-of-the-art neurosurgical suite equipped with advanced neuronavigation systems and intraoperative MRI. This leading-edge suite provides enhanced efficiency and safety for neurosurgical services and offers a venue for expanded neurosurgical procedures, including functional surgery for epilepsy and movement disorders, and a platform for advanced neuroimaging research.
State-of-the-Art Neuro-Critical Care Units
A dedicated team of highly trained neuroneonatologists, pediatric neurointensivists and nursing staff take care of neonates and children who are acutely ill as a result of brain injuries such as hypoxia, trauma, tumors and severe infections, or who have undergone complex neurosurgical procedures. The units feature the most current monitoring equipment to detect seizures or changes in brain oxygenation and intracranial pressure.
Videos
Congenital Spine Diseases Program
The multidisciplinary Congenital Spine Diseases Program brings together a comprehensive team to treat children with a full spectrum of spinal disorders.
The team includes neurosurgeons, spinal surgeons, and rehabilitation specialists who collaborate to provide a comprehensive care plan to support children and families.
The surgical team's extensive experience, supported by state-of-the-art intraoperative neuromonitoring and other technologies, enchances surgical safety and preservation of spinal function.
Neurocritical Care Home
Nicklaus Children’s neurocritical care team, comprised of board-certified neurointensivists, neurosurgeons and neurologists, offers extensive expertise in the diagnosis and management of traumatic brain injuries, nervous system infections, hypoxic injuries, neuro-immune disorders, strokes, metabolic disorders, and severe uncontrolled epilepsies.
The team, which provides care for a large volume of neurocritical care patients, offers advanced diagnostic and neuro-monitoring techniques, and innovative management options, including therapeutic hypothermia, medication research trials, surgical interventions and evidence-based diets.
Neurocritical Care Home
Nicklaus Children’s neurocritical care team, comprised of board-certified neurointensivists, neurosurgeons and neurologists, offers extensive expertise in the diagnosis and management of traumatic brain injuries, nervous system infections, hypoxic injuries, neuro-immune disorders, strokes, metabolic disorders, and severe uncontrolled epilepsies.
The team, which provides care for a large volume of neurocritical care patients, offers advanced diagnostic and neuro-monitoring techniques, and innovative management options, including therapeutic hypothermia, medication research trials, surgical interventions and evidence-based diets.
Genetic Evaluation and Counseling Program
The genetic and metabolic services associated with Nicklaus Children's Hospital renowned Brain Institute feature a unique multidisciplinary clinical approach to diagnosis and treatment of complex genetic and metabolic disorders that offers unparallelled convenience and support for patients and their families.
Genetic assesment for children/infants who present any of the following:
Patients with a variety of genetic or suspected genetic conditions are seen by a board-certified genetic counselor and clinical geneticist for counseling. The team gathers detailed medical and family history information, assessing risk for offspring and family members and discussing the origin of any findings. Genetic testing options are also discussed.
Genetic counseling offered for the following referrals:
- Family history of a genetic condition
- Previous pregnancy with an abnormality/genetic condition
- Recurrent pregnancy loss
- Teratogen exposure
- Ethnicity tha may increase risk
- Advanced maternal age
- Abnormal prenatal testing
- Ultrasound anomalies
Genetic Evaluation and Counseling Program
The genetic and metabolic services associated with Nicklaus Children's Hospital renowned Brain Institute feature a unique multidisciplinary clinical approach to diagnosis and treatment of complex genetic and metabolic disorders that offers unparallelled convenience and support for patients and their families.
Genetic assesment for children/infants who present any of the following:
Patients with a variety of genetic or suspected genetic conditions are seen by a board-certified genetic counselor and clinical geneticist for counseling. The team gathers detailed medical and family history information, assessing risk for offspring and family members and discussing the origin of any findings. Genetic testing options are also discussed.
Genetic counseling offered for the following referrals:
- Family history of a genetic condition
- Previous pregnancy with an abnormality/genetic condition
- Recurrent pregnancy loss
- Teratogen exposure
- Ethnicity tha may increase risk
- Advanced maternal age
- Abnormal prenatal testing
- Ultrasound anomalies
Genetic Evaluation and Counseling Program
The genetic and metabolic services associated with Nicklaus Children's Hospital renowned Brain Institute feature a unique multidisciplinary clinical approach to diagnosis and treatment of complex genetic and metabolic disorders that offers unparallelled convenience and support for patients and their families.
Genetic assesment for children/infants who present any of the following:
Patients with a variety of genetic or suspected genetic conditions are seen by a board-certified genetic counselor and clinical geneticist for counseling. The team gathers detailed medical and family history information, assessing risk for offspring and family members and discussing the origin of any findings. Genetic testing options are also discussed.
Genetic counseling offered for the following referrals:
- Family history of a genetic condition
- Previous pregnancy with an abnormality/genetic condition
- Recurrent pregnancy loss
- Teratogen exposure
- Ethnicity tha may increase risk
- Advanced maternal age
- Abnormal prenatal testing
- Ultrasound anomalies
Neuropsychology Program
The Neuropsychology Program at the Nicklaus Children’s Brain Institute helps patients cope with issues of learning, memory, organization and emotional control resulting from brain injuries or neurological disorders.
What is a neuropsychological evaluation?
A neuropsychological evaluation is a customized assessment that provides insight into the neurocognitive (brain) mechanism and brain functioning that underlies the area of concern.
A neuropsychological evaluation can help to:
- Monitor medication-related congnitive difficulties (e.g. antiseizure, radiation, chemotherapy)
- Determine if medication dosages need to be adjusted (e.g. ADHD medication)
- Assess neurocognitive functioning after a head injury (i.e. concussion or TBI)
- Assess baseline functioning prior to new medications, brain surgery or cranial radiation
- Establish baseline functioning prior to sport participation to allow for timely intervention and treatment following sport concussions
- Identify exceptional learners with learning difficulties
- Identify areas of challenge to assist with treatment programming
A neurospychological evaluation is specifically customized to best anwer your specific concerns and typically takes between five to seven hours, depeding on assessment needs and will test the following:
- Intellectual functioning (IQ, reasoning skills, problem solving)
- Motor functioning (manual dexterity, strength and coordination)
- Auditory processing (understanding and response to heard information)
- Speech and language (understanding and effective use of oral and written language)
- Attention and executive functioning
- Learning and memory (verbal and nonverbal learning and memory)
- Academic functioning (reading, writing and math)
- Psychological, emotional and social functioning
Steps of the Neuropsychology Evaulation
- Intake: Initial session with the child’s parent(s) or legal guardian(s) to discuss any medical conditions or presenting issues.
- Testing: Your child will undergo a series of tests to determine his/her performance. Your child may have as little as two testing sessions or as many as five sessions. Each testing session takes two to three hours. Authorizations are required for each session.
- Feedback: Post testing session where the parent(s) or legal guardian(s) discuss the results and final report with the neuropsychologist.
- Follow-up: Session for the parent(s) or legal guardian(s) that is offered to discuss any updates or changes seen with your child.
Childhood Epilepsy: Your Questions Answered
Here are some questions to ask your doctor that may help you better understand epilepsy in children.
My child was diagnosed with epilepsy. What does this mean?
Childhood epilepsy is a brain disorder leading to repeated seizures over time. Seizures, also known as convulsions, are episodes in which brain activity is disturbed, causing changes in awareness, movement or behavior. Epilepsy in children is sometimes caused by certain medical conditions such as congenital brain defects or metabolic disorder present at birth, or resulting from a brain tumor or brain injury.
What are some childhood epilepsy symptoms and signs?
Symptoms of epilepsy in children vary depending on the brain area involved and the underlying cause. For example, some children with epilepsy have simple staring spells or loss of alertness, while others experience violent shaking.
Infant seizures can include sudden jerking of the head forward when sitting down. Other symptoms of epilepsy in babies can include staring into space, breathing problems or grabbing behaviors.
Symptoms of epilepsy in toddlers and older children also include:
- Suddenly falling for no reason
- Rolling of the eyes and blinking repeatedly
- Sudden nodding of the head
- Sudden stiffening of the arms or legs
Are there treatments for epilepsy in infants and children?
In most cases, childhood seizures can be well controlled by anticonvulsant drug therapy. Depending on the specific type of childhood epilepsy, some patients require several different anti-epileptic medications; surgery is an important treatment option for children who do not respond to medication, while dietary changes yield positive results in certain types of severe epilepsy.
Will epilepsy affect other aspects of my child’s life?
Many types of childhood epilepsy improve or go into remission by the late teens or early twenties, but epilepsy is life-long in some individuals. While there is a very low risk of sudden death with epilepsy, serious injuries can occur during activities like driving. Your doctor can help you determine the best childhood epilepsy treatment.
Childhood Epilepsy: Your Questions Answered
Here are some questions to ask your doctor that may help you better understand epilepsy in children.
My child was diagnosed with epilepsy. What does this mean?
Childhood epilepsy is a brain disorder leading to repeated seizures over time. Seizures, also known as convulsions, are episodes in which brain activity is disturbed, causing changes in awareness, movement or behavior. Epilepsy in children is sometimes caused by certain medical conditions such as congenital brain defects or metabolic disorder present at birth, or resulting from a brain tumor or brain injury.
What are some childhood epilepsy symptoms and signs?
Symptoms of epilepsy in children vary depending on the brain area involved and the underlying cause. For example, some children with epilepsy have simple staring spells or loss of alertness, while others experience violent shaking.
Infant seizures can include sudden jerking of the head forward when sitting down. Other symptoms of epilepsy in babies can include staring into space, breathing problems or grabbing behaviors.
Symptoms of epilepsy in toddlers and older children also include:
- Suddenly falling for no reason
- Rolling of the eyes and blinking repeatedly
- Sudden nodding of the head
- Sudden stiffening of the arms or legs
Are there treatments for epilepsy in infants and children?
In most cases, childhood seizures can be well controlled by anticonvulsant drug therapy. Depending on the specific type of childhood epilepsy, some patients require several different anti-epileptic medications; surgery is an important treatment option for children who do not respond to medication, while dietary changes yield positive results in certain types of severe epilepsy.
Will epilepsy affect other aspects of my child’s life?
Many types of childhood epilepsy improve or go into remission by the late teens or early twenties, but epilepsy is life-long in some individuals. While there is a very low risk of sudden death with epilepsy, serious injuries can occur during activities like driving. Your doctor can help you determine the best childhood epilepsy treatment.
Childhood Epilepsy: Your Questions Answered
Here are some questions to ask your doctor that may help you better understand epilepsy in children.
My child was diagnosed with epilepsy. What does this mean?
Childhood epilepsy is a brain disorder leading to repeated seizures over time. Seizures, also known as convulsions, are episodes in which brain activity is disturbed, causing changes in awareness, movement or behavior. Epilepsy in children is sometimes caused by certain medical conditions such as congenital brain defects or metabolic disorder present at birth, or resulting from a brain tumor or brain injury.
What are some childhood epilepsy symptoms and signs?
Symptoms of epilepsy in children vary depending on the brain area involved and the underlying cause. For example, some children with epilepsy have simple staring spells or loss of alertness, while others experience violent shaking.
Infant seizures can include sudden jerking of the head forward when sitting down. Other symptoms of epilepsy in babies can include staring into space, breathing problems or grabbing behaviors.
Symptoms of epilepsy in toddlers and older children also include:
- Suddenly falling for no reason
- Rolling of the eyes and blinking repeatedly
- Sudden nodding of the head
- Sudden stiffening of the arms or legs
Are there treatments for epilepsy in infants and children?
In most cases, childhood seizures can be well controlled by anticonvulsant drug therapy. Depending on the specific type of childhood epilepsy, some patients require several different anti-epileptic medications; surgery is an important treatment option for children who do not respond to medication, while dietary changes yield positive results in certain types of severe epilepsy.
Will epilepsy affect other aspects of my child’s life?
Many types of childhood epilepsy improve or go into remission by the late teens or early twenties, but epilepsy is life-long in some individuals. While there is a very low risk of sudden death with epilepsy, serious injuries can occur during activities like driving. Your doctor can help you determine the best childhood epilepsy treatment.
Childhood Epilepsy: Your Questions Answered
Here are some questions to ask your doctor that may help you better understand epilepsy in children.
My child was diagnosed with epilepsy. What does this mean?
Childhood epilepsy is a brain disorder leading to repeated seizures over time. Seizures, also known as convulsions, are episodes in which brain activity is disturbed, causing changes in awareness, movement or behavior. Epilepsy in children is sometimes caused by certain medical conditions such as congenital brain defects or metabolic disorder present at birth, or resulting from a brain tumor or brain injury.
What are some childhood epilepsy symptoms and signs?
Symptoms of epilepsy in children vary depending on the brain area involved and the underlying cause. For example, some children with epilepsy have simple staring spells or loss of alertness, while others experience violent shaking.
Infant seizures can include sudden jerking of the head forward when sitting down. Other symptoms of epilepsy in babies can include staring into space, breathing problems or grabbing behaviors.
Symptoms of epilepsy in toddlers and older children also include:
- Suddenly falling for no reason
- Rolling of the eyes and blinking repeatedly
- Sudden nodding of the head
- Sudden stiffening of the arms or legs
Are there treatments for epilepsy in infants and children?
In most cases, childhood seizures can be well controlled by anticonvulsant drug therapy. Depending on the specific type of childhood epilepsy, some patients require several different anti-epileptic medications; surgery is an important treatment option for children who do not respond to medication, while dietary changes yield positive results in certain types of severe epilepsy.
Will epilepsy affect other aspects of my child’s life?
Many types of childhood epilepsy improve or go into remission by the late teens or early twenties, but epilepsy is life-long in some individuals. While there is a very low risk of sudden death with epilepsy, serious injuries can occur during activities like driving. Your doctor can help you determine the best childhood epilepsy treatment.
Referral Guidelines for Physicians
Definition of Concussion
Any direct or indirect trauma to the head and/or neck that results in any of the following symptoms:
- Loss of consciousness
- Headache
- Nausea
- Vomiting
- Balance problems
- Dizziness
- Lightheadedness
- Fatigue
- Drowsiness
- Sensitivity to light or noise
- Feeling more emotional
- Numbness or tingling
- Feeling like "in a fog"
- Difficulty concentrating
- Difficulty remembering/amnesia
- Visual problems
For children who exhibit one symptom for a brief period of time, this may be a liberal definition. However, there are some children who recover initially but with subsequent exertion have delayed onset ot symptoms.
Who Needs to Be Referred to the Concussion/Brain Injury Clinic?
- All children who meet the above criteria for concussion, even if they appear “normal” at the time of discharge. There can be an asymptomatic interval between concussion and symptoms, usually brought on by cognitive or physical exertion, e.g., going to school.
- All children with GCS < 15
- All children who meet criteria for a brain CT for CHI whether positive or negative for TBI. The rationale is that if they appear acute enough to need a brain CT or meet the PECARN criteria for CT, they need follow up.
- All children with an abnormal brain CT, including skull fracture.
- All sports related injuries that require return to play clearance in compliance with Florida law requiring all athletes to obtain written clearance from a LHCP before returning to play.
- All kids with a history of prior TBI/concussion.
- Mild TBI or concussion patients discharged from ED/UCC should initially be sent to the Concussion/Brain Injury Clinic. Neurosurgical referrals will then be made as needed.
Rationale for Early Concussion Evaluation and Management:
- Education and reassurance of family and child.
- Early intervention to decrease duration and severity of symptoms and reduce returns to ED.
- Implement return-to-school protocol with individualized accommodations as needed. Concussion clinic personnel communicate with the TBI specialist for Miami-Dade public schools and school personnel to ensure implementation of classroom accommodations.
- Implement safe return-to-play protocol
- Appropriate referrals for vestibular, exertional, oculomotor and general physical therapy, as well as neuropsychological and psychological assessment and treatment.
- Repeated follow up clinic visits to maximize recovery and achieve best outcome.
- Detailed report sent to all PCPs and referring physicians after evaluation.
Referral Guidelines for Physicians
Definition of Concussion
Any direct or indirect trauma to the head and/or neck that results in any of the following symptoms:
- Loss of consciousness
- Headache
- Nausea
- Vomiting
- Balance problems
- Dizziness
- Lightheadedness
- Fatigue
- Drowsiness
- Sensitivity to light or noise
- Feeling more emotional
- Numbness or tingling
- Feeling like "in a fog"
- Difficulty concentrating
- Difficulty remembering/amnesia
- Visual problems
For children who exhibit one symptom for a brief period of time, this may be a liberal definition. However, there are some children who recover initially but with subsequent exertion have delayed onset ot symptoms.
Who Needs to Be Referred to the Concussion/Brain Injury Clinic?
- All children who meet the above criteria for concussion, even if they appear “normal” at the time of discharge. There can be an asymptomatic interval between concussion and symptoms, usually brought on by cognitive or physical exertion, e.g., going to school.
- All children with GCS < 15
- All children who meet criteria for a brain CT for CHI whether positive or negative for TBI. The rationale is that if they appear acute enough to need a brain CT or meet the PECARN criteria for CT, they need follow up.
- All children with an abnormal brain CT, including skull fracture.
- All sports related injuries that require return to play clearance in compliance with Florida law requiring all athletes to obtain written clearance from a LHCP before returning to play.
- All kids with a history of prior TBI/concussion.
- Mild TBI or concussion patients discharged from ED/UCC should initially be sent to the Concussion/Brain Injury Clinic. Neurosurgical referrals will then be made as needed.
Rationale for Early Concussion Evaluation and Management:
- Education and reassurance of family and child.
- Early intervention to decrease duration and severity of symptoms and reduce returns to ED.
- Implement return-to-school protocol with individualized accommodations as needed. Concussion clinic personnel communicate with the TBI specialist for Miami-Dade public schools and school personnel to ensure implementation of classroom accommodations.
- Implement safe return-to-play protocol
- Appropriate referrals for vestibular, exertional, oculomotor and general physical therapy, as well as neuropsychological and psychological assessment and treatment.
- Repeated follow up clinic visits to maximize recovery and achieve best outcome.
- Detailed report sent to all PCPs and referring physicians after evaluation.
Patient Stories
Patient Stories
Patient Stories
Patient Stories
Conditions we Treat
The brachial plexus is a network of nerves within the neck that supply the arm with motor input and sensory feedback. Injuries to the brachial plexus can occur during the birthing process or as a result of trauma, including falls, sports injuries, penetrating injuries (stab wounds/gunshot wounds) and motor vehicle collisions.
In addition to our focus on the brachial plexus, the Program also provides care for children with injuries or diseases (including tumors) of other peripheral nerves throughout the body.
Read more about the different kinds of injuries and syndromes treated by the program below:
Conditions we Treat
The brachial plexus is a network of nerves within the neck that supply the arm with motor input and sensory feedback. Injuries to the brachial plexus can occur during the birthing process or as a result of trauma, including falls, sports injuries, penetrating injuries (stab wounds/gunshot wounds) and motor vehicle collisions.
In addition to our focus on the brachial plexus, the Program also provides care for children with injuries or diseases (including tumors) of other peripheral nerves throughout the body.
Read more about the different kinds of injuries and syndromes treated by the program below:
Conditions we Treat
The brachial plexus is a network of nerves within the neck that supply the arm with motor input and sensory feedback. Injuries to the brachial plexus can occur during the birthing process or as a result of trauma, including falls, sports injuries, penetrating injuries (stab wounds/gunshot wounds) and motor vehicle collisions.
In addition to our focus on the brachial plexus, the Program also provides care for children with injuries or diseases (including tumors) of other peripheral nerves throughout the body.
Read more about the different kinds of injuries and syndromes treated by the program below:
Conditions we Treat
The brachial plexus is a network of nerves within the neck that supply the arm with motor input and sensory feedback. Injuries to the brachial plexus can occur during the birthing process or as a result of trauma, including falls, sports injuries, penetrating injuries (stab wounds/gunshot wounds) and motor vehicle collisions.
In addition to our focus on the brachial plexus, the Program also provides care for children with injuries or diseases (including tumors) of other peripheral nerves throughout the body.
Read more about the different kinds of injuries and syndromes treated by the program below:
Conditions we Treat
The brachial plexus is a network of nerves within the neck that supply the arm with motor input and sensory feedback. Injuries to the brachial plexus can occur during the birthing process or as a result of trauma, including falls, sports injuries, penetrating injuries (stab wounds/gunshot wounds) and motor vehicle collisions.
In addition to our focus on the brachial plexus, the Program also provides care for children with injuries or diseases (including tumors) of other peripheral nerves throughout the body.
Read more about the different kinds of injuries and syndromes treated by the program below:
Videos
Videos
Videos
Videos
Videos
Brachial Plexus Home
Brachial Plexus Home
Brachial Plexus Home
Brachial Plexus Home
Brachial Plexus Home
Conditions we Treat
Conditions we Treat
Conditions we Treat
Sleep Disorders Center Home
Sleep Disorders Center Home
Sleep Disorders Center Home
Meet the NeuroCardiac Team
Meet the NeuroCardiac Team
Meet the NeuroCardiac Team
Epilepsy Center Home
Epilepsy Center Home
Epilepsy Center Home
Epilepsy Center Home
NeuroCardiac Home
NeuroCardiac Home
NeuroCardiac Home
Conditions we Treat
Program candidates include any child or teen who:
- Has headaches that occur on a consistent basis
- Has headaches that result in missed school days or other activities
- Has headaches that cause concern for the patient, parents, or primary care physician in any way
Conditions we Treat
Program candidates include any child or teen who:
- Has headaches that occur on a consistent basis
- Has headaches that result in missed school days or other activities
- Has headaches that cause concern for the patient, parents, or primary care physician in any way
Conditions we Treat
Program candidates include any child or teen who:
- Has headaches that occur on a consistent basis
- Has headaches that result in missed school days or other activities
- Has headaches that cause concern for the patient, parents, or primary care physician in any way
Lucas Pineda Donation Page
crm-footer-2
heidi-gamboa-gastroenterology
Medical Education Dues
Student/Observer - Application Fee
Please fill out the registration to proceed to payment.
Payment
Application Fee - $500
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
Student/Observer - Background Screening Fee
Please fill out the registration to proceed to payment.
Payment
Background Screening Fee - $150
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
News & Research
News & Research
News & Research
News & Research
News & Research
Pediatric Gastroenterology, Hepatology and Nutrition Fellowship
Heart Institute
Sports Medicine Program
EKG News
EKG Test Home
Luca Pineda
PhysicianChat
Specialty Care Centers
Specialty Care Center Services
As part of Nicklaus Children's commitment to enhancing service convenience for South Florida families, our network of Care Centers offer consultations by appointment with board certified specialists for babies, children, teens and young adults under 21 years old. Specialties vary per location, please view each center's page for more details.
Cleft Lip & Palate Course
Please fill out the form to register.
Registration Payment
Click on the button to pay with credit card.
The link will open Authorize.net to complete the transaction.
Hospitalist Medicine Home
CME Mission Statement
Nicklaus Children's Hospital's mission is to “inspire hope and promote lifelong health by providing the best care to every child”. As a teaching institution Nicklaus Children's Hospital is committed to supporting the professional and educational needs of its health care providers, and the lifelong learning of the interprofessional team with the aim to provide the best possible care to every child. Continuing medical education (CME) is one of the major ways in which Nicklaus Children's Hospital supports its overall mission.
CME Purpose
Nicklaus Children's Hospital is committed to advancing the knowledge, enhancing the competence and performance in practice of clinicians, with the ultimate goal of improving patient outcomes through the design and delivery of high-quality, evidence-based continuing medical education (CME) programs that focus on patient care, medical knowledge, practice-based learning and improvement (i.e. Quality Improvement, patient safety, research), interpersonal and communication skills, professionalism, and systems-based practice (i.e. Interprofessional education). The CME programs focus on common practice guidelines, advances in medicine, new medical technology, biomedical research, healthcare quality, patient-centered care, and changes in the health care environment.
Content Areas
The CME Committee utilizes the ACGME/ABMS/ IOM core competencies as a platform for content areas. The contents are developed based on annual and continuous needs assessments for the overall institutional CME program and individual activities. The needs assessment process identifies “gaps” in attendees’ knowledge, competence and/or performance. Other sources of content include hospital-specific or national patient care initiatives, peer-reviewed published literature, re-licensure requirements, maintenance of certification or accreditation, hospital committee-identified gaps or needs for improvement, and various practice and referral patterns. CME activities are planned in the context of desirable physician attributes and core competencies to promote dissemination of high quality practice patterns and serve the best interest of the public. Topics are assigned to the activity that is best suited for its target audience and delivery format. The content of Nicklaus Children's Hospital CME activities includes, but not limited to, a) all aspects of patient care (diagnosis, management, and prevention) of children in the areas of primary and subspecialty pediatric problems, b) quality improvement, c) medical ethics d) faculty development e) clinical and translational research, f) business of medicine and risk management g) hot and emerging topics.
Target Audience
Nicklaus Children's Hospital's CME activities are provided to:
- Pediatricians, House Staff physicians, medical students, pediatric subspecialists in medicine & surgery
- Pediatric researchers
- National and international clinicians
- Allied health and members of multidisciplinary/interprofessional teams
- Parents/family representatives
Types of Activities
Nicklaus Children's Hospital offers a range of CME activities including the following:
- Regularly scheduled series (RSS), e.g. Grand Rounds, Faculty Development, Tumor Board, Radiology Conference, Community-Based Educational programs, and Trauma and Cardiology Conferences
- Live Courses: e.g. General Pediatric & Pediatric Critical Care Board Review Courses, Pediatric Post Graduate Course (PPGC)
- Virtual/e-learning/online education – This includes live transmission of courses and/or archived/video-on-demand enduring materials
Expected Results
The expected result of Nicklaus Children's Hospital's CME is to:
- Improve physician competence measured by outcome assessment (including knowledge, skills and attitudes)
- Improvement in performance-in-practice through assessment of intent of behavior change and implementation of practice change
- Improved patient outcomes through self-reported improvement or quality improvement data or EMR data when feasible. It is also hoped that as clinicians improve their competence and performance, this will translate into improvement of patient outcomes meeting ultimately the hospital’s and health system’s mission to “inspire hope and promote lifelong health by providing the best care to every child”.
Last Review – July 2018
Relicensure Courses
Earn CME credit that counts towards your license renewal from the comfort of your own home or office! Nicklaus Children’s Hospital is proud to offer Florida required courses on its on-demand CME platform, iLearnPeds.com. Upon registration and completion of one of the courses shown below, you will receive a CME certificate with the amount of AMA PRA Category 1 CreditsTM shown below.
If you are a Nicklaus active medical staff member, please contact us at 305-669-5873 for information on receiving a discount on our relicensure courses.
- NEW! Prescribing Controlled Substances
(Provided by Baptist Health South Florida)
Issued on: February 1, 2019
Expires on: January 31, 2020
2 AMA PRA Category 1 Credits™
- Domestic Violence
Issued on: December 8, 2017
Expires on: December 7, 2019
2 AMA PRA Category 1 Credits™
- HIV/AIDS Update
Issued on: January 19, 2018
Expires on: January 18, 2020
1 AMA PRA Category 1 Credits™
Accreditation Statement
Nicklaus Children’s Hospital is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Disclosure and Conflict of Interest Resolution
All conflicts of interest of any individual(s) in a position to control the content of a CME activity will be identified and resolved prior to the educational activity being provided. Disclosure about provider and faculty relationships, or the lack thereof, will be provided to learners.
Links and Resources
CME Requirements for Relicensure (FMA)
Frequently Asked Questions
Meeting planners or program chairs wishing to request CME sponsorship from the Department of Medical Education at Nicklaus Children's Hospital for their planned educational activities are required to follow the steps and timeline below in starting the application process. Click on the links below to be directed to a step-by-step planning process for your CME activity.
5 months before activity
Activity Chair, CME Director, and Committee
Activity Chair awaits notification of approval of Activity Request. All COIs should be resolved prior to proceeding with the planning process.
Activity Chair and CME Staff
- Schedule a meeting with CME Staff to discuss steps and CME Checklist deadlines.
- CME Department provides an orientation to the Nicklaus CME website, forms, and roles.
4-5 months before activity
Activity Chair
Once all COIs of activity director and planner are resolved, complete and submit a CME Application Form along with the following documents:
- Draft agenda
- List of confirmed speakers
- Proposed Budget (Contact the CME Department for the template.)
- Marketing Materials (when ready) for review
- AV Request Form
- Proposed Evaluation Forms
If activity is a Regularly Scheduled Series, the activity chair must complete one of the following:
- CME Application Form for the entire series, if the sessions have the same theme
- CME Application Form for the entire series and an RSS addendum for each session, if the sessions vary in theme
CME Staff
The CME Department designs the activity's registration site or dedicated landing page based on feedback from the Activity Chair and Planners.
4 months before activity
Activity Chair
If soliciting educational grants or exhibitor support, submit one of the following:
- Educational grants - A signed Written Agreement for Commercial Support for each commercial entity
- Exhibitors - A signed exhibitor agreement
Please note that there are differences in policy between exhibitors and educational grants. All grants requests and exhibitor agreements MUST be reviewed by CME staff prior to execution in order to ensure compliance.
CME Staff
The CME Department sends letters to faculty to collect faculty disclosures, CVs, and other documents.
2 months before activity
Activity Chair or Planner(s)
OPTIONAL - Submit a revised preliminary budget.
During the activity
Activity Planner(s)
- Maintain accurate sign-in sheets.
- Collect evaluation sheets from attendees:
- Faculty Evaluation
- Activity Evaluation
- Pre and Post Surveys
2 weeks after activity
Activity Planner(s)
Submit all sign-in sheets, evaluations, and forms collected during the event to the CME Department.
1 month after activity
CME Staff
- The CME Department grants CME credits based on attendance records, sign-in sheets, and/or evaluation forms.
- Emails are sent to attendees with instructions on claiming their CME certificates.
2 months after activity
Activity Chair or Planner(s)
- Submit copies of final syllabus and/or handouts.
- Submit a final budget report. (Contact the CME Department for the template.)
CME Staff
The CME staff distributes the Evaluation Summary Reports to CME Director (and optionally, to the Activity Chair).
- Speaker Valuation by Learners
- Event Evaluation by Learners
- Pre/Post Survey Gap Analysis Report
3 months after activity
Activity Chair
If applicable, consider a 3-month Post-Activity Survey to assess practice change.
CME Committee
| Committee Member |
Role |
Liaison to other committees |
| Rani Gereige, MD, MPH - Committee Chair |
Director of Medical Education |
- GMEC, Chair
- Library Committee, Chair
- Mortality & Morbidity Review Committee, Member
- IT PAG for EMR, Member
|
| Jefry Biehler, MD, MPH |
- Chair of Pediatrics - FIU
- Med Students Clerkship Director
|
- GMEC, Member
- IT PAG for EMR, Chair
- Mortality & Morbidity Review Committee, Member
- Utilization Review and Quality, Physician Reviewer
|
| Beatriz Cunill, MD |
Pediatric Residency Program Director |
- GMEC, Member
- ICU Committee, Member
- IT PAG for EMR, Member
- Quality Pillar/ Blue Chip, Member
|
| Jose Rosa-Olivares, MD |
General Pediatrics - Attending |
IT PAG for EMR, Member |
| Elizabeth Menocal |
Senior Director, Medical Staff Resources |
- Blue Chip on IV Infiltration, Member
- Credentials Committee, Member
- Medical Executive Committee, Member
- Bylaws Committee, Member
|
| Shakeva Swain, RN |
Coordinator, Trauma RSS |
- Trauma Physician Peer Review, Planner
- Trauma Quality Management Committee, Member
- Hospital Safety and Compliance Committee, Member
|
| Gabriela Martinez |
CME Specialist
(e-Learning, Marketing, Social Media, and Website) |
|
CME COMMITTEE MEMBERS ROLES AND RESPONSIBILITIES (Click to view)
crm-header-2
julio-daniel-egusquiza-radiology-house-officer
gilbert-smith-psychiatry
subaraman-ramchandran-spine-surgery
courtney-wein-cardiology
Enrich
Craniofacial Center
Conditions we Treat
We provide pediatric therapy for the following conditions:
- Amputee
- Auditory processing disorders
- Fine and gross motor coordination deficits
- Fluency disorder
- Neurological-based disorders
- Orthopedic rehabilitation
- Prematurity
As well as:
Uno Card Campaign
Spine Surgery
Spine Surgery
Foot Deformities
Nicklaus Children's Research Institute
Brain Institute Team
Presentations
Event Photos
Main Topics
- Gutsy Kids: Exploring the Microbiome and its Impact on Pediatric Health - Dr. Luis Caicedo
- Nourishing the Preemie Baby: A Guide to Optimal Growth and Development - Velma Mercado, RD/LDN and Arantza Barroso, RD/LDN
- The Ins and Outs of Nutrition Therapy for Eating Disorders - Melia Menendez-Aponte, RDN/LDN
- From Hospital to Home: Ensuring Smooth Coordination of Care for Home Enteral and Parenteral Patients - Erin Corrigan, MS, RDN, CNSC
- Growing the Future: From the Hospital to the Community - Nicole Dulzaides, MS, RDN, LD/N
Round Tables
- Being a Cystic Fibrosis RD: Yesterday, Today and the Promising Future - Cristina Visona, MS, CSP, RD/LDN
- Uncovering the Potential of the REAL Ketogenic Diet - Laura Garcia, MS, RD/LDN
- Nutrition Therapies for Inflammatory Bowel Disease - Mirta Rios, CSP, RD/LDN
- Plant-Based Nutrition for Pediatric Renal Patients - Megan Wakai, MPH, RD/LDN
- A Review of Pediatric Commercial Formulas and Home-made Blenderized - Julia Leone, MS, RD/LDN
- Advancements in Individualized Nutrition Strategies for Critically Ill Pediatric Patients - Pierina Picasso, MS, RD/LDN, CNSC, CSPCC
- Updates in Nutrition and Type I DM - Maria Paula Criado, RD/LDN
- Counseling the Child and Adolescent Athlete - Maria Parra, MS, RD/LDN
- Improving Outcomes in Treatment of Childhood/Adolescence Overweight/Obesity - Tania Koerber, CSP, RD/LDN
Videos
Nicklaus Children's Pediatric Specialists
Board of Directors
Therapeutical Treatments and Services
Man Vs Impossible
Treatments and Procedures
Treatments and Procedures
Treatments and Procedures
Treatments and Procedures
Treatments and Procedures
Treatments and Procedures
For Researchers
Our Biobank Samples
The Nicklaus Children's Biobank has the ability to collect blood samples (store extracted DNA) and data from a participant over time and to include samples from both the proband and family members is highly significant in terms of the ability of the Biobank to support studies focused on personalized and translational medicine. The Biobank will also collect, process, and store remnant and archived clinical material (tissue and fluids – FFPE & Archival tissue services), and specimens collected specifically for research purposes (tissue and fluids). Samples may be used immediately, further processed (into DNA, cell lines, etc.), and/or stored for future use. It is anticipated that the exact procedures for aliquoting, processing, and storage will vary over time so that the Biobank can optimize the mix of samples and matrices to match evolving research needs.
Sample integrity is essential to the success of every research project. Various Pre and Post-analytical variables can be introduced at numerous points in a sample, beginning at the time it is collected, through transport, receiving, laboratory processing, during storage and subsequent retrieval for analysis. For the Nicklaus Children's Biobank, providing high quality samples is our goal.
Our Biobank Services
Nicklaus Children's Biobank operates to national and international standards. All biospecimens are validated against original pathological diagnosis to confirm accuracy and assure high quality standards. Nicklaus Children's Biobank supports research by ensuring investigators have access to high quality samples annotated with clinical data.
Nicklaus Children's Biobank provides services in:
- baking of samples,
- procurement, processing, archiving, and distribution of fresh and formalin-fixed tissues and body fluids,
- specimen characterization, quality control, and linkage with pathological and clinical annotation,
- auxiliary services including histology, immunohistochemistry, whole blood DNA Extraction, and computer-assisted imaging/image analysis.
Our Biobank is designed to support the biospecimen handling requirements of any local or multi-institutional research study, biobanking, or clinical trial with full integration into our Clinical Trial Management System.
Biorepository Services
- Access to Banked samples
- Modular collection kits for biospecimen collection that allow for standardized collection and specimen annotation from on and off-site locations
- Body fluid processing and aliquoting
- Surgical specimen procurement by specialized staff stationed in the pathology suite
- Tissue fixation and embedding
- Specimen archiving and inventory
- Distribution of specimen and associated data for research projects
- Provide remnant archival material from surgical pathology specimens for research projects
- Imaging and image analysis (Aperio XT and Syncroscopy tissue imaging system)
Please contact us to discuss your project; our services can be tailored to meet the needs for individual collections and research projects at biobank@nicklaushealth.org. Pricing available upon request.
How to Apply
Step 1:
- Fill out the RedCap form
- With your project information and detailed sample request. You will also be required to submit the Curriculum vitae of Principal Investigator (no longer than 2 pages) and IRB approval and amendment letters (or equivalent).
- We also recommend you read the Nicklaus Children’s Biobank Conditions of Use.
Step 2:
- We will review your application and provide a feasibility assessment in 5-7 business days.
Step 3:
- You will receive letter of approval, plus work order. Upon approval, your project will commence! Any subsequent de-identified clinical data will be securely transferred to you and samples will be shipped expeditiously.
Please contact us to discuss your project. Our services can be tailored to meet the needs for individual collections and research projects at
biobank@nicklaushealth.org – Pricing available upon request.Frequently Asked Questions
What is a biobank?
A biobank is similar to a library. It holds samples, known as “biospecimens,” that are provided voluntarily by hundreds, sometimes thousands, of individuals. These samples, which can include blood, saliva, tissue, stool or urine, are important to scientists, who study them to learn about elements that affect children’s health.
Why join the Nicklaus Children’s Hospital Biobank?
With minimal effort, you and your child will contribute to scientific knowledge that can lead to improvements in healthcare management and treatment for children and lead to brighter tomorrows for young people everywhere. The study of biospecimens can help scientists learn:
- How the body works
- How disease develops and affects the body
- How to treat diseases and conditions
Will biobank participation directly benefit my child?
Medical research is time consuming. It is not likely that knowledge gained through the biobank will directly benefit you or your child’s medical care plan. However, it may benefit future patients.
Who can join the Nicklaus biobank?
Any child and his or her family members can participate in the Nicklaus Children’s Biobank. Participation is always voluntary and participants can withdraw at any time.
How can we get started?
If you are interested in contributing, you will be asked to review and sign an informed consent form allowing the Nicklaus Children’s Biobank to collect an extra sample during the next clinical visit, and/or store samples that are no longer needed for clinical care, along with information in your medical record.
Is there a fee for participating?
No, there are no additional fees associated with biobank participation.
What will happen to the sample provided? What about privacy?
Nicklaus Children’s is collaborating with Sanford Health in Sioux Falls, South Dakota for long-term sample storage. Before shipment, samples are de- identified. This means that all personal information is removed from the sample and stored within Nicklaus Children’s secure data system. Samples are assigned a unique identification number.
Researchers will only see this unique identification number and not the identity of the individuals who provided the samples. Nicklaus Children’s will always retain ownership of all samples and ensure safekeeping for all participant personal information.
How will my sample be used?
Samples will help researchers and doctors understand disease and may help identify treatments or cures. Examples of ways in which your sample may be used include population studies of genetics, cancer research, and assessments of treatments and other medical advancements. Any researcher or doctor who seeks to use samples from the Nicklaus Children’s Biobank needs to submit a proposal to the hospital’s scientific committee and obtain approval from the institutional review board, an administrative body that protects the rights and welfare of human research subjects.
What if we want to withdraw from the biobank?
If you or your child decide at any point that you no longer want to participate in the biobank, Nicklaus Children’s will remove your samples. However, when data has already been analyzed and included in an academic paper, it is not possible to omit your sample from the data.
Is it possible to know about the studies conducted using my sample?
We will publish information about our studies on our website.
Does my family have any rights over the study results?
Research results involve intellectual property rights relating to the study outcome. Those rights do not belong to the donors or their families.
Ethics
The Nicklaus Children's Biobank is committed to ensuring that the collection of research biospecimens does not interfere with patient care and that the privacy and confidentiality of all volunteer donors are maintained.
Informed consent for sample collection and research use is obtained from all patients. NCH Biobank complies with all existing USA federal, state, territory and institutional requirements pertaining to the participation of patients in research, as well as the collection and use of research biospecimens and accompanying clinical data.
Collection of research biospecimens and associated clinical data has been approved by the research ethics committees at participating healthcare institutions. All research applications for biospecimens and clinical data must be accompanied by research ethics approvals of the research study and are subject to further review and approval by an internal Advisory Review Committee.
All biospecimens and associated clinical data are de-identified so that a patient’s identity is accessible only to NCH Biobank authorized staff. Identifying information is not disclosed to any recipient medical researchers.
Biobank Home
Pediatric Surgery Home
Programs and Clinics
Athletic Training Services
Genetics and Metabolic Disorders Home
Tests and Genetic Screenings
Physicians
Craniofacial Center Services
IGIVE Employee Campaign
Conditions we Treat
Conditions we Treat
Conditions we Treat
Conditions we Treat
Conditions we Treat
luxme-hariharan-ophthalmology
shelly-wang-neurosurgery
carla-perez-gastroenterology
verena-schreiber-orthopedic-surgery
Diabetes Center Home
Diabetes Center Home
Managing Diabetes in Children (Video series)
Managing Diabetes in Children (Video series)
Managing Diabetes in Children (Video series)
News
Treatments and Diagnostics
Patient Stories
Patient Stories
Heart Institute
Cancer & Blood Disorders Institute
Brain Institute
Fetal Care Services
Orthopedic Surgery Program
Sports Health/Medicine Program
Sports Health Center (in Pinecrest)
Giving Tuesday
Adolescent Medicine Home
Psychiatry Home
Evaluations and Treatments
Treatments and Therapies
Psychology Home
News
News
Spine Disorders Home
Spine Disorders Home
Treatments and Procedures
Rehab Home
Symptoms
Symptoms
Treatments and Procedures
Procedures
PCP-Seminar-Series
Thank You
Nephrology (Home)
Treatments and Procedures
Treatments and Procedures
Birdies for Children
International Patient Services
International Patient Services
Global Health Home
Doral Orientation
International Patient Services
Expert Care Coordination by a Comprehensive Team of Pediatric Specialists
Our multilingual concierge staff are specially trained to serve the unique needs of patients and families traveling from around the world in search of answers and groundbreaking treatments for their child. Our expert care coordination begins with the first contact and continues throughout your child’s stay, follow-up care and the transition back home, including coordination and follow-up with your local physician team.
Travel Arrangements
Traveling to receive medical treatment for your child can be complicated, often perplexing, and very expensive. We are your liaison for all medically-related financial arrangements, working with international insurance providers and foreign government agencies. Non-insured patients will receive an estimate of expenses and deposit requirements.
Critical Care Transport
For the critically ill or injured child, Nicklaus Children's Global Health can arrange LifeFlight® Critical Care Transport via ground (ambulance), helicopter, and fixed wing aircraft. Our team of medical transport professionals, including a physician, will coordinate the transport of critically ill or injured children from anywhere in the hemisphere to Nicklaus Children's Hospital. The LifeFlight® Critical Care Transport Helicopter Team specifically serves South Florida, the Caribbean and Central and South America.*
*Nicklaus Children's Hospital is not a direct air carrier. Aircraft, both helicopter and fixed wing, are operated pursuant to contract with Nicklaus Children's Hospital, by companies which are FAA certificated.
The best accommodations and services
From five-star hotels to long-term condominium rentals, we can help you find the best accommodations to fit your personal tastes, needs, and situation. Special corporate rates have been negotiated for our international patients and their families.
Nicklaus Children's Hospital is located in a beautiful and tranquil family-friendly area just outside Coral Gables. This is a community long known for its semi-tropical beauty and easy accessibility by car, Tri-Rail or bus, to Miami International Airport, the downtown area, cultural center and numerous attractions including Parrot Jungle, Seaquarium and the Museum of Science. Miami is called the “magic city” because it has it all… and more. Here, treatment and rehabilitation can take place in an environment made for children and their families.
Language Services
As the gateway to the Americas, Miami has an international flavor that will make anyone feel right at home. Spanish, English, Creole, and Portuguese, as well as Arabic, French, German, Mandarin and Russian are among the many languages spoken by our diverse, multilingual staff. Additionally, Nicklaus Children's Hospital has access to a 24-hour Language Line, a service that allows for translation via telephone for whichever language is needed, available seven days a week. This service is free to our patients and ensures that language is not an obstacle to receiving world-class care.
Staying in touch with home
We recognize that you have responsibilities at home and that it is important for you to stay in touch with your family, friends, and office when you travel. Whether you need to send or receive facsimiles or e-mail, require the services of a courier, or any other personalized assistance, call us and we will promptly make arrangements to take care of those needs.
At Nicklaus Children's Hospital we will do anything and everything possible to make sure you receive the highest quality healthcare in a truly friendly, accommodating environment with a doctor and staff who will communicate with you and is sensitive to your culture.
Religious Services & Cultural Needs
At Nicklaus Children's Hospital, we will do anything and everything possible to make sure you receive the highest quality healthcare in a truly friendly, accommodating environment with a doctor and staff who will communicate with you and is sensitive to your culture.
An interfaith chaplain is available for the spiritual and emotional needs of patients and families and visits those who have requested the chaplain upon admission or during their hospitalization. The chaplain leads daily healing prayer services for families and staff in the hospital chapel, and administers religious rites, sacraments and celebrations in accordance with the faith and traditions of patients and families. The chapel, located on the main hospital campus, is available for people of all faiths to use for personal prayer and meditation, and is also accessible for observance of diverse interfaith religious holidays throughout the year.
International Patient Registration Form
Preparing for Your Visit
Your first point of contact should be the Global Health team. We expedite all necessary appointments and admissions, including coordinating coverage and authorizations with your international insurance provider. We will also help you better understand your child’s plan of care, provide information on our medical team and assist with the logistics of your trip (visas, accommodations, etc.). We are always available to answer any questions or discuss any issues you may have.
Be sure to bring all medical documents and imaging from your primary doctor, as well as travel and financial documents. If you are unsure about the paperwork required, please contact the Global Health team.
Resources to Prepare for your Visit
Maps and Directions

Directions to the Hospital

Directions to Global Health Center
Local Miami Guides and Information
Local Weather
Patient Stories
2020 NCYA Kickoff
Treatments
The treatment approach to peripheral nerve problems depends upon the nature of the problem. Many injuries, particularly “stretch injuries” will recover without requiring surgery. Some injuries, especially severe stretch injuries or lacerations, will require surgery to repair or reconstruct the affected nerves.
With respect to brachial plexus birth injuries, the majority of babies affected by this condition will make a full recovery with therapy alone, while others may require extensive therapy and possibly surgical intervention. Treatment initially includes:
- Specialized occupational therapy to maintain motion and prevent joint deformity in the affected arm.
- Specialized splints may be required to protect the joints from developing deformities.
In some cases, botulinum toxin (Botox) is used to temporarily weaken “functioning” muscles that are contributing to joint deformity. After the Botox is given, intensive therapy is used to help strengthen the “weakened” muscles and place the shoulder in a better position.
If the injury is severe, surgery may be required to release affected nerves from surrounding scar tissue, repair/reconstruct damaged nerves, or transfer “redundant” nerves to stimulate muscle function.
Additional procedures that may be recommended as children grow, include release of tight muscles or joints, tendon transfers, or joint fusions.
Read more about the different approaches to treatment below:
Treatments
The treatment approach to peripheral nerve problems depends upon the nature of the problem. Many injuries, particularly “stretch injuries” will recover without requiring surgery. Some injuries, especially severe stretch injuries or lacerations, will require surgery to repair or reconstruct the affected nerves.
With respect to brachial plexus birth injuries, the majority of babies affected by this condition will make a full recovery with therapy alone, while others may require extensive therapy and possibly surgical intervention. Treatment initially includes:
- Specialized occupational therapy to maintain motion and prevent joint deformity in the affected arm.
- Specialized splints may be required to protect the joints from developing deformities.
In some cases, botulinum toxin (Botox) is used to temporarily weaken “functioning” muscles that are contributing to joint deformity. After the Botox is given, intensive therapy is used to help strengthen the “weakened” muscles and place the shoulder in a better position.
If the injury is severe, surgery may be required to release affected nerves from surrounding scar tissue, repair/reconstruct damaged nerves, or transfer “redundant” nerves to stimulate muscle function.
Additional procedures that may be recommended as children grow, include release of tight muscles or joints, tendon transfers, or joint fusions.
Read more about the different approaches to treatment below:
Treatments
The treatment approach to peripheral nerve problems depends upon the nature of the problem. Many injuries, particularly “stretch injuries” will recover without requiring surgery. Some injuries, especially severe stretch injuries or lacerations, will require surgery to repair or reconstruct the affected nerves.
With respect to brachial plexus birth injuries, the majority of babies affected by this condition will make a full recovery with therapy alone, while others may require extensive therapy and possibly surgical intervention. Treatment initially includes:
- Specialized occupational therapy to maintain motion and prevent joint deformity in the affected arm.
- Specialized splints may be required to protect the joints from developing deformities.
In some cases, botulinum toxin (Botox) is used to temporarily weaken “functioning” muscles that are contributing to joint deformity. After the Botox is given, intensive therapy is used to help strengthen the “weakened” muscles and place the shoulder in a better position.
If the injury is severe, surgery may be required to release affected nerves from surrounding scar tissue, repair/reconstruct damaged nerves, or transfer “redundant” nerves to stimulate muscle function.
Additional procedures that may be recommended as children grow, include release of tight muscles or joints, tendon transfers, or joint fusions.
Read more about the different approaches to treatment below:
Treatments
The treatment approach to peripheral nerve problems depends upon the nature of the problem. Many injuries, particularly “stretch injuries” will recover without requiring surgery. Some injuries, especially severe stretch injuries or lacerations, will require surgery to repair or reconstruct the affected nerves.
With respect to brachial plexus birth injuries, the majority of babies affected by this condition will make a full recovery with therapy alone, while others may require extensive therapy and possibly surgical intervention. Treatment initially includes:
- Specialized occupational therapy to maintain motion and prevent joint deformity in the affected arm.
- Specialized splints may be required to protect the joints from developing deformities.
In some cases, botulinum toxin (Botox) is used to temporarily weaken “functioning” muscles that are contributing to joint deformity. After the Botox is given, intensive therapy is used to help strengthen the “weakened” muscles and place the shoulder in a better position.
If the injury is severe, surgery may be required to release affected nerves from surrounding scar tissue, repair/reconstruct damaged nerves, or transfer “redundant” nerves to stimulate muscle function.
Additional procedures that may be recommended as children grow, include release of tight muscles or joints, tendon transfers, or joint fusions.
Read more about the different approaches to treatment below:
Treatments
The treatment approach to peripheral nerve problems depends upon the nature of the problem. Many injuries, particularly “stretch injuries” will recover without requiring surgery. Some injuries, especially severe stretch injuries or lacerations, will require surgery to repair or reconstruct the affected nerves.
With respect to brachial plexus birth injuries, the majority of babies affected by this condition will make a full recovery with therapy alone, while others may require extensive therapy and possibly surgical intervention. Treatment initially includes:
- Specialized occupational therapy to maintain motion and prevent joint deformity in the affected arm.
- Specialized splints may be required to protect the joints from developing deformities.
In some cases, botulinum toxin (Botox) is used to temporarily weaken “functioning” muscles that are contributing to joint deformity. After the Botox is given, intensive therapy is used to help strengthen the “weakened” muscles and place the shoulder in a better position.
If the injury is severe, surgery may be required to release affected nerves from surrounding scar tissue, repair/reconstruct damaged nerves, or transfer “redundant” nerves to stimulate muscle function.
Additional procedures that may be recommended as children grow, include release of tight muscles or joints, tendon transfers, or joint fusions.
Read more about the different approaches to treatment below:
NeuroMuscular Center Home
NeuroMuscular Center Home
NeuroMuscular Center Home
Art Displays
The student art displays at the main hospital fulfill our vision “to be where the children are,” and spreads joy to patient families, while contributing to our ongoing community outreach efforts.
Display & Artwork Guidelines
Schools may participate by submitting artwork or photography for provisional display on a rotating basis to the hospital.
Artwork or photography submissions should be matted on black or white cardboard. We are currently accepting only 2D art (acrylic, watercolor, printmaking, mixed media) or photography no larger than 18 X 24. This will also allow us to best accommodate pieces within the allotted space.
Rotating artwork and photography will be displayed for the duration of a school calendar year – late August through the end of May.
Registration Form
To participate, please complete the Registration Form below and you will be contacted within two weeks.
When You're Here
At Nicklaus Children's, we understand that a trip to the hospital can be an emotional, and sometimes worrisome, experience for parents and their children. To make your registration a quicker and smoother process we have developed Rapid Registration. Rapid Registration is an initiative established in order to minimize the steps involved during your visit to Nicklaus Children's Hospital by gathering all the needed items prior to your appointment date. If the patient qualifies, you will be receiving a call from one of our dedicated Rapid Registration team members who will verify your demographic information, explain your insurance benefits along with any responsibilities due at time of service.
Below are helpful links with additional information.
Valet Parking Services
As a convenience to our patients and visitors, Nicklaus Children’s Hospital, in collaboration with Town Park valet’s healthcare division, offers complimentary valet service at several campus locations.
Locations and hours of valet services include:
Blue Garage/Advanced Pediatric Care Pavilion: (SW 62 Avenue entrance)
7 a.m. to 9 p.m. (after 9 p.m. keys can be picked up from security)
Devonshire Lobby entrance: (located near SW 57th Avenue and Devonshire Boulevard/60th Court)
7 a.m. to 9 p.m. (after 9 p.m. keys can be picked up from security)
Emergency Department/Outpatient entrance: (follow Emergency Department signs from any entrance)
8 a.m. to 6 p.m. (after 6 p.m. hours keys can be picked up from security)
Want to have your car waiting for you when you return?
Our car request text service can make that happen. Your valet will provide texting information via the parking stub you receive. The color and labeling of the valet parking stub you receive will signify the location of your vehicle. To request your car text 786-789-2095.
- Blue stub = the Blue garage.
- Yellow stub = Yellow garage.
- Pink = Devonshire entrance lobby.
 Tobacco-Free Campus
Tobacco-Free Campus
To protect the children in our care, we are a tobacco-free campus, and smoking is not permitted anywhere on hospital grounds. If you would like help with smoking cessation products, such as Nicoderm gum during your stay, please let your nurse know.
Adaptive Care Program
At Nicklaus Children’s Hospital, our inpatient Adaptive Care Program supports the needs of our neurodivergent population and other eligible children. Our Adaptive Care team works with the families of children with behavioral and developmental needs such as autism, to create a safe and comfortable environment during their hospitalization.
This inpatient program is offered to families of children over the age of 3 who have difficulty coping during hospitalization, or have sensory, behavioral, or communicative needs. If your child would benefit from the Adaptive Care Program, please contact AdaptiveCareTeam@nicklaushealth.org, so our team can provide tools and support for your child’s needs. Our Adaptive Care Patient Resources can also help you plan for a more comfortable experience for your child before, during, and after their hospital visit or stay.
The University of Miami-Nova Southeastern University Center for Autism and Related Disabilities (UM-NSU CARD), South Florida’s leading resource for autism support, recognizes Nicklaus Children’s Hospital as an Autism Friendly Partner.
Patient and Guest Relations
Patient and Guest Relations representatives are available to assist patients and families by answering questions, explaining hospital policies, customer service and helping to resolve issues related to hospital services.
Representatives help families understand their rights and responsibilities and assist in the resolution of complaints, grievances, and treatment disagreements. They are also part of the multi-disciplinary team of care for patients and families and are available to work with families who express concerns about the hospital, its staff and its services.
To contact a Patient and Guest Relations representative, please call 786-624-4400or by filling out an online form.
Mask Wearing Requirements for all Nicklaus Children’s Facilities
As of August 1, 2023, masks are required only in certain circumstances. Examples include persons exhibiting signs or symptoms of an infectious disease, in areas of the facility that are designated sterile, or if the applicable person will be around an immunocompromised patient. This policy applies to all Nicklaus Children's staff members, patients, and visitors two years of age and older. Patients and visitors can contact the patient’s healthcare team (e.g., the treating provider’s office or inpatient unit) and staff members can contact the Infection Prevention and Control Department at ext. 2399.
For More Information
GetWellNetwork
To help you stay connected and informed, Nicklaus Children’s is pleased to offer the GetWellNetwork® in inpatient rooms. This service, available through your in-room television screen, offers many resources, including:
- Email and internet access, including access to our interactive website
- Entertainment (television, movies and games!)
- Our in-house NCHSTV station can be viewed on channel 36
- Information on keeping your child safe in the hospital
- Educational videos related to your child’s specific health needs
- Information on fun activities available for children at Nicklaus Children’s
- Information on hospital programs and services (food service and other conveniences)
- Opportunities to provide feedback on hospital care (compliments and concerns)
Need help with GetWellNetwork? Contact our 24-hour help desk team at 1-888-GWN-DESK (1-888-496-3375).
Planning Your Visit Home
When You're Here (Home)
Community Outreach and Education Programs
Nicklaus Children's Hospital provides community outreach to our local South Florida community by providing classes and courses, in addition to family-centered services to parents, families and professionals.
sarah-fuchs-cardiology
Research Institute Home
Clinical Trials & Research Studies
Headache Program Home
Headache Program Home
Headache Program Home
Clinical Trials & Research Studies
Clinical Trials & Research Studies
Clinical Trials & Research Studies
Clinical Biochemical Genetics Fellowship
Our Partners and Projects
Sanford Health, one of the nation's most extensive rural nonprofit health care system offers primary and specialty care, innovative research, and affordable health plans.
Trans-Hit Bio is the worldwide biospecimen access CRO with the most extensive collection capability for biospecimens and clinical samples through an unrivaled worldwide partnered-network state-of-the-art academic biorepositories and clinical sites.
GENEWIZ is a leading global genomics service company and trusted provider for Sanger sequencing, next generation sequencing, gene synthesis, molecular biology, bioinformatics, and GLP regulatory services. Easily accessible around the world, GENEWIZ is the preferred partner at leading academic, pharmaceutical, biotechnology, agricultural, government, and clinical institutions.
Florida International University (FIU) is Miami's public research university and offers more than 190-degree options, including South Florida's only public schools of law and medicine.
70th Annivers Donation Page
Conditions we Treat
These conditions occur as a result of any damage within the central nervous system that impairs the coordination of muscle activity. It is most commonly related to:
Conditions we Treat
These conditions occur as a result of any damage within the central nervous system that impairs the coordination of muscle activity. It is most commonly related to:
Conditions we Treat
These conditions occur as a result of any damage within the central nervous system that impairs the coordination of muscle activity. It is most commonly related to:
Conditions we Treat
These conditions occur as a result of any damage within the central nervous system that impairs the coordination of muscle activity. It is most commonly related to:
Treatments
While these treatments will not eliminate the underlying neurological problem (e.g. Cerebral palsy) of spasticity, reducing the severity of the spasticity may allow better muscle control and function. Therapy is also an essential component for improving muscle movement.
Treatments
While these treatments will not eliminate the underlying neurological problem (e.g. Cerebral palsy) of spasticity, reducing the severity of the spasticity may allow better muscle control and function. Therapy is also an essential component for improving muscle movement.
Treatments
While these treatments will not eliminate the underlying neurological problem (e.g. Cerebral palsy) of spasticity, reducing the severity of the spasticity may allow better muscle control and function. Therapy is also an essential component for improving muscle movement.
Treatments
While these treatments will not eliminate the underlying neurological problem (e.g. Cerebral palsy) of spasticity, reducing the severity of the spasticity may allow better muscle control and function. Therapy is also an essential component for improving muscle movement.
Cerebral Palsy Program Home
Cerebral Palsy Program Home
Cerebral Palsy Program Home
Cerebral Palsy Program Home
Videos
Videos
Videos
Videos
Motor Disorders Program
Videos
Videos
Videos
Videos
Wheelchair/Seating and Mobility Clinic
Treatments and Procedures
Dr. Burnweit Retirement Party Donation Page
Dental Services (Home)
Dentistry Residency Program
Dental Unit
The 40-foot mobile unit is Nicklaus Children’s Hospital’s latest endeavor to assist families in need as part of its vision “to be where the children are” in South Florida and beyond. In addition to screenings and exams, services can include varnish treatments, dental sealants, oral and health hygiene education as well as referrals for follow-up oral treatment, to underserved families of children who do not have dental insurance.
Please note that the dental services will be offered to the first 25 children on a walk-in basis.
KidsHealthArticle
Join the Biobank
Nicklaus Children's Hospital Biobank Participation Consent
The Nicklaus Children's Hospital Biobank offers a unique opportunity for you, your child, and others in our community to participate in advancing medical research to benefit the health and well-being of future generations. By contributing a small amount of blood, saliva, or other biospecimens, you can help scientists learn:
- How the body works
- How disease develops and affects the body
- How to treat diseases and condition
If you are interested in participating, you will be asked as part of the Self-Administered consent process to:
- Watch the patient education video
- Read the informed consent
- Sign the consent form
Please press the PLAY button to begin the video!
Biobank web consent
Nicklaus Children's Hospital Biobank Participation Consent
Thank you for considering participating. We understand you will not participate at this time.
314 Brain Challenge
Meet the Team
Steven Melnick, PhD., MD
Medical Director, Nicklaus Children’s Biobank

Dr. Melnick, serves as the Medical Director of the Nicklaus Children’s Biobank (NCB) with responsibility for oversight of all aspects of this project and for assuring compliance with all policies and procedures by NCB staff.
Dr. Melnick received a B.Sc. degree in Physics at McGill University, Montreal, Quebec. Later he pursued a doctoral research in Chemical Physics and earned a Ph.D., at McGill University, Department of Chemistry in the field of nuclear quadrupole resonance spectroscopy. Following a Post-doctoral Fellowship in the same field, he began Medical School at Queen’s University, Kingston, Ontario and subsequently, residency training in Pathology at Mount Sinai Medical Center, Miami Beach, Florida. He continued his career in medicine as an attending Pathologist at Miami Children’s Hospital (now Nicklaus Children’s Hospital). In addition to his clinical activities, he established a research program in cell and molecular biology, with a particular focus on cancer research including ethnobotanical drug discovery. Currently, Dr. Melnick serves as Chief, Department of Pathology and Clinical laboratories at Nicklaus Children’s Hospital.
Meet the Team
Food and Nutrition Home
Videos
Timeline of Milestones and Major Naming Gifts

In an effort to give every child the chance at a healthy future, we rely on community support from people and organizations like you. Here, we recognize the incredible impact of visionaries, volunteers and generous philanthropists who partner with us in meaningful ways to provide the very best care to our children and families when they need us most. Ongoing philanthropic support has helped us innovate, improve patient outcomes, carry out groundbreaking research, acquire state-of-the art equipment and expand programs and services that have made a difference for generations of children.
In this historical timeline, we highlight several significant moments and transformational gifts that have been instrumental to our hospital’s remarkable growth and progress. However, we cannot understate the impact of the hundreds of thousands of supporters who have given and continue to give generously year after year. No matter the size, every contribution helps to change and save lives, and for this, you have our heartfelt thanks.
2023
A transformational $15 million gift from South Florida philanthropists Helen and Jacob Shaham to further elevate world-class pediatric cancer care and research through the hospital’s cancer and blood disorders institute. In recognition of the gift, the program now proudly bears the name, the Helen & Jacob Shaham Cancer & Blood Disorders Institute.
A $1 million donation from the Saka family to support various programs including the Adaptive Care Program, music therapy, palliative care, children’s experiences, and the Cardiac Intensive Care Unit (CICU).
The Batchelor Foundation issued a $250,000 grant to benefit the Mobile Dental Unit. Other grantors include Delta Dental, Florida Blue Foundation and the Kirk Foundation, with new 2023 support for the Mobile Dental Unit totaling $357,000.
Hyundai Hope on Wheels, STOP Children’s Cancer of Palm Beach County and Ayúdame a Vivir Foundation issued grants totaling $192,000 overall for cancer research.
2022
A $25 million gift from Ken Griffin to advance surgical care at Nicklaus Children’s, naming the Kenneth C. Griffin Surgical Tower, which opened in 2024 as one of the most innovative surgical facilities in the country..
A $2 million gift from Nicklaus Children's Health Care Foundation to support various areas of the hospital including cardiac surgery, child life, cancer research, and pediatric services at Jupiter Medical Center.
A $1,149,000 grant from the Glenn W. Bailey Foundation to provide innovative healthcare technologies to patients, including establishment of the PGx genetic testing program and support of the Cardiac Surgery Advanced Projects Laboratory.
A $1 million planned gift from the estate of Carlos Malamud to support pediatric epilepsy services and programs.
A $1 million gift from Michelle and Michael Hagerty to support the hospital’s greatest needs.
A $1 million gift from VoLo Foundation to support the new surgical tower.
A $300,000 gift from John Paul Medina to support the creation of the Medina Innovation Lab that will leverage technology to improve the patient experience.
The Sourcing Group, LLC donated personal protective equipment for frontline clinicians, with a total value of $260,000.
A $250,000 gift from The Altman Family Foundation, Inc. to support the Patient Assistance Fund for families with unmet financial need.
A $250,000 gift from Juan Carlos and Vivian Mas to support the new surgical tower.
A $250,000 bequest gift from Melisa and Fred Levenson to support the hospital’s greatest needs.
2021
A $5 million gift from Michelle and Michael Hagerty to expand and enhance the inpatient Psychiatry Unit, doubling its current capacity, to treat and care for patients.
A $5 million gift from VoLo Foundation, thanks to co-founders David S. Vogel and Thais Lopez Vogel. The donation will advance pediatric surgery, with an emphasis on cardiac surgery, supporting important advancements in state-of-the-art medical technologies and innovations, medical education and expansions in surgical operating suites.
Coral Gables healthcare entrepreneur Miguel “Mike” B. Fernandez donated his personal Sikorsky ® S76 C+ helicopter, which will benefit the LifeFlight ® critical care transport team at Nicklaus Children’s.
A major grant from The Frederick A. DeLuca Foundation to support autism care and psychiatry.
A major grant from Rotary Club of Key Biscayne and the Rotary Club of Windsor Roseland, Canada to expand access to telebehavioral health screenings.
A major grant from The Taft Foundation to implement the use of virtual reality (VR) to reduce child anxiety in clinical settings.
2020
The Samuel C. Cantor Charitable Trust and Eddy and Helaine Cantor make gift that names the Pediatric Intensive Care Unit Lobby
A gift from The Honda Classic, in partnership with the Nicklaus Children’s Health Care Foundation, benefits pediatric services in Palm Beach County and free dental care provided by the Mobile Dental Van for underserved kids
A gift from the Miami Dolphins supported the care of children with diabetes and sickle cell disease, as well as research related to COVID-19
A significant gift from Foundation board member Michelle Hagerty and husband Michael support the hospital’s greatest needs, naming the Michelle & Michael Hagerty Advanced Pediatric Care Pavilion Plaza
Frank Scaduto donated a significant gift to benefit the neonatal intensive care unit
2019
Linda and Morton Bouchard make a generous gift that names The Morton & Linda Bouchard Healing Garden in the APCP
The Esrick Dream Foundation names the Cardiac Intensive Care Unit Floor in the APCP
Lynn and Frank Scaduto make a generous gift that names the Neonatal Intensive Care Unit Floor in the APCP
2018
Ravneet Chowdhury, a Nicklaus Children’s Hospital Foundation chair and husband Anand Chowdhury, make generous contributions that name the Nirvair Chowdhury Midtown Outpatient Center in honor of their son, Nirvai
2017
Carlos J. Arboleya, Sr., a former Miami Children’s Hospital Foundation board member, makes generous gift that names
The Marta & Carlos J. Arboleya, Jr. Pediatric Intensive Care Floor in the APCP in honor of his late wife and son
Ruth Waltz makes a generous gift that names the Cardiac Intensive Care Unit Lobby in the APCP
Lawrence J. and Florence A. De George Charitable Trust makes generous gift to further the Telehealth initiative
2016
Trust of Rita Auerbach Wallach provides a generous legacy gift that names the APCP Lobby
Cherie and Jack Denson make generous gift that names the Denson Family Neurology-Neurosurgery Floor in the APCP
Laurie and Robert Lucks make a generous gift that names the Lucks Family Neonatal Intensive Care Floor
2015
Raul Rodriguez names The Raul Rodriguez Fracture Care Center
Pledge from the Barbara and Jack Nicklaus’ Nicklaus Children’s Health Care Foundation renamed Miami Children’s Hospital as Nicklaus Children’s Hospital and later also Nicklaus Children’s Health System
Gladys M. Stewart leaves a generous gift from her estate to help sick children; Main Campus PCC named The Gladys M. & Frederick Stewart Pediatric Care Center
2012
The Anthony R. Abraham Foundation names the Orthopedics Lobby
2011
Miami Children’s Hospital Foundation launches the five-year “Together For The Children” campaign that raised $150 million for the hospital
Florence Groover Frank – “Grande Dame” of the Foundation leaves a sizeable estate gift
The Miguel “Mike” B. Fernandez Family names The Miguel “Mike” B. Fernandez Family Pediatric Trauma Center
2010
A generous bequest from the Estate of Ralph George Hasker funds an entertainment area in the newly expanded Emergency Department, which is named the Hasker Teddy Bear Zone
2006
Florida Blue gift names the Brain Institute’s “Blue Concourse” and continues to serve as a steadfast partner of the hospital and foundation
2002
Samuel Blank & Family Foundation – Million Dollar Club members – names the Sam & Bea Blank Pavilion
1996
The Dan Marino Foundation makes a generous gift that names the Dan Marino Outpatient Center in Weston
1994
U.S. News & World Report names Miami Children’s Hospital the best pediatric institute in the Southeast
1992
The Batchelor Foundation names the George E. Batchelor Research and Academic Pavilion and continues to support the hospital
1991
Bettina Wattles, a generous patron of Miami Children’s Hospital Foundation, names the Roger & Bettina Wattles Wing and the Roger & Bettina Wattles Foundation Building
1990
The Miami Children’s Hospital Pediatric Research Institute opens its doors
Solomon Klein Foundation gift names the Solomon Klein Pavilion
1987
Became a Children’s Miracle Network Hospitals® member, nearly $40 million raised to date for Nicklaus Children’s by partner organizations
James L. Knight makes significant gift that names the main hospital building the Mary Ann Knight International Institute of Pediatrics after his late wife
1986
Gifts from benefactors and founders Bernice & Harry Simone name The Harry & Bernice Simone Wing
The Ambassador David M. Walters International Pediatric Hall of Fame recognizes its first inductees: Walt Disney, Dr. Jonas Salk, Dr. Helen Taussiq and Bob Keeshan (Capt. Kangaroo); 75 world-renown champions of children are now members of the Hall of Fame
1983
Variety Children’s Hospital becomes Miami Children’s Hospital
MCH Foundation launches a three-phase campaign called “A Campaign for Our Children; Phase I raised $49.8 million to fund construction; Phase II raised $25 million to establish a pediatric research institute; and Phase III raised $25 million to help establish an academic presence at the hospital
1982
Ambassador David M. Walters activates Miami Children’s Hospital Foundation
1980
Estate of Sue-Byrd Pentland (wife of Founder Col. Robert C. Pentland) makes a significant legacy gift
1979
With the generous support of United True Order Sisters (UOTS), the hospital dedicated a 2,000 sq. ft. facility dedicated solely to expanding pediatric/oncology services. The newly named John Wayne Pavilion recognized UOTS – Miami 43 support of pediatric hematology/oncology
1960s and 70s
Variety Children’s grows to meet the needs of the growing Miami population, including an influx of refugees fleeing communist Cuba
1958
Variety Children’s is recognized as a teaching hospital with a focus on pediatrics
Variety Children’s Research Foundation Laboratory named in honor of Jack Bell, a journalist who was the driving force behind the Committee of 100, a Variety Club group committed to raising $100,000 a year for the hospital and which raised $117,000 in 1958 to match a government grant - guests at the dedication include Debbie Reynolds and Mickey Spillane
1956
Obelisk erected on hospital grounds honoring founders/ benefactors: Col. Robert Pentland, Jr., George C. Hoover, Roscoe Brunstetter and Jack Cleary
1950
With funding from Variety International, Variety Children’s Hospital opens its doors just as the polio epidemic was encompassing the United States
1947
The Crippled Children’s Society turns over management and maintenance of the hospital to Variety International’s (a leading charitable organization affiliated with the entertainment industry) Club Tent 33
1941
Dr. Arthur H. Weiland, a leading orthopedic surgeon, dreams of building a hospital in South Florida for crippled children; a vision that will be realized within a few years
1939
Patsy Carr writes letter to Santa asking for a children’s hospital in our community
As you read through our donor history, we invite you to help us be there for the  children by making an investment in their future through a contribution to Nicklaus Children's Hospital Foundation.
children by making an investment in their future through a contribution to Nicklaus Children's Hospital Foundation.
Coronavirus Updates
This page was last updated on: {% DocumentContext.CurrentDocument.DocumentLastPublished |(user)MCH-rherrera1|(hash)0aec6678707b7dce039185d888d8d3ea32b6ef370585b492f52f807d628796b1%}
COVID-19 Vaccines for Kids
The COVID-19 vaccine is available for adults and children through a variety of sources in our community. The link below can help you find locations near you. In addition, pharmacy chains, including CVS, Publix and Walgreens, also offer the vaccine. Please check the website of the pharmacy of your choice for more information.
Click here for a link to the Miami-Dade County COVID-19 Vaccine Locator
COVID-19 Testing (Children without Symptoms)
Our emergency department and urgent care centers provide COVID-19 testing for children with associated symptoms as part of a complete medical evaluation.
Due to very high volumes in local emergency rooms and urgent care centers, associated with the pandemic, we encourage families of children who do not have symptoms of illness to visit a local COVID-19 testing center. These centers offer appointments and can often provide test results within 24 to 48 hours.
Click here for a link to the Miami-Dade County COVID-19 Testing Site Finder
COVID-19 Testing (Children with Symptoms)
Nicklaus Children's Hospital's Emergency Department and Urgent Care Centers provide testing for children who are displaying symptoms of COVID-19 such as:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
COVID-19 Test Results
Parents can access the child's medical records and covid test results online by visiting MyKids Patient Portal. For information about MyKids and instructions on how to register, please visit nicklauschildrens.org/Patient-Portal
{$NCH.NCHSAnywhereBox_Specialty$}
Visitor Policies and Protocols
Visitor Policies and Protocols
We continue to use protocols recommended by the Centers for Disease Control regarding the novel COVID-19 virus. Our priority, as always, is the health and safety of all our patients and visitors. Due to the current higher-than-usual rate of respiratory infections in our community, please note we are reinforcing changes to our visitor policy in all our care settings. We ask patient families to adhere to the following practices to ensure the safety of the children in our care.
Safety Protocols for All Visits
- All parents/guardians accompanying children must be free of signs and symptoms of infectious disease, including cough, runny nose, rash, vomiting and fever. Please notify the medical provider caring for your child if you or anyone else in the home has a fever, cough, rash, shortness of breath, or any other sign of respiratory infection.
- We encourage all visitors to wash or sanitize hands frequently.
For Inpatient Visits
- Each hospitalized patient may have up to four caregivers/visitors (including siblings) at one time. Visitors are limited to the same four people per 24-hour period. Siblings are only allowed if there are no other alternatives for their care. Babies who are breastfeeding are an exception. Siblings must remain in the patient room.
- In COVID-19 care areas, only one adult visitor is permitted in a 24-hour period. The visitor must stay in the room at all times. If required to leave, the visitor must be accompanied from the facility by a healthcare worker.
- Any family member remaining alone in a room with a patient must be age 18 or older.
For Emergency Room, Urgent Care, Physician Offices, Radiology, Diagnostic Services, Rehabilitation and Dental Services
- A maximum of two caregivers/visitors (including siblings) can accompany a patient who has an appointment at any of our clinics/centers, medical offices, or who visits the Emergency Department or one of our Urgent Care Centers or other above-listed services.
- Please do not bring additional family members or friends to these visits (especially children under 12 years old).
For Ambulatory Surgery Visits
- Only one visitor can accompany the patient. No one under the age of 18 is permitted.
How to decide if you should be tested or seek care
How to decide if you should be tested or seek care
Provided by the CDC: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
Not everyone needs to be tested for COVID-19. Here is some information that might help you make decisions about seeking medical care or testing.
- Most people have mild illness and are able to recover at home without medical care. They may not need to be tested.
- There is no treatment specifically approved for people who have COVID-19.
- If you think you may be sick, stay home and consult with your healthcare provider on the need for testing.
CDC has guidance for who should be tested, but decisions about testing are at the discretion of state and local health departments and/or individual clinicians.
- Clinicians should work with their state and local health departments to coordinate testing through public health laboratories, or work with clinical or commercial laboratories.
Coronavirus (COVID-19) Updates
Incident Command Internal Communications
Incident Command External Communications
COVID19Fund
Masks for Miami
Nicklaus Children’s COVID-19 Fund Ambassador Toolkit
Telehealthspecialties

Telehealth Specialty Appointments
Telehealth services may be available for certain specialty appointments depending on the nature of the condition, or reason for the visit. The following specialties are currently offering telehealth services:
-
Adolescent Medicine
-
Allergy & Immunology
-
Cardiology
-
Dental Services
-
Endocrinology
-
Gastroenterology
- Genetics
- General Pediatrics
-
Infectious Diseases
-
Nephrology
|
- Neurosurgery
- Ophthalmology
-
Orthopedics
-
Otolaryngology (ENT)
-
Plastic Surgery
-
Psychiatry
-
Psychology
-
Rehabilitation Services
-
Rheumatology
|
To schedule a telehealth appointment with one of these specialties, please call us at 1-888-624-2778
Request an Appointment
Community Health Blog
Telehealth Services FAQ
Q: What is Nicklaus Children's Pediatric Virtual Care?
A: Nicklaus Children’s Pediatric Virtual Care allows patients and their caregivers to connect with providers from the comfort of their home through a computer, tablet or mobile app.
Q: Who is available for consultations?
A: Consultations can be scheduled with individual specialists or a team of multi-disciplinary subspecialists as needed. Medical translation services are also provided when needed to support communications.
Q: What services are currently offered through Nicklaus Children's Pediatric Virtual Care Platform?
- Non-emergent pediatric care
- Pediatric Primary Care
- Complex multi-disciplinary team consultations
- Nutrition Services
- Mental/Behavioral Health
- Social Services
- Support Groups
- Care/Case Management
- Second opinions
- New patient and follow-up consultations for many pediatric specialties and subspecialties:
- Adolescent Medicine
- Allergy & Immunology
- Cardiology
- Dental Services
- Endocrinology
- Gastroenterology
- Genetics
- Infectious Diseases
- Nephrology
- Neurosurgery
- Ophthalmology
- Orthopedics
- Otolaryngology (ENT)
- Plastic Surgery
- Psychiatry
- Psychology
- Rehabilitation Services
- Rheumatology
Q: Will my insurance cover a Telehealth visit?
A: Insurance companies are currently reimbursing for Telehealth visits. For details on what your insurance will help cover, please contact your insurance carrier for more information. The specific practice or Customer Care Center team may also be able to answer basic insurance-related questions.
Q: Can I obtain prescriptions? What is the process?
A: If the provider determines you will need prescriptions following your consultation, they will provide this information to your pharmacy of choice for pick up.
Q: How do I schedule an appointment?
A: You can schedule a Telehealth appointment with a pediatric specialist by contacting either the Nicklaus Children’s Customer Care Center (1-888-624-2778) or the provider’s office directly and requesting a Telehealth consult. If the provider determines you qualify for a Telehealth visit, the care team will help get you setup before your scheduled consult date.
Q: Will I be able to see my usual provider via the Telehealth appointment?
A: If your provider is offering Telehealth services, you should be able to connect with them via Nicklaus Children's Pediatric Virtual Care. Please confirm your provider’s availability when scheduling your appointment(s) with their staff or by calling the Customer Care Center at 1-888-624-2778.
Q: How do I get started?
A: Download the Nicklaus Children's Pediatric Virtual Care app on the Apple Store or the Google Play Store and create an account.
Q: Who do I contact for technical assistance?
A: To reach the Nicklaus Children's Pediatric Virtual Care Telehealth Center at Nicklaus Children's Hospital, please email telehealth.office@nicklaushealth.org. You may also visit the website at: www.nicklauschildrensvirtualcare.org/
Nicklaus Children's Pediatric Specialists Home
Community Outreach Home
robert-hanfland-cardiovascular-surgery
Infectious Diseases Home
Lipid Clinic Home
Lipid Clinic Home
Appointment: Brachial Plexus
Thank you
Community Health Blog Home
UCC Safety Spanish
Estimado Paciente y Familia,
El Coronavirus (conocido como COVID-19), nos ha afectado a todos en maneras que no pudiéramos haber anticipado hace unos meses atrás. Nicklaus Children’s se complace en poder servirle a usted y su familia mientras nos esforzamos a navegar esta pandemia juntos.
La seguridad y el servicio siempre son nuestra prioridad en los Centros de Cuidados Urgentes de Nicklaus Children’s. Debido al Coronavirus, nuestros equipos médicos han aumentado las prácticas de seguridad para proteger a todos que visitan nuestros centros.
Espero que tome un momento para ver este video y nuestras nuevas políticas en acción.
Los Centros de Cuidados Urgentes de Nicklaus Children’s están actualmente abiertos en las ciudades de:
Para más información sobre nuestros centros y ubicaciones, visite:
nicklauschildrens.org/CuidadosUrgentes
Sinceramente,
Dra. Maria Ramon-Coton
Directora Médica, Centros de Cuidados Urgentes de Nicklaus Children’s
COVID19-tool
ED Safety Spanish
Cuando Suceden Emergencias, No Demore la Atención
En Nicklaus Children’s Hospital, la seguridad, salud, y bienestar de los niños de la comunidad es nuestra primera prioridad. Hospitales en el Sur de la Florida, también como en otras partes de la nación, están experimentado un aumento en pacientes con heridas y enfermedades que empezaron varios días atrás.
Acuérdese, cuando una emergencia surge, es importante buscar atención médica
inmediatamente. El esperar a buscar atención médica puede ser peligroso para todos, especialmente niños que tal vez no puedan explicar cómo se sienten.
El
Departamento de Emergencias de Nicklaus Children’s y el Miguel “Mike” B. Fernandez and Family Pediatric Trauma Center, el único centro de trauma pediátrico independiente del sur de la florida, ha aumentado sus medidas de seguridad para ayudar a mantenerlos saludables:
- Pedimos que adultos y niños con más de dos años de edad lleguen a nuestras instalaciones con mascarillas puestas. Nuestro personal le proveerá una mascarilla si no tiene una.
- Pacientes, padres/guardianes, visitantes y empleados recibirán una prueba de temperatura al llegar a una de las entradas del hospital.
- Al llegar a la sala de emergencias, le preguntaremos una serie de preguntas para determinar la zona apropiada para el cuidado de su hijo/hija.
- Hemos agregado señales de distancia física en las áreas comunes para recordarles de mantener seis pies de distancia. Hemos quitado los juguetes, libros y revistas de estas áreas.
- También hemos instalado más estaciones de gel desinfectante por todo el hospital.
Recuerde, si su hijo(a) tiene una emergencia médica, visite la sala de emergencias más cercana o llame al 911 inmediatamente. Para más información sobre las medidas de seguridad que hemos implementado, visite,
Nicklauschildrens.org/Covid19seguridad
Este video de Nicklaus Children’s Hospital les muestra lo que pueden esperar en su próxima visita al hospital o sala de emergencias:
Rehab Safety Spanish
Un mensaje importante de los servicios de rehabilitación de Nicklaus Children's Hospital
Estimada familia de pacientes:
Muchos de nuestros pacientes y sus familias han expresado interés en reanudar las terapias en persona para sus hijos. Por favor tenga en cuenta que estamos ofreciendo terapias, tomando precauciones de seguridad, en las oficinas de los servicios de rehabilitación en Nicklaus Children’s Hospital, así como en nuestras instalaciones en Miami Lakes, Miramar, Palm Beach Gardens y West Kendall.
Las nuevas prácticas de seguridad incluyen:
- Citas programadas se han reducido para minimizar movimiento en áreas comunes.
- Solo un adulto puede acompañar a un niño o adolescente a las citas (estamos adaptando estas prácticas para para niños con necesidades especiales que requieren asistencia adicional).
- Todo el personal, visitantes y pacientes de dos años en adelante deben usar mascarillas durante la visita.
- Una prueba de temperatura se realiza para todo el personal, visitantes y pacientes al llegar a la instalación.
- Cualquier persona con una temperatura elevada, o que ha sido expuesto al COVID-19 en el hogar, debe reprogramar su cita para una fecha posterior.
- El acceso rápido a las salas de terapia minimiza el tiempo en espacios compartidos.
- Señales de distanciamiento físico se encuentran en todos los espacios compartidos.
- Hemos aumentado nuestras políticas de limpieza para todos los cuartos de terapias y espacios compartidos.
Este video muestra cómo estamos implementando estas prácticas para la seguridad de todos. Esperamos que se tome un momento para verlo.
Para obtener más información o si desea programar una cita, llame al 1-877-255-8437.
Gracias,
Jessica Thomas, MS, CCC-SLP
Directora de Operaciones,
Rehabilitación de pacientes hospitalizados/ambulatorios
Safety Newsletter Spanish
Aumentan Las Heridas en Casa Cuando Hay Más Tiempo Libre y se Hacen Muchas Cosas a La Misma Vez
A medida que los niños pasan del aprendizaje virtual a las rutinas de verano, es importante que los padres y guardianes estén conscientes de que cuando hay más tiempo libre, aumentan las heridas accidentales. Aunque los riesgos de sufrir heridas durante el verano están presentes todos los años, los expertos han observado que hay un aumento de estos eventos este año, debido a que las familias practican el distanciamiento social en casa.
“El problema con COVID-19 ha sido que muchos padres están trabajando desde sus casas y no pueden estar atentos a qué hacen los niños todo el tiempo”, explicó Malvina Duncan, coordinadora de Prevención de Lesiones en Nicklaus Children’s Hospital y coordinadora de Safe Kids en el condado de Miami-Dade.
“Lamentablemente, en la Florida hemos visto un aumento del 37.5 por ciento en el número de muertos por ahogamiento con respecto a esta misma época el año pasado. A través de la promoción de la concienciación entre los padres y tutores, esperamos combatir esta lamentable tendencia,” dijo Duncan.
Es importante que todos los familiares y amigos que ayuden a cuidar a los niños este verano sean conscientes de los peligros que hay en el hogar:

Seguridad en el Agua
- Siempre se debe supervisar activamente a los niños cuando estén cerca o dentro de masas de agua. Use barreras, como cercas para piscinas, puertas y ventanas que puedan cerrarse con traba si están cerca de cualquier masa de agua, ya sea una piscina, un lago, un canal, el mar u otros.
- Los padres y otros guardianes deben recordar que el ahogamiento es un evento silencioso. La única forma de prevenir los ahogamientos es que un adulto responsable vigile de cerca a los niños cuando estén en el agua.

Productos de Limpieza Para el Hogar
- Las familias ahora están haciendo más limpieza que antes debido a la pandemia de COVID-19. Muchos productos de limpieza pueden parecer como una bebida tentadora para los niños pequeños. Mantenga estos productos fuera del alcance de los niños y úselos solamente según las instrucciones del fabricante.
Seguridad de los Juguetes y Equipos
- Mientras los niños estén en el patio o afuera dando un paseo, recuerde que deben jugar de manera segura: Deben usar juguetes apropiados para su edad y equipos de seguridad, como cascos, cuando usen bicicletas, monopatines, patinetas, etc.
- Mantenga los objetos y juguetes pequeños, al igual que las cuerdas, fuera del alcance de los niños pequeños para prevenir el atragantamiento y la estrangulación.
No Demore en Buscar Atención Médica si el Niño Está Lesionado o Enfermo
En las salas de emergencias y los centros de cuidados urgentes de todo el país, se están viendo casos de niños con lesiones y enfermedades que se complicaron debido a las demoras en buscar tratamiento. Asegúrese de que su hijo reciba la atención adecuada en el momento adecuado.
El Departamento de Emergencias de Nicklaus Children’s cerca de Coral Gables y los centros de cuidados urgentes de Nicklaus Children’s en Doral, Hialeah, Homestead, Palm Beach Gardens, Palmetto Bay, Miami Lakes, Midtown, Miramar, West Bird y West Kendall están disponibles para atenderlo. Todos cuentan con prácticas de seguridad mejoradas para la protección de todo el mundo.
Para obtener más información y consejos sobre salud y seguridad, visite: Nicklauschildrens.org/seguridad
West Bird UCC Reopening Email Spanish Landing Page
El Centro de Cuidados Urgentes de Nicklaus Children’s en West Bird reanude sus servicios con prácticas de seguridad y salud expandidas
El Centro de Cuidados Urgentes en West Bird ha reanudado sus servicios para servir a su familia con prácticas de seguridad aumentadas debido al Coronavirus (Conocido como COVID-19) para la protección de todos.
El horario del Centro de Cuidados Urgentes es de 11 a.m. a 10 p.m. de lunes a domingo.
El centro ofrece atención personalizada y rápida de lesiones menores y enfermedades de bebés, niños, adolescentes y adultos jóvenes menores de 21 años. Los servicios son proporcionados por expertos en atención pediátrica, dirigidos por médicos certificados por la junta.
Vea nuestro video de practicas de seguridad!
Prácticas de seguridad mejoradas para que te sientas como en casa
El centro ha implementado las siguientes medidas de seguridad:
Visitantes limitados: Le pedimos que solo un adulto acompañe a un niño al centro de cuidados urgentes. Para niños con necesidades especiales, un adulto adicional puede acompañar al niño si es necesario.
Mascarillas: Todos los adultos y niños mayores de dos años deben usar mascarillas al entrar a la instalación. Todo el personal también estará usando mascarillas y otros equipos de protección personal.
Detección: A todos los pacientes, el personal y los visitantes se les tomará la temperatura antes de entrar al centro.
Registro rápido: Adentro de nuestra instalación, tenemos un proceso de registro rápido. Los pacientes son trasladados a las habitaciones lo más rápido posible.
Distanciamiento físico: Existen señales visuales para ayudar a todos a mantener una distancia de seis pies de los demás.
Limpieza profunda: Cada sala de examen se limpia profundamente después de cada paciente. Además, las áreas comunes se limpian continuamente, con atención especial a los puntos de contacto, como los reposabrazos, las manijas de las puertas y más.
Higiene de manos: Alentamos a las familias que usen las estaciones de desinfección de manos que proporcionamos después de tocar cualquier superficie.

Condiciones que tratamos
Algunas de las condiciones que tratamos en los
Centros de Cuidados Urgentes de Nicklaus Children’s incluyen:
- Lesiones, heridas, cortes y golpes (incluyendo puntos de sutura)
- Picaduras de insectos, picaduras, erupciones y quemaduras menores
- Reacciones alérgicas menores
- Lesiones por tensión muscular
- Enfermedades respiratorias
- Dislocaciones y torceduras (incluyendo rayos X y entablillados)
- Dolores de oído e infecciones del oído
- Infecciones del tracto urinario
- Los virus, como la enfermedad de manos, pies y boca
- Vómitos, diarrea y deshidratación menor
El Centro de Cuidados Urgentes en West Bird
11449 SW 40 Street
Miami, FL 33165
786-624-4200
Emergency Dept. Home
Urology Home
Pulmonology Home
Review-Dr-Drossner
Review-Dr-Khan
Review-Dr-Burke
Review-Dr-Lopez
In Memory of Mary Turnbach
Treatments and Procedures
Rehab Reopening Spanish
Un mensaje importante sobre la reanudación de los servicios de rehabilitación de Nicklaus Children's Hospital
Estimada familia de pacientes:
Nicklaus Children's Health System se complace en comunicar que hemos reanudado la mayoría de nuestras oficinas de servicios de rehabilitación, incluidas las del campus principal, así como en Doral, Miami Lakes, Midtown, Miramar, Palm Beach Gardens, Palmetto Bay, West Kendall y Weston.
Cómo comenzar la terapia de su hijo(a)
Favor de empezar llamando al departamento de servicios de rehabilitación al 1-877-255-8437. Dependiendo de la fecha de la última cita de rehabilitación de su hijo(a), puede ser necesario obtener una nueva receta de su pediatra y una nueva evaluación de servicios de rehabilitación para volver a recibir los servicios. Nuestro equipo le ayudará a navegar estos pasos para comenzar. Una llamada a nosotros es el primer paso.
La seguridad es nuestra principal prioridad
Hemos implementado las siguientes prácticas en cada centro para proteger a los pacientes, los familiares y el personal:
- Se ha reducido la cantidad de citas programadas para minimizar la congregación en áreas comunes.
- Solo un adulto puede acompañar a un niño o adolescente a las citas (estamos adaptando estas prácticas para para niños con necesidades especiales que requieren asistencia adicional).
- Todo el personal, visitantes y pacientes de dos años en adelante deben usar mascarillas durante la visita.
- Una prueba de temperatura se realiza para todo el personal, visitantes y pacientes al llegar a la instalación.
- Cualquier persona con una temperatura elevada, o que ha sido expuesto al COVID-19 en el hogar, debe reprogramar su cita para una fecha posterior.
- Acceso rápido a las salas de terapia para minimizar el tiempo en espacios compartidos.
- Señales de distanciamiento físico se encuentran en todos los espacios compartidos.
- Hemos aumentado nuestras políticas de limpieza para todos los cuartos de terapias y espacios compartidos.
Este video muestra cómo estamos implementando estas prácticas para la seguridad de todos. Esperamos que se tome un momento para verlo.
Gracias, esperamos poder ayudarlo a reanudar el plan terapéutico de su hijo.
Sinceramente,
Jessica Thomas, MS, CCC-SLP
Directora de Operaciones,
Rehabilitación de pacientes hospitalizados/ambulatorios
In Memory of Anand Chowdhury
Trauma Services Home
Patient Stories
Emergency Department
Treatments and Procedures
Treating epilepsy can be challenging since each child is unique and will respond differently to various kinds of treatment. Treating epilepsy can be challenging since each child responds differently to various kinds of treatment. Our experienced team will help your family understand the best treatment options available and what might work best for your child.
Our Comprehensive Epilepsy Center offers state-of-the-art technology for patients seeking specialized pediatric treatment and care for managing epileptic seizures.
Treatments and Procedures
Treating epilepsy can be challenging since each child is unique and will respond differently to various kinds of treatment. Treating epilepsy can be challenging since each child responds differently to various kinds of treatment. Our experienced team will help your family understand the best treatment options available and what might work best for your child.
Our Comprehensive Epilepsy Center offers state-of-the-art technology for patients seeking specialized pediatric treatment and care for managing epileptic seizures.
Treatments and Procedures
Treating epilepsy can be challenging since each child is unique and will respond differently to various kinds of treatment. Treating epilepsy can be challenging since each child responds differently to various kinds of treatment. Our experienced team will help your family understand the best treatment options available and what might work best for your child.
Our Comprehensive Epilepsy Center offers state-of-the-art technology for patients seeking specialized pediatric treatment and care for managing epileptic seizures.
Treatments and Procedures
Treating epilepsy can be challenging since each child is unique and will respond differently to various kinds of treatment. Treating epilepsy can be challenging since each child responds differently to various kinds of treatment. Our experienced team will help your family understand the best treatment options available and what might work best for your child.
Our Comprehensive Epilepsy Center offers state-of-the-art technology for patients seeking specialized pediatric treatment and care for managing epileptic seizures.
Appointment: Fetal Care Services
Thank You
Thank you! Your request has been submitted.
A team member will contact you regarding your inquiry within the hours you have indicated.
Return to the Fetal Care CenterEvent Sign In
Thank you
Diamond Auction
Patient Resources
Exercises and Application of Orthosis
Home Stretching Program
Perform these passive stretches for all upper extremity joints of affected arm. The exercise program is designed to prevent joint contractures, loss of motion and muscle tightness which can result in abnormal postures and movement patterns, as well as limit arm use.
How often should my child do these exercises?
Twice daily, with the exception of the external rotation stretches. Refer to this stretch for details. Therapist will guide which stretches/joints should be performed more frequently.
Patient Resources
Exercises and Application of Orthosis
Home Stretching Program
Perform these passive stretches for all upper extremity joints of affected arm. The exercise program is designed to prevent joint contractures, loss of motion and muscle tightness which can result in abnormal postures and movement patterns, as well as limit arm use.
How often should my child do these exercises?
Twice daily, with the exception of the external rotation stretches. Refer to this stretch for details. Therapist will guide which stretches/joints should be performed more frequently.
Meet the Trauma Team
Dispositions
NCPS Heart Program Virtual Care Spanish
Un mensaje importante sobre el programa de cardiología de
Nicklaus Children's Hospital
Estimados padres y guardianes:
Gracias por elegir el Programa Cardíaco de Nicklaus Children’s Hospital para la atención de su hijo. La salud y seguridad de su hijo y su familia continúan siendo nuestra principal prioridad.
Muchas familias han preguntado por las citas de telesalud, de modo que nos complace proveerles una lista de médicos de nuestro consultorio que pueden estar disponibles para consultas a través de nuestro programa Nicklaus Children’s Pediatric Virtual Care, según la naturaleza de la afección del paciente o el motivo de la visita.
Queremos informar a las familias que deseen vernos en una cita en el consultorio que estamos abiertos y listos para servirles con medidas de seguridad mejoradas en la era del COVID19, a fin de brindar una experiencia sin inconvenientes. Visiten nuestra página web exclusiva para conocer más detalles y obtener las últimas actualizaciones sobre las políticas para visitantes y los servicios hospitalarios.
A seguir, encontrará una lista de los médicos y enfermeras practicantes del Programa Cardíaco de Nicklaus Children’s Hospital que actualmente ofrecen consultas virtuales:
Si tienen alguna pregunta o si desean programar una cita, llámenos al 305-662-8301 y un miembro de nuestro equipo, con gusto los atenderá. Las visitas presenciales y virtuales también pueden solicitarse en línea visitando: nicklauschildrens.org/Citas.
Esperamos poder seguir atendiéndolos.
Sinceramente,
Dr. Anthony Rossi
Director de la División de Cardiología de Nicklaus Children’s Hospital
Jefe de la Sección de Medicina Cardiovascular de Nicklaus Children’s Pediatric Specialists (NCPS)
Patient Resources

Neurodynamic Warm Up

Static Stretches, Dynamic Stretches and Eccentric Isometrics
Exercises & Videos for Patients
Review-Dr-Perlyn
Home
Home
Home
Home
Conditions we Treat
Conditions we Treat
Conditions we Treat
Conditions we Treat
Victor Center Home
Victor Center Home
Meet the Victor Center Team
The Victor Center serves as a national resource to clinical and community organizations around the country. To that end, we:
- Advocate with professional societies, labs, insurers and healthcare providers to promote coverage of preconception genetic screening and counseling services.
- Develop turnkey resources to enable Jewish community engagement in outreach and education campaigns.
- Cultivate the development of “Model Cities” by assisting local collaborations between healthcare providers and Jewish community groups.
Meet the Victor Center Team
The Victor Center serves as a national resource to clinical and community organizations around the country. To that end, we:
- Advocate with professional societies, labs, insurers and healthcare providers to promote coverage of preconception genetic screening and counseling services.
- Develop turnkey resources to enable Jewish community engagement in outreach and education campaigns.
- Cultivate the development of “Model Cities” by assisting local collaborations between healthcare providers and Jewish community groups.
Our Curriculum
Doral UCC Spanish

El Centro de Cuidados Urgentes de Nicklaus Children’s en Doral abierto con prácticas de seguridad y salud expandidas

El Centro de Cuidados Urgentes en Doral esta abierto para servir a su familia con prácticas de seguridad aumentadas debido al Coronavirus (Conocido como COVID-19) para la protección de todos.
El horario del Centro de Cuidados Urgentes es de 11 a.m. a 10 p.m. de lunes a domingo.
El centro ofrece atención personalizada y rápida de lesiones menores y enfermedades de bebés, niños, adolescentes y adultos jóvenes menores de 21 años. Los servicios son proporcionados por expertos en atención pediátrica, dirigidos por médicos certificados por la junta.
Vea nuestro video de practicas de seguridad!
Prácticas de seguridad mejoradas
El centro ha implementado las siguientes medidas de seguridad:
- Visitantes limitados: Le pedimos que solo un adulto acompañe a un niño al centro de cuidados urgentes. Para niños con necesidades especiales, un adulto adicional puede acompañar al niño si es necesario.
- Mascarillas: Todos los adultos y niños mayores de dos años deben usar mascarillas al entrar a la instalación. Todo el personal también estará usando mascarillas y otros equipos de protección personal.
- Detección: A todos los pacientes, el personal y los visitantes se les tomará la temperatura antes de entrar al centro.
- Registro rápido: Adentro de nuestra instalación, tenemos un proceso de registro rápido. Los pacientes son trasladados a las habitaciones lo más rápido posible.
- Distanciamiento físico: Existen señales visuales para ayudar a todos a mantener una distancia de seis pies de los demás.
- Limpieza profunda: Cada sala de examen se limpia profundamente después de cada paciente. Además, las áreas comunes se limpian continuamente, con atención especial a los puntos de contacto, como los reposabrazos, las manijas de las puertas y más.
- Higiene de manos: Alentamos a las familias que usen las estaciones de desinfección de manos que proporcionamos después de tocar cualquier superficie.

Condiciones que tratamos
Algunas de las condiciones que tratamos en los Centros de Cuidados Urgentes de Nicklaus Children’s incluyen:
- Lesiones, heridas, cortes y golpes (incluyendo puntos de sutura)
- Picaduras de insectos, picaduras, erupciones y quemaduras menores
- Reacciones alérgicas menores
- Lesiones por tensión muscular
- Enfermedades respiratorias
- Dislocaciones y torceduras (incluyendo rayos X y entablillados)
- Dolores de oído e infecciones del oído
- Infecciones del tracto urinario
- Los virus, como la enfermedad de manos, pies y boca
- Vómitos, diarrea y deshidratación menor
El Centro de Cuidados Urgentes en Doral
3601 NW 107th Avenue
Doral, FL 33178
305-418-7717
All Locations
Who We Are
West Kendall UCC Spanish
El Centro de Cuidados Urgentes de Nicklaus Children’s en
West Kendall Está Abierto con Prácticas de Seguridad y Salud Expandidas

El Centro de Cuidados Urgentes en West Kendall está abierto para servir a su familia con prácticas de seguridad aumentadas debido al Coronavirus (COVID-19) para la protección de todos.
El horario del Centro de Cuidados Urgentes es de 11 a.m. a 10 p.m. de lunes a domingo.
El centro ofrece atención personalizada y rápida de lesiones menores y enfermedades de bebés, niños, adolescentes y adultos jóvenes menores de 21 años. Los servicios son proporcionados por expertos en atención pediátrica, dirigidos por médicos certificados por la junta.
¡Vea nuestro video de prácticas de seguridad!
Prácticas de Seguridad Aumentadas
El centro ha implementado las siguientes medidas de seguridad:
- Visitantes limitados: Le pedimos que solo un adulto acompañe a un niño al centro de cuidados urgentes. Para niños con necesidades especiales, un adulto adicional puede acompañar al niño si es necesario.
- Mascarillas: Todos los adultos y niños mayores de dos años deben usar mascarillas al entrar a la instalación. Todo el personal también estará usando mascarillas y otros equipos de protección personal.
- Detección: Todos los pacientes, empleados y visitantes recibirán una prueba de temperatura antes de entrar al centro.
- Registro rápido: Tenemos un proceso de registro rápido. Los pacientes son trasladados a las salas de examinación lo más rápido posible.
- Distanciamiento físico: Existen señales visuales para ayudar a todos a mantener seis pies de distancia de los demás.
- Limpieza profunda: Cada sala de examinación se limpia profundamente después de cada paciente. Además, las áreas comunes se limpian continuamente, con atención especial a los puntos de contacto, como los reposabrazos, las manijas de las puertas y más.
- Higiene de manos: Alentamos a las familias a que usen las estaciones de desinfección de manos que proporcionamos después de tocar cualquier superficie.

Condiciones que Tratamos
Algunas de las condiciones que tratamos en los Centros de Cuidados Urgentes de Nicklaus Children’s incluyen:
- Lesiones, heridas, cortes y golpes (incluyendo puntos de sutura)
- Picaduras de insectos, picaduras, erupciones y quemaduras menores
- Reacciones alérgicas menores
- Lesiones por tensión muscular
- Enfermedades respiratorias
- Dislocaciones y torceduras (incluyendo rayos X y entablillados)
- Dolores de oído e infecciones del oído
- Infecciones del tracto urinario
- Los virus, como la enfermedad de manos, pies y boca
- Vómitos, diarrea y deshidratación menor
El Centro de Cuidados Urgentes en West Kendall
13400 SW 120th Street, Suite 100
Miami, FL 33186
305-278-5912
Allergy & Immunology
Anesthesiology Home
NICU (Home)
Test Logon
Test Landing Page
If you are logged in, you will be able to see this page in your browser.
Donate
Videos
Videos
Test SVG
Test SVG 2
ENT Home
Ophthalmology Home
Miami Lakes UCC Spanish

El Centro de Cuidados Urgentes de Nicklaus Children’s en
Miami Lakes Está Abierto con Prácticas de Seguridad y Salud Expandidas

El Centro de Cuidados Urgentes en Miami Lakes está abierto para servir a su familia con prácticas de seguridad aumentadas debido al Coronavirus (COVID-19) para la protección de todos.
El horario del Centro de Cuidados Urgentes es de 11 a.m. a 10 p.m. de lunes a domingo.
El centro ofrece atención personalizada y rápida de lesiones menores y enfermedades de bebés, niños, adolescentes y adultos jóvenes menores de 21 años. Los servicios son proporcionados por expertos en atención pediátrica, dirigidos por médicos certificados por la junta.
¡Vea nuestro video de prácticas de seguridad!
Prácticas de Seguridad Aumentadas
El centro ha implementado las siguientes medidas de seguridad:
- Visitantes limitados: Le pedimos que solo un adulto acompañe a un niño al centro de cuidados urgentes. Para niños con necesidades especiales, un adulto adicional puede acompañar al niño si es necesario.
- Mascarillas: Todos los adultos y niños mayores de dos años deben usar mascarillas al entrar a la instalación. Todo el personal también estará usando mascarillas y otros equipos de protección personal.
- Detección: Todos los pacientes, empleados y visitantes recibirán una prueba de temperatura antes de entrar al centro.
- Registro rápido: Tenemos un proceso de registro rápido. Los pacientes son trasladados a las salas de examinación lo más rápido posible.
- Distanciamiento físico: Existen señales visuales para ayudar a todos a mantener seis pies de distancia de los demás.
- Limpieza profunda: Cada sala de examinación se limpia profundamente después de cada paciente. Además, las áreas comunes se limpian continuamente, con atención especial a los puntos de contacto, como los reposabrazos, las manijas de las puertas y más.
- Higiene de manos: Alentamos a las familias a que usen las estaciones de desinfección de manos que proporcionamos después de tocar cualquier superficie.

Condiciones que Tratamos
Pruebas de COVID-19 están disponibles cuando indicado clínicamente.
Algunas de las condiciones que tratamos en los Centros de Cuidados Urgentes de Nicklaus Children’s incluyen:
- Lesiones, heridas, cortes y golpes (incluyendo puntos de sutura)
- Picaduras de insectos, picaduras, erupciones y quemaduras menores
- Reacciones alérgicas menores
- Lesiones por tensión muscular
- Enfermedades respiratorias
- Dislocaciones y torceduras (incluyendo rayos X y entablillados)
- Dolores de oído e infecciones del oído
- Infecciones del tracto urinario
- Los virus, como la enfermedad de manos, pies y boca
- Vómitos, diarrea y deshidratación menor
El Centro de Cuidados Urgentes en Miami Lakes
15025 NW 77th Avenue
Miami Lakes, FL 33014
786-313-7821
Diamond Society
Coconut Creek Spanish Letter
Un mensaje importante sobre la oficina de Nicklaus Children’s localizada en Coconut Creek
Estimado Padre/Madre o Guardián:
Gracias por la oportunidad de brindarle atención a su hijo(a). Ha sido un privilegio atenderlo en la oficina de Nicklaus Children’s localizada en Coconut Creek (Nicklaus Children’s Coconut Creek Care Center). Es importante informarle que este centro de servicio cerrará pronto y dejará de atender pacientes a partir del 16 de octubre.
Esperamos continuar ofreciéndole atención médica a su hijo(a) en uno de nuestros centros regionales. Además, puede solicitar una consulta virtual de telemedicina (virtual Telehealth consultations), dependiendo de la naturaleza de la condición o el motivo de la visita.
Para obtener una lista de todas las especialidades pediátricas, por favor visite:
https://www.nicklauschildrens.org/servicios-medicos
Para obtener una lista de nuestros médicos y sus respectivas localidades de servicio, por favor visite:
https://www.nicklauschildrens.org/encuentre-un-doctor
Para citas en persona en cualquiera de nuestras localidades, por favor visite:
https://www.nicklauschildrens.org/ubicaciones
Su bienestar y el de su hijo(a) es nuestra mayor prioridad. Sepa que nuestro equipo está disponible para ayudarlo durante esta transición. Si tiene alguna pregunta o una cita programada en el Centro de Cuidados Coconut Creek después del 16 de octubre, llame al 888-624-APPT (2778) y un miembro de nuestro equipo lo ayudará con mucho gusto. También puede programar visitas en-persona o virtuales a través de: nicklauschildrens.org/Citas.
Para obtener una copia de sus registros médicos, llene un formulario de “Consentimiento para la divulgación de información” (Consent for Release of Information), disponible en nuestro sitio en la red en nicklauschildrens.org/RegistrosMedicos. También puede llamar a nuestra oficina de Gestión de Información de Salud (HIM, Health Information Management) al 1-800-432-6837, de lunes a viernes de 8:30 a.m. a 4:30 p.m.
Con nuestro sincero aprecio y mejores deseos,
Chad Perlyn, MD, PhD, FACS Maria Jayoussi, MBA, CPA, FHFMA
Presidente Interino Vicepresidenta, Gerente de Operaciones Ejecutivas y Directora Financiera
Nicklaus Children’s Pediatric Specialists (NCPS) Nicklaus Children’s Pediatric Specialists (NCPS)
Meet the Team
The treatment team will work closely with your child and the family to reach goals and assist with any needs throughout the hospital stay. There are many people with different disciplines involved in the care of your child and it is important to know their roles. Listed below is an explanation of the provider’s different roles.
NCPS Gastroenterology Virtual Care Spanish
Un mensaje importante de la Sección de Gastroenterología de
Nicklaus Children's Pediatric Specialists
Estimados padres y guardianes:
Gracias por elegir la Sección de Gastroenterología de Nicklaus Children’s Pediatric Specialists para el cuidado de su hijo(a). La salud y la seguridad de su hijo(a) y su familia siguen siendo nuestra principal prioridad.
Muchas familias han preguntado por las citas de telesalud, de modo que nos complace proveerles una lista de médicos de nuestro consultorio que pueden estar disponibles para consultas a través de nuestro programa Nicklaus Children’s Pediatric Virtual Care, según la naturaleza de la afección del paciente o el motivo de la visita.
A seguir, encontrará una lista de los médicos de la Sección de Gastroenterología de Nicklaus Children’s Hospital que actualmente ofrecen consultas virtuales:
Queremos informar a las familias que deseen vernos en una cita en el consultorio que estamos abiertos y listos para servirles con medidas de seguridad mejoradas en la era del COVID19, a fin de brindar una experiencia sin inconvenientes. Visiten nuestra página web exclusiva para conocer más detalles y obtener las últimas actualizaciones sobre las políticas para visitantes y los servicios hospitalarios.
Si tienen alguna pregunta o si desean programar una cita, llámenos al 888-624-APPT (2778) y un miembro de nuestro equipo, con gusto los atenderá. Las visitas presenciales y virtuales también pueden solicitarse en línea visitando: nicklauschildrens.org/Citas.
Esperamos poder seguir atendiéndolos.
Sinceramente,
Alisa Muñiz Crim, MD, MS
Jefa, Sección de Gastroenterología, Nicklaus Children’s Pediatric Specialists (NCPS)
Directora, División de Gastroenterología, Nicklaus Children’s Hospital
Directora, Centro de Enfermedad Inflamatoria del Intestino (IBD)
Appointment: Dental
Thank You
kayleen-ball-clinical-psychology
Appointment: BMT
Thank You
Conditions we Treat
Conditions we Treat
Videos
Videos
Nursing (Home)
Science of Nursing Home
Safety & Quality Innovations
At Nicklaus Children's Health System, we embrace innovation by deploying state-of-the-art technology throughout the hospital to improve patient safety and the patient experience, as well as to make our operational processes more efficient. Transforming pediatrics through innovation takes a village, and we are proud to work with leading technology companies, community programs, schools, policy-makers and other organizations for the betterment of our patients and their families.
GetWell:)Network
As a leading provider of interactive patient care solutions, GetWellNetwork was implemented in 2008. The GetWellNetwork is recognized by and works in conjunction with Child Health Corporation of America (CHCA) and the National Association of Children's Hospitals and Related Institutions (NACHRI). The bedside interactive computer/TV monitor allows the patient and family to be involved in their care.
The system provides educational materials through KidsHealth®, both standard and those prescribed by the nurse, interactive games, surveys for the families to complete, meal ordering, as well as "pop-ups" for patient-specific reminders. The system also allows the patient/family to access the Daisy Award to nominate outstanding nurses.
Foley
https://www.youtube.com/watch?v=1cu1DlW5zQo
Seca Scales
In 2018, Nicklaus Children's Health System became the first pediatric hospital using the Cerner electronic health record to implement electronic height and weight transmission directly from the patient scale to the medical record. Integration between the patient scales and the documentation system aligns with the organization's commitment to promote a culture of safety by further safeguarding weight-based dosing for medications. Eliminating manual input reduces the possibility of transcription related errors, enables consistent documentation, and promotes a more efficient workflow.
Camera Capture
Specialized photo application used to capture and share patient images securely. Images are electronically transmitted directly to the patient record.
Sherlock Catheter Insertion Technology
Prevents the need for second procedures/Xrays improving patient experience and quality of care
Johns/New Sepsis Alert
Early recognition of sepsis is crucial for the best patient outcome. The St. John Sepsis Surveillance Agent does just that, alerts the care team when to evaluate and treat sepsis at one of the earliest detectable points. The St. John sepsis alert draws from the best and most recent published evidence and uses cloud computing to screen and alert early on. Early detection and treatment can save lives.
Code Bear
In an effort to continue to promote a culture of safety and excellent patient care, Nicklaus Children's Hospital has created an innovative and proactive approach for the care and treatment of our autistic/behavioral patients. Code Bear comprises an outstanding healthcare professional team, with each member specializing in different aspects of caring for this patient population. Whether it's soothing techniques such as music therapy or medical intervention, they are there to ease their triggers and support the families during these challenging times.
Hand in Hand Together We Can.
PONS
The Pediatric Oncology Nutrition Screening (PONS) tool was developed at Nicklaus Children's Hospital as a collaboration between Nursing and Food and Nutrition departments. The PONS tool incorporates into our Electronic Medical Record (EMR) to screen pediatric oncology patients based on a risk assessment for malnutrition. This collaborative project has improved the process of identifying patients at risk for malnutrition, providing early nutritional interventions, and streamlined ordering dietary consults.
Telehealth
Nicklaus Children's Pediatric Virtual Care, our state-of-the-art telehealth platform, provides convenient access to care, bringing expert services and peace of mind to children and families. We are re-imagining the healthcare experience and innovating how we support families and children at the point of illness and throughout the continuum of health and wellness. The platform supports sophisticated videoconferencing and diagnostics via a range of web-enabled devices, allowing consultation with renowned specialty and subspecialty pediatricians, physicians, nurses, therapists, and other healthcare professionals.
The majority of our virtual care services are delivered through our proprietary telehealth application that is encrypted and HIPAA compliant. Our innovative virtual care services are provided in over 24 specialty areas and programs.
Subspecialty consultations account for 37% of volume, mental health 38%, rehabilitation services 17%, and primary care 5%. Telehealth services include direct services for assessment and intervention, consultations (provider to provider), second opinions, multi-disciplinary/health care team meetings, and education services.
School Health Services
This program offers preventive, primary care as well as mental health services to children in 75 schools in the Miami Dade County district.
Services are brought in person or via telehealth technology by nurses, nurse practitioners, mental health professionals, social workers, and a medical provider physician to more than 10,000 students in Miami-Dade County public schools.
At no cost, vaccines for children who do not have medical insurance or who are insured through Medicaid can obtain their childhood vaccines and the seasonal flu vaccine by calling the School Health Service appointment line (786-624-4757).
With an overarching aim to improve health outcomes for the student population, nurses ensure that children without a pediatrician receive anticipatory guidance, nutritional education, as well as chronic disease management, ensuring they are in environments conducive to thriving and learning.
Point of Care Testing
Nicklaus Children's Hospital nurses utilize iSTAT to perform point of care testing. The iSTAT is a portable machine not much bigger than a phone that is brought to the bedside for patient lab testing. With 0.1 cc of blood the nurse can run labs such as blood gas, lactic acid, electrolytes and the results are available within 120 seconds. The results are then downloaded into PEDS and accessible to the entire healthcare team.
Cerner Bridge™
Cerner Bridge™ Transfusion Administration uses bar-code scanning technology, wireless networks and clinical systems integration to improve patient safety. Utilizing positive patient identification, the solution records and collects information at the bedside and facilitates compliance with standards. The Cerner Bridge™ Transfusion solution provides up to six bar-code checks to ensure the right blood product is being administered to the correct patient, resulting in safer administration of blood products.
Education & Professional Development Innovations
Nicklaus Children's Health System offers Nursing Scholarship opportunities to support nurses in innovating and improving the nursing practice. Some of the programs offered include:
DART Simulation
In 2018, Nicklaus Children's Health System developed a hybrid simulation and mock code approach to nursing education and validation of cardiac specialty competencies using the DART Sim™ application in the CICU setting.
DART Sim is a mobile teaching software that can be installed onto a tablet or smartphone, with functions including cardio-respiratory monitoring, defibrillation and cardioversion, capnography, 12 Lead EKG and X-rays. It can be used with traditional CPR mannequins, making it portable and cost-effective. A simulation can be set up within the unit in minutes with an iPad, Apple TV, and a mannequin.
DART Simulations promote interdisciplinary and peer-to-peer interaction, which and aligns with Magnet culture.
Escape Room/Creative Education
To enhance knowledge and engagement through education, the clinical education team leads an annual Nursing Skills Fair. During the Fair, education is provided in different modalities, such as gaming techniques, verbal instruction, hands-on demonstration, case scenarios, and role-play. Recently, the clinical education team created an escape room method, where participants had to unlock codes by answering questions based on case scenarios to advance to the next session.
Elsevier's Nursing Skills
Nicklaus Children's Health System nurses have access to Elsevier's Nursing Skills. Elsevier's offers nurses and nurse educators the convenience of online access to evidence-based skills and procedures. Easily accessed from Nicklaus Children's Health System's portal, Elsevier's content provides nurses with resources and insight from leading nursing societies. Elsevier's is updated continuously to reflect the latest in evidence-based practice.
Pediatric Human Patient Simulator
Nicklaus Children's Hospital has a Pediatric Human Patient Simulator lab on-site, which provides training to nursing, clinical and medical staff. The lab is managed and run by nurses. Simulations include a variety of situations that nurses may face as they care for pediatric patients. In the interactive simulator lab, nurses and other healthcare professionals can enhance their clinical skills and become more comfortable responding to emergency situations - all in a non-threatening environment. Opportunities to utilize the lab begin during the orientation process.
Tests and Treatments
Tests and Treatments
RSVP

Holiday Celebration RSVP
Saturday, December 21st
Noon to 3 p.m.
Thank you
Treatments and Procedures
Treatments and Procedures
Amazon Wish List
Gift Card Wish List
Children's Experiences Fund
Review-Dental
Inpatient Unit Parent's Handbook
Programs and Services
Media Consent
Thank You
Diamond Ball Silent Auction
TraumaPathways
Virtual Diamond Ball - Live Auction
Virtual Diamond Ball - Social Media Toolkit
Specialty Request / Referral
Virtual Diamond Ball - Bid
Appointment: Heart Institute
Thank You
Thank you! Your request has been submitted.
A team member will contact you regarding your inquiry within the hours you have indicated.
Return to the Heart ProgramAppointment: Hemophilia
Thank You
Appointment: Sickle Cell
Thank You
Thank you! Your request has been submitted.
A team member will contact you regarding your inquiry within the hours you have indicated.
Return to the Sickle Cell ProgramPatient of the Month
Appointment: Survive & Thrive
Thank You
Survivorship Program News
Survivorship Program News
Patient Stories
Patient Stories
Patient Stories
Patient Stories
Gabriella's Gift
Appointment: Leukemia
Thank You
Appointment: Neuro-Oncology
Uncomplicated Community Acquired Pneumonia
Pathways
Leukemia Program Home
Leukemia Program Home
Conditions we Treat
Conditions we Treat
Patient Stories
Patient Stories
Cancer & Blood Disorders Center
Cancer & Blood Disorders Center
Thank You
Speech Development Milestones
If you are concerned about your child’s language development and if they are achieving their developmental milestones age appropriately…. Don’t delay!! Help is available to you from our highly skilled rehabilitative team of speech-language pathologists at Nicklaus Children’s Hospital.
Early intervention for children birth-3 years old is key to future social and academic success. However, in order to provide your child with the best help possible, it is important that you are able to recognize red flags of language delay, Speech delay, Speech disorders, Autism, and or Phonological errors.
Please see the following list of ASHA’s developmental milestones for children from birth to three years old, to determine if you need to request a referral from your child’s pediatrician.

Speech milestones in babies, what should my baby be able to do?
Hearing and Understanding Skills
|
Talking Skills
|
Birth to 3 Months
- Startles at loud sounds.
- Quiets or smiles when you talk.
- Seems to recognize your voice. Quiets if crying.
|
Birth to 3 Months
- Makes cooing sounds.
- Cries change for different needs.
- Smiles at people.
|
4 to 6 Months
- Moves her eyes in the direction of sounds.
- Responds to changes in your tone of voice.
- Notices toys that make sounds.
- Pays attention to music.
|
4 to 6 Months
- Coos and babbles when playing alone or with you.
- Makes speech-like babbling sounds, like “pa, ba, and mi.”
- Giggles and laughs.
- Makes sounds when happy or upset
|
7 Months to 1 Year
- Turns and looks in the direction of sounds.
- Looks when you point.
- Turns when you call her name.
- Understands words for common items and people—words like cup, truck, juice, and daddy.
- Starts to respond to simple words and phrases, like “No,” “Come here,” and “Want more?”
- Plays games with you, like peek-a-boo and pat-a-cake.
- Listens to songs and stories for a short time.
|
7 Months to 1 Year
- Babbles long strings of sounds, such as “mimi” “up up” and “babababa.”
- Uses sounds and gestures to get and keep attention.
- Points to objects and shows them to others.
- Uses gestures like waving bye, reaching for “up,” and shaking his head no.
- Imitates different speech sounds.
- Says one or two words, such as “hi” “dog” “dada” “mama” or “uh-oh.” This will happen around his first birthday, but sounds may not be clear.
|

Speech Milestones in Children One to Two Years
Children develop at their own rate. Your child might not have all skills until the end of the age range.
Hearing and Understanding Skills
|
Talking Skills
|
- Points to a few body parts when you ask.
- Follows 1-part directions, like "Roll the ball" or "Kiss the baby."
- Responds to simple questions, like “Who’s that?” or “Where’s your shoe?”
- Listens to simple stories, songs, and rhymes.
- Points to pictures in a book when you name them.
|
- Uses a lot of new words.
- Uses p, b, m, h, and w in words.
- Starts to name pictures in books.
- Asks questions, like “What's that?”, “Who’s that?”, and “Where’s kitty?”
- Puts 2 words together, like "more apple," "no bed," and "mommy book."
|

Speech Milestones in Children Two to Three Years
Children develop at their own rate. Your child might not have all skills until the end of the age range.
Hearing and Understanding Skills
|
Talking Skills
|
- Understands opposites, like go–stop, big–little, and up–down.
- Follows 2-part directions, like "Get the spoon and put it on the table."
- Understands new words quickly.
|
- Has a word for almost everything.
- Talks about things that are not in the room.
- Uses k, g, f, t, d, and n in words.
- Uses words like in, on, and under.
- Uses two- or three- words to talk about and ask for things.
- People who know your child can understand him.
- Asks “Why?”
- Puts 3 words together to talk about things. May repeat some words and sounds
|
Source: The American Speech-Language-Hearing Association (ASHA).
Complicated Community Acquired Pneumonia
Croup
Jackie Gonzalez Recognition
Thank you for wishing Jackie Gonzalez a happy retirement. There are two ways to share a special personalized message with her:
- Upload a picture or video by clicking here
- Fill out the form below to send her a message
If you’re submitting a video, please be sure to adhere to these guidelines:
- Be sure to hold your phone or tablet in landscape mode
- Avoid using digital zoom or filters
- Beware of background noises
- Remember to check the lighting
Thank You
Thank You
Intentional Overdose
Review-Dr-Cabbad
Review-Dr-Berger
Review-Dr-Tirado
Review-Dr-Ho
Review-Dr-Ramchandran
Review-Dr-George
Review-Dr-Errico
Review-Dr-Spurdle
Review-Dr-Schreiber
Review-Dr-Schoenleber
Review-Dr-Payares-Lizano
Review-Dr-Horowitz
Review-Dr-Baitner
Patient Resources
Patient Resources
Grateful Patients
NYCA Kickoff
For Nurses (Home)
Example of Complicated Community Acquired Pneumonia (parapneumonic effusion)
Example of Complicated Community Acquired Pneumonia (parapneumonic effusion)
Studies and Tests
Studies and Tests
Studies and Tests
Trauma Burn Transfer Criteria
Trauma Burn Transfer Criteria
Review-Dr-Fuchs
Resources for Teachers
School Health Home
Lilly Pulitzer/ Honda Classic Collab
CMNH
BRUE
COVID-19 Testing and Treatment
Medical Staff Annual Education Attestation
Flash Fundraiser
Consent Request
IBD Center Home
IBD Center Home
Review-Dr-Hariharan
Review-Dr-Carrillo-Iregui
Review-Dr-Diaz
Review-Dr-Gonzalez-Mendoza
Review-Dr-Pagan Banchs
Review-Dr-Seiler
Review-Dr-Tarkoff
Review-Dr- Caicedo Oquendo
Review-Dr-Felipez
Review-Dr-Mestre
Review-Dr-Llopiz-Martin
Review-Dr-Firestone-Baum
Review-Dr-Hornig
Review-Dr-Liu
Review-Dr-Kana
Review-Dr-Hay
Review-Dr-Muniz-Crim
Review-Dr-Della-Volpe
Review-Dr-Welch
Review-Dr-Gamboa
Review-Dr-Prieto
Review-Dr-Santana-Acosta
Review-Dr-Wang
Review-Dr-Hanfland
Abuse Reporting Algorithm
Acute Head Trauma
Burn Care Guidelines for UCCs
Cervical Spine Clearance
Skull Fracture
VTE Risk Assessment Algorithm
Trauma Clinical Pathways
Review-Dr-Price
For Medical Professionals Home
Review-Dr-Price
Review-Dr-Escalon
Review-Dr-Resnick
Review-Dr-Pefkarou
Review-Dr-Cotilla
Review-Dr-Mishal
Review-Dr-Schleifer
Review-Dr-Calisto
Review-Dr-Portela
Review-Dr-Silverberg
Review-Dr-Guerrero
Review-Dr-Kozakowski
Review-Dr-Koyfman
Review-Dr-Aftab
Review-Dr-Sanchez-Vegas
Review-Dr-Hagler
Review-Dr-Paredes
Review-Dr-Loredo
Review-Dr-Gray
Review-Dr-Comkornruecha
Review-Dr-Labbie
Review-Dr-Gomara
Review-Dr-Bauer
Review-Dr-Gonzalez-Vallina
Review-Dr-Epstein
Review-Dr-Muinos
Review-Dr-Rossi
Review-Dr-Portela
Review-Dr-DeCardenas
Review-Dr-Niazi
Review-Dr-Soler
Review-Dr-Edrees
Review-Dr-Malvezzi
Review-Dr-Alkhoury
Review-Dr-Gutierrez
Review-Dr-Muniz
Review-Dr-Perez
Review-Dr-Galan
Review-Dr-Fajardo
Review-Dr-Lolo
Review-Dr-Silva
Review-Dr-Jayakar
Review-Dr-McCrea
Review-Dr-Rodriguez
Review-Dr-Patel
Review-Dr-Tuchman
Review-Dr-Fernandez
Review-Dr-Laufer
Review-Dr-Segeren
Review-Dr-Naqvi
Review-Dr-Hannan
Review-Dr-Deray
Review-Dr-Franco
Review-Dr-Wolfe
Review-Dr-Warman
Review-Dr-Castellan
Review-Dr-Arboleda
Review-Dr-Duchowny
Review-Dr-Bolivar
Review-Dr-Katz
Review-Dr-Ramirez-Seijas
Review-Dr-Riefkohl
Review-Dr-Hernandez
Review-Dr-Orjuela
Review-Dr-Parul-Jayakar
Review-Dr-Padilla
Review-Dr-Corrales-Reyes
Review-Dr-Reeves-Garcia
Review-Dr-Milla
Review-Dr-Carreno
Review-Dr-Angulo
Review-Dr-Ragheb
Review-Dr-Rosa-Olivares
Review-Dr-Maher
Review-Dr-Cardenas
Review-Dr-Nwobi
Review-Dr-Bejar
Review-Dr-Dussan
Review-Dr-Cruz
Review-Dr-Diaz-Barbosa
Review-Dr-De-la-Vega
Review-Dr-Tarshish
Review-Dr-Milesi-Halle
Review-Dr-Aponte-Rodriguez
Review-Dr-Godder
Review-Dr-Fader
Review-Dr-Alrazzak
Review-Dr-Abdella
Review-Dr-Monduy
Review-Dr-Gosalbez
Review-Dr-Sterba-Rakovchik
Review-Dr-Mendez-Soto
Review-Dr-Calderon
Review-Dr-Martinez-Fernandez
Review-Dr-Kanter
Review-Dr-Baysa
Review-Dr-Nao-Sasaki
Review-Dr-Jun-Sasaki
Review-Dr-Christin
daniel-duarte-caceres-cardiology
Appointment: Colorectal Center
Thank You
Thank you! Your request has been submitted.
A team member will contact you regarding your inquiry within the hours you have indicated.
Return to the Colorectal ProgramTrauma Alert Criteria
Appointment: Psychiatry
Due to the higher than usual volume of appointment requests, at this time we are unable to schedule any a new appointments. If you need immediate services, please contact your insurance company for additional providers.
If your request can wait, we encourage you to call back during the first days of the next month as some appointments do become available at that time.
Appointment: Sarcoma & Solid Tumor
Box of Love - Polos
Welcome to Florida RSVP
himanshu-adlakha-cardiology
Underwear Fund
jackeline-sanchez-clinical-psychology
Treatments
Treatments
Knots of Hope
Bradley
Meet the IBD Center Team
The IBD Center at Nicklaus Children’s Hospital brings together a comprehensive team of experts to support your child and family. The entire team takes part in clinical management to allow your child to benefit from multispecialty collaboration and consultation.
Meet the IBD Center Team
The IBD Center at Nicklaus Children’s Hospital brings together a comprehensive team of experts to support your child and family. The entire team takes part in clinical management to allow your child to benefit from multispecialty collaboration and consultation.
Employee Gift
Employee Gift - Welcome NCHS
Patient Assistance
Concussion Clinic Home
Concussion Clinic Home
Tests and Treatments
HappySong
Connect4
Thank You
Children's Champion
Carolyn Domina's Retirement
Get Application FAQ

What is the Get App?
The GET App allows our employees, using their mobile device, to order food from the Golden Cub Café and the Miracles Café for pickup.
How do I get the mobile app?
You can download the Get App from the Google Play Store or the Apple App Store.
Can I order on the web, or just on the mobile app?
What if I have issues registering?
If you have issues registering, please verify your Last Name is typed exactly as it shows in PeopleSoft and that your Employee ID is entered with the right amount of leading 0’s. If you still experience an issue, please open an IT "Something isn't working" ticket at https://nchs.service-now.com/sp?id=information_technology
Do you have to be an employee to order food?
Yes. You will need to be an employee with payroll deduction enabled. If you do not have payroll deduction enabled, please visit PeopleSoft Self Service located on the Intranet to activate Employee Payroll Deduction. In the future, we plan to open ordering to everyone.
What cafes/locations are offering this service? Will they have the same Hours of Operation?
Currently only the Golden Cub Café and Miracles Café will offer items on the GET Mobile App. They will also have reduced hours on the mobile app only.
Golden Cub Café will open for lunch orders only.
Monday-Friday 11:30 a.m. - 2:30 p.m.
Miracles café will be open all week.
Monday-Friday 6 a.m. - 10 p.m. on the mobile app.
How can I order food items? How does this work?
The GET App works like various other food ordering applications. You will need to download the Get Mobile app at https://get.cbord.com/nicklauschildrens/ and register. You must also have payroll deduction active to place orders. We are currently accepting only payroll deduction as a payment option at this time.
Where do I pick up my order?
Golden Cub Café order will be available for pickup in the dining room. Miracles Café orders will be available at the pickup window.
Is delivery available?
No. We are only offering pickup at the moment. We are looking into this possibility for the future.
Are the hours of operation the same?
The hours of operation on the mobile app are slightly different.
Golden Cub Café will open for lunch orders only.
Monday-Friday 11:30 a.m.-2 p.m. The Golden Cub Café in person hours remain the same.
Miracles Café will be open Sunday-Saturday from 6 a.m.-10 p.m
How do I know my order is available for pickup?
You will receive an email confirmation with the time you selected for pickup. If you selected ASAP then your order will be ready within 15 minutes. There will not be an additional email or notification showing when the order is available for pickup.
What if I cannot pick up my order on time?
We will hold your order for 15 min after your Pick-up Time, then it will be discarded for Food Safety issues. No refund will be issue if you did not pick up your order.
Are all items available from the Golden Cub Café?
No. To provide the best customer experience, not all menu items are available. At this time, only Grab n Go and the Buffet Line will be available from the Golden Cub Café.
Are the prices different on the mobile app vs. in person at the Golden Cub Café or Miracles Cafe?
No. The prices you see on the GET Mobile App will be the same as shown in both Golden Cub Café and Miracles Café. Prices for Golden Cub Café will reflect the employee discount.
What if I need to change my order? Or I ordered the incorrect item?
Changes on submitted orders are not allowed. You can cancel your order if it is not within 20 minutes of your pickup time. If you placed an order as “ASAP,” you will not be able to cancel the order.
Can I cancel my order?
You can cancel your order if it is not within 20 minutes of your pickup time. If you placed an order as “ASAP,” you will not be able to cancel the order.
Who do I contact if there is a mistake with my order or I have any questions?
Email us at Dietary.Suggestions@NicklausHealth.org
NCH Gift Shop
Can I order items from the Gift Shop?
Not at this time. In the future you will be able to, but this location is not yet active.
Payments / Refunds / Fees
What are the payment methods? Can I use payroll deduction? Can I use my credit card?
Employee Payroll Deduction is the only payment method currently accepted. Credit cards will be available in the future.
Can I use my meal plan stipend to order food?
No. Only Employee Payroll Deduction is accepted. Stipends will not be accepted on the mobile app.
Is there any additional cost?
There will be a Service Charge of $1.50 for Golden Cub Café; prices will be shown with employee discounts.
What is your Refund Policy?
If there is something wrong with your order, a refund can be done. Please come to the location where your order was placed and one of our cashiers will assist you.
Match Game
Who is our furry friend?

Congratulations! You have found Alfie.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Apollo.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Blue.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Clooney.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Copper.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Odin.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Pebbles.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Prada.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Rusty.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Walle.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Walter.
Keep Matching!
Who is our furry friend?

Congratulations! You have found Zeus.
Keep Matching!
Scholarship Day 2019
11th Annual Nicklaus Children’s Hospital Scholarship Day
June 14, 2019
The Nicklaus Children's Hospital Scholarship Day is a yearly event that features the scholarly activities of our pediatric residents, dental residents, pediatric subspecialty fellows, and nursing colleagues. The event is organized by the Nicklaus Children’s Research Institute and the Departments of Medical Education and Nursing. Research projects (original research and case reports) and QI projects are submitted, peer-reviewed, rated, and displayed as poster presentations. Winning abstracts are presented as podium presentations. Below, you will find samples of the research endeavors Nicklaus Children's Hospital GME trainees and nurses are conducting. Read more about the abstracts that were submitted by clicking on one of the tabs.
Underlined Author - Denotes a “Trainee”
Bold Print - Denotes a Winning Peer-Reviewed Abstract
* - Denotes a Presenting Author
§ - Denotes Late Breaking / Non-Rated Abstract
Lozano Chinga M*, Villacis Nunez DS, Thompson J, Comkornruecha M, Cunill B. “Assessment of HIV screening in adolescent patients: A QI project”.
Chang Y*, Cardenas-Morales M, Caicedo Oquendo L, Calderon JG, Blouin WR, Hernandez-Trujillo VP. “Pill endoscopy as a diagnostic tool for an abdominal exacerbation in a pediatric patient with Hereditary Angioedema: a case report”.
Schissler KA*, Ortega C, Hernandez-Trujillo VP, and Calderon J. “A New Diagnosis of CVID in a Pediatric Patient Presenting with Streptococcus Pneumoniae Meningitis”
Cardenas-Morales M*, Ortega C, Martinez P, Hernandez-Trujillo V, Arbach L, Calderon J. “ XLA Presenting as HHV-6 Meningitis and Pseudomonas Meningitis/Bacteremia in a Patient Without History of Recurrent Infections”.
Cardenas-Morales M*, Chang Y, Blouin W, Hernandez-Trujillo VP. “Hereditary Angioedema Precipitated by Constipation Secondary to Stimulant Medication Use”.
Seshadri P*, Habiballah S, Ortega C, Verhage TJ, Lozano Chinga M, Hernandez Trujillo V. “Increasing Discussion on Early Peanut Introduction- A Quality Improvement Project”.
Halickman R*, Gruber JB, Zonana-Amkie R, Rhodes JF. “Long-Term Management of Native Coarctation of the Aorta after Endovascular Stent Implantation in Children with Ongoing Aortic Growth”.
Alarcon G*, Mehta KK, Burke R, Rossi A. “Unusual Single Ventricle Palliation”
Alqahtani M*, Mehta K, Santana-Acosta D. “Hypolastic Left Heart Syndrome with Esophageal Atresia and Tracheoesophageal Fistula”.
Girgis ST*, Patel B. “Heterotaxy with Single Ventricle Physiology with Liver Failure from Alagille Syndrome”.
Halickman R*, Mehta K, Patel M. “Intestinal Obstruction and DIC in the setting of Mechanical Valve”.
Pasternack D*, Sasaki J, Katz J. “The hidden danger of pleural effusions in the post-operative Fontan Patient”.
Torres-Burgos I* & Sasaki, J. “Beating the Odds: Complications after Arterial Switch Operation”.
Zonana Amkie R*, Mehta K; Santana-Acosta D. “Successful Delayed Single Ventricle Palliations Following Natural Calamity.”
Kolli S*, Seshadri P, Lugo C, Totapally B. “Seasonal and Regional Variations in the Prevalence of Viral Encephalitis in Hospitalized Children in the United States”.
Torres D*, Prieto P, Calisto J, Alkhoury F, Sendi P, Martinez P, Totapally B. “Epidemiology and Outcomes of Hospitalized Children with Cholecystectomy”.
Aliotti M*, and Arevalo O. “Capacity of Federally Qualified Health Centers in Florida”.
Purcell K*, Hsu KL, Huang TY, Drukteinis L. “Parental Knowledge and Acceptance of Silver Diamine Fluoride Application”.
Sears L*, and Arevalo O. “Medicaid Perspectives of Florida Dentists”.
Miranda P*, Freitas V. “Oral Morbidity and Service-Mix in a Mobile Dental Unit”.
Roman C*, Drukteinis L. “Analysis of Publication Trends in Three High Impact Pediatric Dentistry Journals”.
Cohen N*, Schissler K, Jeter J, Stathas A, Lozano J, Lowe D. “Unscheduled return visits decrease in pediatric patients post tonsillectomy and adenoidectomy with changes in opioid prescription patterns due to FDA black box warning”.
Cohen N*, Jeter J, Schissler K, Ovando D, Chiriboga L, Maniaci V, Lozano J, and Peña B. “Poor Perception and Knowledge of Electronic Cigarettes Amongst Adolescents and their Parents”.
Reynolds-Herbst T* and Linares MYR. “Nonfreezing Cold Injury Precipitating Bullous Cellulitis: An Important Consideration in the Age of Home Remedies”
Cohen N*; Sedor A; Lozano-Chinga M; Hassor S; Gereige R, Mestre M, Etinger V; Pena B; Denaro A; Reyes M. “Reduction of Chest X-ray Utilization in Uncomplicated Bronchiolitis and Asthma patients presenting to a Pediatric Emergency Department: A Quality Improvement Project”.
Vasquez RA*; Lozano JM; Denaro MA; Maniaci V; Linares M; Lowe DA. “A Zone System is Associated with Decreased Length of Stay in a Pediatric Emergency Department”.
Schissler K*, Diaz N, Sarmiento A, Abdella H, and Diaz A. “Acute Pancreatitis and Diabetic Ketoacidosis in an 8-Year-Old Following Induction Therapy for Pre-B Acute Lymphocytic Leukemia”.
Diaz J*, Cagil Y, Kolli S, Frade-Garcia A, Wang W, Taylor T, Felipez LM, and Muñiz Crim A. “Therapeutic Drug Monitoring of Infliximab During Induction: A Single Center Experience” .
Sierra D, Wood M, Iskowitz S*, Taylor T, Felipez L, Muniz Crim A. “Varicella Immunity in Pediatric IBD: A Review of the South Florida Population”.
Cagil Y* and Caicedo Oquendo LF. “Young Adult with a Rare Cause of Progressive Dysphagia”.
Diaz J*, Frade Garcia A, Pelaez L, Hernandez E, Arboleda R. “Wilson disease and GLUT1 deficiency syndrome – a case report”.
Iskowitz S*, Prieto P, Felipez L, Muniz Crim A. “Disseminated Histoplasmosis During Induction of Adalimumab”.
Iskowitz S*, Prieto P, Felipez L, Muniz Crim A. “Atypical HSP Presentation in an Adult Patient”.
Iskowitz S*, Prieto P, Felipez L, Muniz Crim A. “Adalimumab-Induced Peripheral Neuropathy”.
Liberti A*, Denny V, Reeves-Garcia J. “Mycobacterium and Crohn's Disease: Cause or Coincidence?”
Prieto P*, lskowitz S, Huang A, Pelaez L, Sanchez-Vega C, Hernandez E. “A RARE INFECTIOUS COMPLICATION IN A PATIENT WITH CROHN'S DISEASE AFTER THE USE OF INFLIXIMAB”
Prieto P*, lskowitz S, Huang A, Brathwaite C, Cervantes L, Muniz-Crim A, Felipez L. “CHALLENGING DIAGNOSIS OF A PEDIATRIC PATIENT WITH CROHN'S DISEASE WHO PRESENTED WITH RESPIRATORY SYMPTOMS AFTER TREATMENT WITH VEDOLIZUMAB”.
Prieto P*, Lawand S, Caicedo L. “IBD SGI 7 SERO (+) MARKERS PREDICTING FISTULIZING CROHN'S DISEASE ON ANOTHERWISE HEALTHY PATIENT WITH ULCERATIVE COLITIS”.
Alegria A*, Schissler K*, Hay A, Restrepo R, Laufer P. “Recurrent Bone Pain in a 12-year-old Girl with Ulcerative Colitis”.
Cagil Y*, Diaz J*, Gonzalez E*, and Muniz Crim A. “Improving Influenza Vaccination in IBD Patients Being Treated with Anti-TNF Agents”.
Mendoza M*, Trabal A, Glithero K, Riefkohl G. “Gastric Trichobezoar: An Uncommon Cause of Abdominal Pain”.
Bardi G*, Burkett J*, Lugo C*, Sedor A*, Yasher K*, Riefkohl G. “Straightening Out Scoliosis”.
Zonana Amkie R*, Torres-Burgos I, AlQahtani M, Girgis S, Lawand S. “Identifying Pediatric Hypertension in the Clinic Setting: A single Center Experience”.
Frade Garcia A*, Smith H, Sanchez M, Payson A, Llanos A, Jayakar P, Totapally B, Diaz-Barbosa M. “Rapid Whole Genome Sequencing for Genetic Disease Diagnosis in Acutely Ill Infants”.
Diaz N*, Lozano Chinga MM, Maher OM, Godder K, Galvez J. “Endothelin-1 inhibition in a child with transplant-associated thrombotic microangiopathy following autologous stem cell rescue for high-risk neuroblastoma – possible therapeutic role”.
Kashif R*, Payson A, Del Valle Penella A, Liset P, Abdella H. “Clinical Description and Medical Management of Necrotizing Lymphadenitis in a Sickle Cell Child”.
Kashif R*, O’Connor Z, Del Valle Penella A, Lozano-Chinga M, Maher O, Galvez Silva J, DeAngulo G, Brathwait C. “Primary Myelofibrosis with AML Transformation in a Child: Rare Presentation and Poor Response Therapy”.
Lozano Chinga MM*, Rodriguez A, Lopez Garcia M, Pelaez L, Maher OM, Galvez J. “NOVEL MUTATION OF ALAS2 IN CONGENITAL SIDEROBLASTIC ANEMIA NON-RESPONSIVE TO PYRIDOXINE - NEXT BMT”.
Lozano Chinga MM*, Diaz Forero N, Del Valle Penella A, Kashif R, Galvez Silva J, Khatib Z, Maher OM. “SINUSOIDAL OBSTRUCTION SYNDROME ON HEAD START IV REGIMEN IN YOUNG CHILDREN WITH EMBRYONAL TUMORS”
O’Connor Z*; Kashif R; Del Valle A; Khatib Z; Niazi T; Maher OM. “A Case of Pineal Germ Cell Tumor Presenting With Intracranial Bleeding Following an Endoscopic Third Ventriculostomy”.
Del Valle Penella A*, O’Connor Z, Kashif R, Ragheb J, Hall MD, Khatib Z, Maher OM. “Metastatic high grade neuroepithelial tumor in a child with PLAG1 amplification”.
Sarmiento A*, Del Valle Penella A, Montarroyos SS, Sanchez-Vegas C. “Two Cases of Motor Regression: The Diagnosis we Keep Missing”.
Trabal A*, Cohen N, Laufer M, Rakovchik E. “Parvovirus-Induced Acute Adrenal Crisis in an Immunocompetent 13 year-old Male”.
Alexander D*, Higley R*, Kolli S*, Behnam-Terneus M. “Albuterol HFA Training”.
Mehta KK, Wein C, Hallickman R*, Duarte Caceres D. “Improving Resident Comfort with Electrocardiogram Interpretation”.
Jeter J, Ramos A*, Tano S, Cunill B. “Improvement in resident exposure to procedures”. §
Pennicott K*, Cagil Y, Behnam-Terneus M, Maggioni A. “Trainee Driven Development & Implementation of a Global Health Curriculum at a Large Pediatric Residency Program”.
Llanos A, Diaz-Barbosa M, Sanchez Rosado M, Frade Garcia A*, Smith H, Calderon R, Fistel H, Tena F, Laufer P. “Conducting a Gap Analysis to Prioritize Antibiotics Stewardship Interventions in a Freestanding Children’s Hospital Level IV NICU”.
Sanchez Rosado MO*, Frade Garcia A, Aftab S. “Designing a Quality Improvement Program to Improve Rates of Kangaroo Care in a level IV NICU setting”.
Llanos A, Diaz-Barbosa M, Sanchez M, Frade A*, Miranda F, Smith H, Hussein S, Perez J, Calderon R, Fistel H, Tena F, Laufer P. "Evaluating the Effect of Participating in VON iNICQ Choosing Antibiotic Wiselyin Reducing AntibioticUse in a Free Standing Children's Hospital".
Sanchez Rosado M*, Frade Garcia A, Bukhari A, Diaz-Barbosa M, Celleri V, Llanos A. “Improving Vaccination Rates in Infants in a Freestanding Children’s Hospital NICU: A Resident QI”.
Kolli S*, Halickman R, Seshadri P, Christin N. “A Case of Thrombotic Microangiopathy in a Jehovah’s Witness”.
Jones A*. “Efficacy of the WISER Resilience Training Program in Combating Burnout”
Jones A & Lima-Kellar N*. “Promoting Patient & Family Engagement in the Reduction of Preventable Harm Events Through the Use of Bedside Education Tools”.
Klareich J*, Nieves Roldan I*. “Seize the Day: A Standardized Educational Pathway to Decrease Readmission Rates”.
Klareich J*, Nieves Roldan I*. “Reassess is Best in 60 Minutes or Less!”.
Duva M*; Coakley S. “Ace the Space to Improve Care in Pediatric Dialysis Patients”.
Ferreyra G*, Frank I. “Integrating Lactation Support to Improve Provision of Mother’s Own Milk in a Neonatal Intensive Care Unit”.
Ramchandran S*, Shufflebarger H. “Late arising infection in adolescent spinal deformity: One time exchange from stainless steel to titanium implants”.
Ramchandran S*, Minhas A, Shufflebarger H, George S. “Clinical and radiographic outcomes following spinal deformity correction in adolescent patients refusing blood transfusion”.
Hassor S, Payson A*, Franyie-Ladd B. “Correlation of Meningitis/Encephalitis PCR Panel Results with CSF Cell Counts: A Chart Review”.
Iskowitz S*, Eugenia Carter Febres M, Pulido A. “An Infection That Makes You Feel Like BOOP”.
Liberti A*, Gonzalez C. “Twinkle twinkle starry eyes: How I wonder what you are!”
Lopez Garcia ME*, Murphy K, Clemente M. “A case of missing pulse”.
Lozano Chinga MM*, Gonzalez C. “IT’S NOT WHAT YOU THINK”
Pasternack D*, Runyon J, Pulido A. “When lymph nodes strike back”.
Del Valle Penella A*, Sarmiento A, Pulido A. “Don´t be fooled by the great imitator: A 3-month-old Female with multiple fractures”
Del Valle Penella A*, Sarmiento A, Payson A, Selem S. “When there is more to reflux than meets the eye”.
Sarmiento A*, Del Valle Penella A, Franyie Ladd B. “A Diagnosis Hard To Swallow: A Case Report”.
Alegria A*, Meneses Paz JC. “A 14-year-old Autistic Girl with Back Pain and Gingival Hyperplasia.”
Pennicott K*, Alegria A, Payson A, Mestre M. “Meds to Beds”.
Habiballah S*, Rizkalla M, Alkhoury F. “Acute small bowel obstruction in a virgin abdomen of a 3-week-old girl”.
Iskowitz S*, Marin F. “Intussusception Presenting with Hemoptysis”.
Oweisi S*, Lee H, Roy SY, Blyumin G, Totapally B, Balakumar N, Gupta A, Taylor T. “Evaluation of peri-extubation propofol washout in critically ill children undergoing prolonged mechanical ventilation”.
Vuong M*, Lee H, Roy S, Rodriguez Y, Sotto I, Gruber J. “Evaluation of advancing chemotherapy administration times and the incidence of hemorrhagic cystitis”.
Lozano Chinga M, Villacis Nunez DS*, Thompson J, Hay A, Sterba Y, Cunill B. “Implementation of a Toolkit for Transition Readiness Assessment in Patients with JIA: A QI project”.
Scholarship Week 2021
12th Annual Virtual Scholarship Week
June 1 through June 4, 2021
Due to COVID restrictions, this year's Scholarship event will take place virtually. The Nicklaus Children's Hospital Scholarship Week is part of a yearly event that features the scholarly activities of our pediatric residents, dental residents, pediatric subspecialty fellows, and nursing colleagues.
Below is a list of this year's submissions, click each title to expand the list of abstracts by category. You may download a summary of the abstracts submitted or a detailed list of abstracts by clicking the download buttons below.
Download Abstract List by Specialty | Download Complete Abstract List | Download Schedule At a Glance
Underlined Author - Denotes a “Trainee”
Bold Print & ** - Denotes a Winning Peer-Reviewed Abstract
* - Denotes a Presenting Author
§ - Denotes Late Breaking / Non-Rated Abstract
Abstract #68: (RES-008-QI)
Rezk M; Thompson J*; Comkornruecha M; and Gray S. “Improving Screening for Child Abuse in Adolescent Medicine Clinic”.
Abstract #17: (FEL-016-OR)**
Urschel D*; Hernandez-Trujillo VP; Calderon J. “Panel of Unintended Consequences”.
Abstract #27: (RES-007-CR)
Fallatah E*; Chang Y; Calderon JG; Hernandez-Trujillo VP. “DiGeorge Syndrome and COVID-19 in Two Pediatric Patients”.
Abstract #34: (RES-014-CR)
Graneiro A*; Chang Y; Hernandez Trujillo V. “Chronic chough in a patient with CVID and GLILD”.
Abstract #57: (FEL-037-CR)
Chang Y*; Lairet S; Calderon JG; Hernandez-Trujillo VP. “A Case of Drug Allergy –Or is it?”.
Abstract #58: (FEL-038-CR)
Chang Y*; Urschel D; Hernandez-Trujillo VP; Calderon JG. “A Case of Mild COVID-19 in a Teenager with Common Variable Immunodeficiency and Granulomatous Lymphocytic Interstitial Lung Disease on Replacement Immunoglobulin and Infliximab”.
Abstract #59: (FEL-039-CR)
Urschel D*; Hernandez-Trujillo VP; Calderon J. “Medication Induced Agranulocytosis”.
Abstract #60: (FEL-040-CR)
Urschel D*; Cardenas M; Hernandez-Trujillo VP. “Chronic Variable Immunodeficiency and Coronavirus”.
Abstract #62: (RES-002-QI)
Graneiro A; Fallatah E; Mandel G*; Hernandez-Trujillo VP. “Increasing Awareness of the Montelukast Black Box Warning”.
Abstract #63: (RES-003-QI)
Urschel D*; Mendoza M*; Lairet S*; Riefkhol G; Llopiz F; Milla M; Hernandez-Trujillo V. “Improving Asthma Control Test Use in the Pediatric Care Center”.
Abstract #11: (RES-011-OR)**
Saini A*; Cavalcante R; Aquino Crisanto L; Sasaki J. “Outcomes of catheter-related arterial and venous thrombosis after enoxaparin therapy in neonates and infants with congenital heart disease”.
Abstract #12: (FEL-011-OR)
Abdul Kayoum A*; Rivera E; Reyes M; Almasarweh S; Ojito J; Burke R; Sasaki J. “Outcomes Of Bloodless Congenital Cardiac Surgery On Cardiopulmonary Bypass”.
Abstract #13: (FEL-012-OR)
Girgis S*; Seitz A; Runyon J; Gupta A; Sasaki N. “Incidence of post-operative left outflow tract obstruction in patients with juxtaposed atrial appendages”.
Abstract #45: (RES-025-CR)
Saini A*; Almasarweh S; Acosta S; Sasaki J. “Microphthalmia Syndrome 9: Novel mutations in STRA6 Gene”.
Abstract #1: (RES-001-OR)
Lopez Gonzalez MS*; Fonseca AG; Colon Guzman S; Castro Rivadeneira M; Felipez LM; Caicedo Oquendo LF. “Impact of Telehealth in Our GI Practice in South Florida”.
Abstract #23: (RES-003-CR)
Colón Guzmán S*; Roberts A; Sunny J; Bujarska M; Gonzalez-Vallina R. “A Forgotten Diagnosis: A Case About Anterior Cutaneous Nerve Entrapment Syndrome”.
Abstract #24: (RES-004-CR)
Colon Guzman S*; Prieto P; Gamboa H. “Acute Management of a Suspected Case of Cannabis Induced Cyclic Vomiting Syndrome”.
Abstract #28: (RES-008-CR)
Fonseca A*; Sunny J; Muniz Crim A; Felipez LM. “Anti-Tumor Necrosis Factor Alpha (TNF-Α) Infliximab-Induced Pleural Effusion and Pericarditis In Crohn’s Disease”.
Abstract #29: (RES-009-CR)
Fonseca A*; Sunny J; Muniz Crim A; Felipez LM. “Very Early Onset IBD (VEOIBD) Presenting With Recurrent Leukocytoclastic Vasculitis Preceded by Streptococcal Pharyngitis”.
Abstract #30: (RES-010-CR)
Fonseca A*; Roberts A; Barry R; Meyer K; Malvezzi L; Tackett J; Koyfman S. “Pediatric Patient Presenting with Upper Gastrointestinal Bleed Following Consumption of Whole Sunflower Seeds”.
Abstract #31: (RES-011-CR)
Gawron Roberts A*; Colon Guzman S; Bujarska M; Sunny J; Gonzalez-Vallina R. “Pediatric Patient Presenting with Diphyllobothrium Latum Infection Following Consumption of Raw Fish at a Local Sushi Restaurant”.
Abstract #32: (RES-012-CR)
Gawron Roberts A*; Bujarska M; Bauer M; Brathwaite C; Pelaez L; Reeves-Garcia J. “Gastric Adenocarcinoma and Proximal Polyposis of the Stomach in a Hispanic Pediatric Patient with APC Gene Variant c.-191T>G”.
Abstract #33: (RES-013-CR)
Gawron Roberts A*; Bujarska M; Muniz Crim A; Felipez LM. “A Case of Very Early Onset Inflammatory Bowel Disease (VEOIBD) Presenting with Salmonellosis”.
Abstract #37: (RES-017-CR)
Lopez Gonzalez MS*; Fonseca AG; Sunny J; Caicedo Oquendo LF; Felipez LM. “Inflammatory Bowel Disease and Hidradenitis Suppurativa: Is the Association Real?”.
Abstract #49: (RES-029-CR)
Smith J*; Saini A; Brathwaite C; Koyfman S. “A Case of Refractory Diarrhea and Malabsorption Secondary to Autoimmune Enteropathy in a 10-Year-Old Child”.
Abstract #52: (RES-032-CR)**
Suaris M*; Sunny J; Colon Guzman S; Johnson N; Arboleda R; Felipez LM. “A Case Series of Non-Bacterial Osteomyelitis Associated with Inflammatory Bowel Disease”.
Abstract #53: (RES-033-CR)
Sunny J*; Fonseca A; Rios M; Felipez LM. “Acute Pancreatitis in the setting of Lipoprotein Lipase Deficiency: A Familial Case”.
Abstract #54: (RES-034-CR)
Sunny J*; Lairet S; Muniz-Crim A; Goyal A; Felipez LM. “Hypersensitivity reaction to Ustekinumab in Pediatric Inflammatory Bowel Disease Patients.”
Abstract #55: (RES-035-CR)
Sunny J*; Bujarska M; Gawron A; Colon-Guzman S; Gonzalez-Vallina R. “Orientia Tsutsugamushi and subsequent development of auto-immune hepatitis in a liver transplant Patient”.
Abstract #56: (RES-036-CR)
Sunny J*; Fonseca A; Muniz Crim A; Felipez LM. “Pyoderma Gangrenosum presenting after changing from Anti-TNF to Ustekinumab”.
Abstract #61: (RES-001-QI)
Gawron Roberts A*; Fonseca A; Colon Guzman S; Vidal G; Rios M; Reeves-Garcia J; Farias A; Behnam M. “Improving Adherence to the Management of Acute Pancreatitis in the Pediatric Population.”
Abstract #66: (RES-006-QI)**
Riera-Canales C*; O’Farrell C; Zaidi Z; Gabay M; Felipez L. “Increasing Depression Screening In Admitted Patients 12-21 Years Old With Inflammatory Bowel Disease”.
Abstract #67: (RES-007-QI)**
Alruwaili A; Bujarska M; Lopez Gonzalez M; Sunny J*; Felipez LM; Behnam-Terneus M. “Appropriate Thromboembolic Prophylaxis Therapy in IBD Patients Admitted to the Hospital: A Proposed Risk Stratification Algorithm”.
Abstract #64: (RES-004-QI)
Deiros G; Frias J; Modir P*; Ramos-Garcia A; Milla M. “Improving HPV Vaccination Rates at NCH PCC”.
Abstract #21: (RES-001-CR)
Aquino Crisanto L*; Napky Raudales PJ; Girgis S; Jayakar P. “Complex combined Trisomy 14 and 21 Mosaicism and Multisystem Involvement in a Newborn”.
Abstract #36: (RES-016-CR)
Lopez Gonzalez MS*; Caicedo Oquendo LF. “Dorsal Agenesis of the Pancreas: A Rare Entity”.
Abstract #44: (RES-024-CR)
Saini A*; Kana SL; Visona C; Diaz A; Jayakar P. “Hypermethioninemia due to Adenosine Kinase Deficiency: Novel Mutations in ADK Gene diagnosed by Rapid Whole Genome Sequencing”.
Abstract #38: (RES-018-CR)
Mandel G*; Riera Canales C; O’Farrell C; Fader M. “Methotrexate Use in End-Stage Renal Disease for Treatment of Osteosarcoma”.
Abstract #39: (RES-019-CR)
Mandel G*; Pelaez L; Hogan A; Riera Canales C; O’Farrell C; Fader M. “All that grows isn’t malignant: The Hibernoma”.
Abstract #40: (RES-020-CR)
Napky Raudales P*; Barry R; Dantas M; Fader M. “More than meets the eye: Juvenile xanthogranuloma in a child with hyperlipidemia and bicytopenia”.
Abstract #41: (RES-021-CR)
Napky Raudales P*; Barry R; Shariati F; Sanchez E; Fonseca A; Niazi T; Maher O; Khatib Z. “Acute psychosis as an initial manifestation of a pineal germinoma in an adolescent male”.
Abstract #43: (RES-023-CR)
Riera-Canales C*; O’Farrell C; Mandel G; Abdella H. “Late relapse in Wilms Tumor: Does intense chemotherapy improve survival?”.
Abstract #50: (RES-030-CR)
Smith JD*; Maher O; Galvez Silva J; Khatib ZA. “Complete Response of Therapy Related Myelodysplastic Syndrome to Alisertib”.
Abstract #51: (RES-031-CR)
Smith J*; Behnam-Terneus M. “More Than Just a Rash: A Case of Multisystem Langerhans Cell Histiocytosis”.
Abstract #70: (NUR-010-QI)
Burke ML* & Taylor-Amador S. “Screening for Malnutrition in Oncology”.
Abstract #71: (NUR-011-QI)
Cruz D*. “Pain Management Protocol for Vaso-Occlusive Crisis in Children with Sickle Cell Disease in the Emergency Department at Nicklaus Children’s Hospital”.
Abstract #22: (RES-002-CR)
Cavalcante RC*; Dantas MA; Perez-Burnes L. “Go Where The Blood Is”.
Abstract #35: (RES-015-CR)
Graneiro A*; Mandel G; Laufer M. “What to consider when things start to heat up: A rare cause of FUO”.
Abstract #47: (RES-027-CR)
Smith J*; Behnam-Terneus M. “Rub-a-dub-dub Pathogens In The Tub”.
Abstract #2: (RES-002-OR)
Napky Raudales P*, Ness-Cochinwala M, Sendi P, and Totapally BR. “Epidemiology and outcomes of necrotizing enterocolitis in preterm neonates”.
Abstract #3: (RES-003-OR)
Sanchez-Solano N*; Bermudez Chicango D; Frade-Garcia A; Cruz H; Diaz-Barbosa M; Vallarino D; Totapally B; Llanos-Martinez A. “A Ten-Year Experience in the Management of Congenital Diaphragmatic Hernia in a Freestanding Children’s Hospital”.
Abstract #72: (NUR-012-QI)
Ferreyra G*; Perdomo M. “A Quality Improvement Project to Reduce Mother’s Own Milk Administration Error Risk in the NICU”.
Abstract #18: (NUR-017-OR)
Bandin A*; Roberts K; Valiente A. “Pedaling for Air: A Pediatric Inpatient Approach to Enhance Lung Function”.
Abstract #19: (NUR-018-OR)
Burke ML*; and Taylor-Amador S. “Parent Education Discharge Support Strategies”.
Abstract #20: (NUR-019-OR)**
Bandin A; Canizares A; Dieguez R; Klareich J*; Mirabal C. “There’s No Place like Home: A Standardized Discharge Plan to Reduce Hospital Readmission Rates”.
Abstract #69: (NUR-009-QI)
Augustin W*. “Empowered to Discharge: Development of Nurse-led Clinical Guidelines to Decrease Length of Stay and Cost”.
Abstract #73: (NUR-013-QI)
Lima-Keller N*; Suarez R*; Sztokfisz I; Sánchez A; Perez J; Cincotta C; Cortes I; Simon-Mengana K. “Horizon SharePoint Page”.
Abstract #14: (FEL-013-OR)
Ness-Cochinwala M*; Kobaitri K; Sendi P; Martinez P; Totapally BR. “Alteplase Use in Pediatric Necrotizing Pneumonia”.
Abstract #15: (FEL-014-OR)
Ness-Cochinwala M*; Totapally BR. “Risk Factors for Pediatric Pulmonary Embolism: A National Database Study”.
Abstract #4: (DRES-004-OR)
Acloque S*; Miranda P; Gupta A; Saman DM. “Oral health practices, knowledge, and attitudes among Hispanic immigrant parents of pediatric dental patients in South Florida”.
Abstract #5: (DRES-005-OR)
Cardenas MB*; Meincken M; Saman D; Patel P. “Motivational Interviewing to Improve Pediatric Dental Visits after General Anesthesia”.
Abstract #6: (DRES-006-OR)
Chery J*; Freitas V; Saman D; Gupta A. “Comparing Residents’ Cavity Using Er,Cr:YSGG Laser Versus Conventional High-Speed”.
Abstract #7: (DRES-007-OR)
Hui N*; Arevalo O; Gupta A; Saman DM; Wilson S. “Assessing the Current Research Infrastructure of Pediatric Dentistry Residency Programs: An Update for 2020”.
Abstract #8: (DRES-008-OR)**
Oliva M*; Aponte-Rodriguez S; Saman D; Gupta A. “Association Between Parental Acculturation and Children’s Oral Health”.
Abstract #16: (FEL-015-OR)**
Payson A*; Etinger V; Napky P; Montarroyos S; Ruiz-Castaneda A; Mestre M. “Risk of Serious Bacterial Infections in Febrile Infants With COVID-19”.
Abstract #25: (RES-005-CR)
Dantas M*; Cavalcante R; Hassor-Rivero S; Clemente M. “An Uncommon Cause of Fever of Unknown Origin”.
Abstract #26: (RES-006-CR)
Diaz M*; Torres D; Murphy K; Pulido A. “A Lump In My Chest, Will You Be Able To Guess?”.
Abstract #42: (RES-022-CR)
Navarro R*; Etinger V. “Don’t be Fooled! The Many Faces of Abdominal Pain”.
Abstract #48: (RES-028-CR)**
Smith J*; Behnam-Terneus M. “Vaping Associated Lung Injury: A Case of Rapid Respiratory Decompensation”.
Abstract #65: (RES-005-QI)
Liberti A; Montarroyos S*; Sanchez Solano N, Etinger V; Reyes M. “Implementation of Asthma Clinical Pathway”.
Abstract #74: (FEL-017-OR) §
Hassor S*; Payson A; Dantas M; Clemente M; Sanchez-Vegas C. “Identification of Pneumonia-Causing Pathogens using Karius Testing in Pediatric Patients”.
Abstract #9: (PHARM-009-OR)
Alvira-Arill G*; Chang N; Totapally B; Mulas N; Sotto I; Lee H. “Incidence of hyponatremia with the use of vasopressin in pediatric patients”.
Abstract #10: (PHARM-010-OR)
Kuchnik M*; Sotto I; Vuong M; Rodriguez Y; Lee H. “Evaluation of advancing chemotherapy administration times and the incidence of hemorrhagic cystitis/hematuria”.
Abstract #46: (RES-026-CR)
Sanchez-Solano N*; Laufer M; Della Volpe A. “Unexpected Case of Pulmonary Nodules”.
MichaelC
AmazonSmiles Page Shop
Little Acts of Love
Child & Adolescent Psychiatry
Ashley POM
Vision Day
Treatments and Procedures
Diamond Ball Sponsors
Diamond Ball Donation
Diamond Ball Tables and Seats
FGB Tickets
FGB Sponsorship
Patient Stories
Patient Stories
When to take your child to Urgent Care?
When to take your child to an Urgent Care?
When your pediatrician’s office is closed and your child needs medical treatment, we offer the comfort of walk-in urgent care service with no appointment needed at numerous South Florida locations.
With a typical lower co-pay than an emergency room, the Nicklaus Children’s Urgent Care Centers offer personalized and prompt care for babies, children, teens and young adults under 21 years old, provided by board-certified pediatric physicians for minor injuries and illnesses.
Nicklaus Children’s Urgent Care Centers offer COVID-19 testing for children with associated symptoms as part of an Urgent Care Center Visit.
1-833-Nick4Kids
Hours are 11 a.m. to 10 p.m. daily.

andrea-granados-endocrinology
mubeena-abdulkarim-cardiology
jordan-steinberg-plastic-surgery
roger-saldana-orthopedic-surgery
gracielaPOM
Pediatric Physical Therapy Residency Program
School Immunizations Sign-Up
Thank you
Virtual Education Request
sabiha-karakas-rothey-radiology
lauren-delgado-hardegree-radiology
halley-park-radiology
Michael
Laboratory Services Home
Planning Your Visit
andrew-sy
Review-Dr-Ramos
Review-Dr-Steinberg
Get Application FAQ

What is the Get App?
The GET App is used to allow mobile ordering at the Nicklaus Children’s Hospital Gift Shop, Golden Cub Café and the Miracles Café.
How do I get the mobile app?
You can download the Get App from the Google Play Store or the Apple App Store.
Can I order on the web, or just on the mobile app?
Do I need to register?
Yes. Once you are at the login page (link below) scroll to the section labeled Parents, Guardians or Other Relatives and then click on the Guest Registration’s Sign up now! link. https://get.cbord.com/nicklauschildrens/
How do I reset my password?
On the main login page there is a “I forgot my password” link. Once you click on the link, you will be prompted to enter the email address you registered with. Follow the instructions on the email you receive to reset your password.
What cafes/locations are offering this service? Will they have the same Hours of Operation?
The Golden Cub Café, Miracles Café, and the Gift Shop will offer items on the GET Mobile App. Golden Cub Café will have reduced hours on the mobile app only. In person hours will remain the same.
Golden Cub Café will open for lunch orders only on the mobile app.
Monday-Friday 11:30 am - 2:30 pm
Miracles Café will open
Sunday-Saturday 6:30 am - 10:00 pm
Nicklaus Children’s Hospital Gift Shop Gift Shop will open
Monday-Friday 10 am- 3 pm
How can I order food items? How does this work?
The GET App works like various other food ordering applications. You will need to download the Get Mobile app at Get App and register. A credit card will be required at the time of placing your order.
Where do I pick up my order?
Golden Cub Café order will be available for pickup in the dining room.
Miracles Café orders will be available at the pickup window.
Is delivery available?
Delivery is available for the Golden Cub Café and the Gift Shop. Miracles Café does not offer delivery.
Are the hours of operation the same on the mobile app ?
The hours of operation on the mobile app are slightly different for the Café’s. The Gift Shop hours are the same.
Golden Cub Café will open for lunch orders only
Monday - Friday 11:30 am - 2:30 pm
The Golden Cub Café in person hours remain the same.
Miracles Café will open
Sunday -Saturday 6:30 am - 10:00 pm
NCH Gift Shop will open
Monday - Friday 10:00 am - 3:00 pm
How do I know my order is available for pickup?
At the time of placing your order, you will select your pickup time. If you selected ASAP then your order will be ready within 15 minutes. You will receive an email confirmation with the time you selected for pickup after placing your order, but there will not be an additional email or notification showing when the order is available for pickup.
What if I cannot pickup my order on time?
We will hold your order for 15 min after your Pick up Time, then it will be discarded for Food Safety issues. No refund will be issued if you did not pick up your order.
Are all items available from the Golden Cub Café?
No. To provide the best customer experience, not all menu items are available. At this time, only Grab n Go and the Buffet Line will be available from the Golden Cub Café.
Are the prices different on the mobile app vs. in person at the Golden Cub Café or Miracles Cafe?
No. The prices you see on the GET Mobile App will be the same as shown in person at all locations.
What if I need to change my order? Or I ordered the incorrect item?
Changes on submitted orders are not allowed. You can cancel your order if it is not within 20 minutes of your pickup time. If you placed an order as “ASAP,” you will not be able to cancel the order.
Can I cancel my order?
You can cancel your order if it is not within 20 minutes of your pickup time. If you placed an order as “ASAP,” you will not be able to cancel the order.
Who do I contact if there is a mistake with my order or I have any questions?
Not at this time. In the future you will be able to, but this location is not yet active.
Payments / Refunds / Fees
What payment methods are accepted?
We accept all major credit cards. American Express, Discover, MasterCard, and Visa.
Are there any additional cost/fees?
• Golden Cub Café has a $1.50 Service Charge.
• Miracles Café and Nicklaus Children’s Hospital Gift Shop will not have any additional costs.
What is your Refund Policy?
If there is something wrong with your order, a refund can be done. Please come to the location where your order was placed and one of our cashiers will assist you.
Athena
rosa-monte-fernandez
Thank You
Success!
Thank you for submitting a status update.
PACT Home
Thank You
Directions to ER
Clinical Excellence
At Nicklaus Children’s Hospital, we dedicate ourselves daily to offering the best possible care to every child and family who come to us for hope and healing. We understand that quality and safety are the twin pillars of clinical excellence. We continuously evaluate our quality and safety performance to ensure that we meet and exceed national benchmarks and routinely incorporate evidence-based strategies to support a culture of continuous improvement.
Patients and families have an essential role in our quality and safety program. No one knows a patient better than the child’s parents or guardians. We look to parents and extended family members to share insights to enhance care and create a better experience to meet each patient’s needs.
Measuring Care Quality
As we strive to provide the best care experience possible, we steadfastly track key outcomes and measures that serve as quality and safety indicators.
The measures shown below are only a small sampling of the data we routinely measure and report as part of our commitment to quality and safety. Through measurement over time, we can identify practices that enhance these outcomes and identify opportunities for improvement.
Children receiving care in a hospital sometimes require a urinary catheter, a thin tube that drains urine from the bladder. Catheters are helpful for patients during their care or recovery, but they can also bring risks, including catheter-associated urinary tract infections (CAUTI). Minimizing the incidence of CAUTI contributes to patient safety. Nicklaus Children’s uses multiple strategies to minimize CAUTI, including steps taken by the clinical team before and after the catheter is placed.
Measurement
While patients are in the hospital, we track any urinary tract infections that occur that are associated with the use of a urinary catheter (CAUTI). By measuring such infections over time, we can quickly identify emerging trends that impact infections and adapt quickly to continuously improve our care.
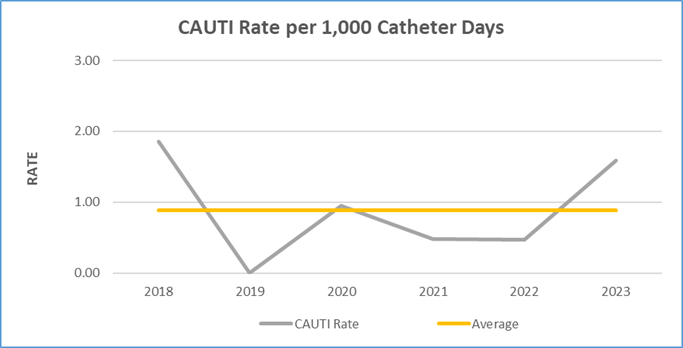 Fig 1. 2018-2023 Chart of CAUTI rate per 1,000 catheter days
Fig 1. 2018-2023 Chart of CAUTI rate per 1,000 catheter days
Continuous Improvement
Information about CAUTI are regularly reviewed by our Infection Prevention and Control staff along with other members of the care team to observe trends that may impact these events. Strategies to prevent CAUTI include using proper techniques for inserting and maintaining the urinary catheter. We also emphasize the importance of avoiding unnecessary urinary catheter use and removing the catheter when it is no longer needed. Rounding is done to ensure compliance with these strategies, and family representatives are part of our subject matter expert team to help us identify ways to improve continuously.
Collaboration to Improve Safety
Nicklaus Children’s submits our CAUTI data monthly to the Children's Hospitals' Solutions for Patient Safety (SPS) national collaborative. Hospitals from throughout the U.S. are part of this network that tracks hospital-acquired conditions to share best practices regarding patient safety. The purpose of this is to help hospitals learn from their combined experiences so that all can enhance patient safety.
Children receiving care in a hospital sometimes need to have a central line placed into a large blood vessel in their bodies. Central lines are intravenous catheters that are used to provide the patient with fluids, medications and nutrients. This important tool of the medical team can sometimes pose risks, including central line-associated blood stream infections (CLABSI). Minimizing the incidence of CLABSI contributes to patient safety. Nicklaus Children’s uses multiple strategies to minimize these events, including steps taken before and after the central line is placed.
Measurement
While patients are in the hospital, we track any infections that occur that are associated with the use of a central line. By measuring such infections over time we can quickly identify emerging trends that impact infections and adapt quickly to improve our care and reduce future events.
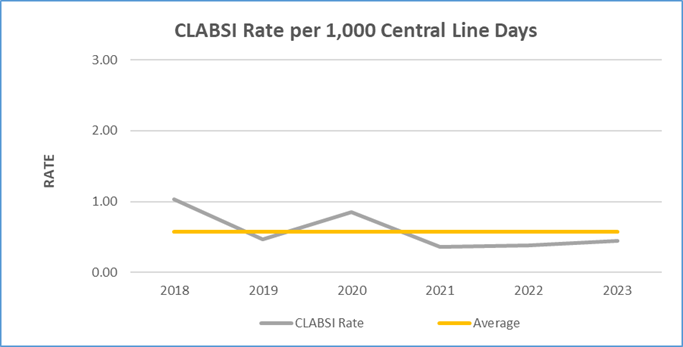 Fig 2. 2018-2023 Chart of CLABSI rate oer 1,000 central line days.
Fig 2. 2018-2023 Chart of CLABSI rate oer 1,000 central line days.Continuous Improvement
Information about CLABSI are regularly reviewed by our Infection Prevention and Control staff along with other members of the care team to observe trends that may impact these events. Strategies to prevent CLABSI include using proper techniques for inserting and maintaining the central line and the associated dressings. After the line is inserted, we regularly assess the necessity of each central line and remove them when they are no longer needed to support the patient’s care. Rounding is done to ensure compliance with these strategies, and family representatives are part of our subject matter expert team to help us identify ways to improve continuously.
Collaboration to Improve Safety
Nicklaus Children’s submits our CLABSI data monthly to the Children's Hospitals' Solutions for Patient Safety (SPS) national collaborative. Hospitals from throughout the U.S. are part of this network that tracks hospital-acquired conditions to share best practices regarding patient safety. The purpose of this is to help hospitals learn from their combined experiences so that all can enhance patient safety.
success
Success!
igive
Virtual Birthmarks Meeting
Virtual Birthmarks Meeting
margaret-wright-ortho
Portal-de-Pacientes
robert-flood-emergency
Dance-ppcsdm
Donar
Donar
pact-page
Concussion Screening
Thank You
Thank you! Your request has been submitted.
A team member will contact you regarding your inquiry within the hours you have indicated.
Return to the Concussion ClinicCrypto
annette-medina-gastro
Review-Dr-Firestone
Review-Dr-Feldman
RSVP - IRSF Center of Excellence
The International Rett Syndrome Foundation and Nicklaus Children’s Hospital
invite you to a celebration to Commemorate the hospital’s Center of Excellence Designation
(Ver en Español)
PACT Legacy Night RSVP

The Pediatric Advanced Care Team (PACT)
at Nicklaus Children's Hospital invited you to a special evening as we honor your child and family.
Thursday, February 20, 2025
6:00 p.m.
(Ver en Español)
San Diego Zoo Kids
Nicklaus Children’s Hospital is pleased to offer the San Diego Zoo Kids channel in every patient room on channel 21. San Diego Zoo Kids is an innovative television channel that provides patients and families with animal-oriented programming that is both entertaining and educational. The stories told through the channel share the joy of animals with children, some of whom may be unable to visit the local zoo, due to illness.
San Diego Zoo Kids offers:
- Wildlife stories
- Quizzes about animals and their habitats
- Short video vignettes
- Videos from San Diego Zoo and other zoos around the world
The stories shared on the channel not only provide wholesome entertainment to children during their time of healing but inspire them to appreciate wildlife and their natural habitats.
Radiothon
PCC Flu Vaccine Spanish

Ahora Más Que Nunca:
¡Proteja a su Hijo(a) Contra la Gripe!
Asegurarse de que su hijo ha recibido la vacuna anual contra la gripe es importante ahora más que nunca. A medida que los niños vuelven a la escuela y a las actividades previas a la pandemia, se espera que la gripe y otros virus respiratorios aumenten según lo dice la Academia Americana de Pediatría.
Se recomienda que todas las personas de 6 meses o más se vacunen contra la gripe antes de finales de noviembre de 2022, ya que las vacunas siguen siendo la mejor manera de prevenir enfermedades graves y mantener a los niños en las escuelas.
Programe la vacuna contra la influenza de su hijo(a) en uno de los cuatro centros de atención pediátrica de Nicklaus Children's (Nicklaus Children's Pediatric Care Centers):
Solicite una cita
Totally 93.9
610 WIOD
Mariangel POM
Health Survey
newfit4kidsapp
We are pleased to announce that Nicklaus Children's Hospital has a new mobile app.
Please tap/hold the Apple Store icon below to install.
MyNicklaus
MyNicklaus app – now available in app stores – helps families access our hospital and health system service locations, pediatric health library content, virtual care services as well as receive real-time alerts. The digital platform features physician directories, appointment scheduling, patient records, bill pay options and enables families to verify hours, locations and wait times for urgent care centers.
Coming soon to the app: Gozio Health’s patented indoor wayfinding with turn-by-turn navigation to help families find their way to hospital departments and physician offices, as well as on-site hospital amenities, such as dining options, restrooms, ATMs, the gift shop and more.
Children's Experiences
Brain Donate Now
bingo sessions
Majory Stoneman Douglas
fiuroarthon
Monarch High School
North Broward Prep
Review-West-Kendall-UCC
Review-West-Bird-UCC
Review-Palmetto-Bay-UCC
Review-Palm-Beach-UCC
Review-Midtown-UCC
Review-Miramar-UCC
Review-Miami-Lakes-UCC
Review-Doral-UCC
Review-Homestead-UCC
Review-Hialeah-UCC
specialgift
Meet the Fetal Care Center Team
Level II De George Neonatal Intensive Care Unit
The 16 bed De George Neonatal Intensive Care Unit at Jupiter Medical Center, made possible through the generosity of the Lawrence J. and Florence A. De George Charitable Trust, is equipped to care for babies born as early as 32 weeks. The unit adheres to policies, procedures, training and competencies shared through the collaboration with Nicklaus Children’s. In addition, the unit is staffed around-the-clock by Nicklaus Children’s neonatologists, and Nicklaus provides nursing staff oversight.
Features of the unit include:
- Advanced monitoring and technology
- A family lounge
- Treatment rooms
- Two private nesting rooms to foster bonding
- An infant feeding preparation space
Cludo Test
Jaxon
POM gloria
Neighborhood news
waystogive
Donate Items
Jayden
GENEuary Schedule

Join Us for GENEuary 2023, Live and Virtual Options Available
Nicklaus Children’s Hospital is collaborating in January with other organizations to offer “GENEuary 2023,” a month-long program to promote understanding of the role of genetics and genetic testing in diagnosis and treatment of disease. During the month, the hospital’s Personalized Medicine and Health Outcomes team is hosting live and virtual events to share the latest developments in genomic medicine.
Download the Program Booklet
Event Schedule
Date
|
Time
|
Speaker
|
Topic
|
Location
|
Zoom
|
Passcode
|
| Thursday, March 30, 2023 |
6:00 PM |
Dr. Jada Benn Torres & Dr. Carlina de la Cova |
Ancestry, Heritage and Health: A Community Conversation |
Downtown Miami Charter School, 305 NW 3rd Ave, Miami, FL 33128 |
Go to Zoom Link |
655759 |
|
Friday,
January 13th, 2023
|
8:00 AM |
Dr. Nina Brodsky |
Multisystem inflammatory Syndrome (MIS-C) - Critical Review and Lessons Learned |
Grand Rounds / Virtual |
Go to Zoom Link |
860 7024 5872 GR2223 |
| Wednesday, January 18th, 2023 |
2:00 PM |
Dr. Yana Vorontsova |
Role of Precision Medicine and its Benefits to Patients |
Nursing Grand Rounds / Virtual / NCHS Main Auditorium |
Go to Zoom Link |
860 7024 5872 GR2223 |
| Friday, January 20th, 2023 |
8:00 AM |
Dr. Monique Jindal |
The Impact of Racism on Health |
Grand Rounds/ Virtual / NCHS Main Auditorium |
Go to Zoom Link |
860 7024 5872 GR2223 |
| Tuesday, January 24th, 2023 |
12:00 PM |
Dr. Lina Felipez |
Inflammatory Bowl Disease, Past, Present and Future |
Resident Luncheon / Hybrid / NCHS Main Auditorium |
Go to Zoom Link |
997 8081 3610 |
| Monday, January 30th, 2023 |
7:30 PM |
Dr. Paul Wolpe |
Who Do You Think You Are? How Genomics and Artificial Intelligence Challenge Our Sense of Self |
Community Event at
Miami Beach JCC
4221 Pine Tree Dr
Miami Beach, FL
33140 / Virtual |
Go to Zoom Link |
842 0024 8606 |
| Friday, February 3rd, 2023 |
8:00 AM |
Dr. Chun-Hung Chan |
The Importance of Biobanks |
Grand Rounds / Hybrid / NCHS Main Auditorium |
Go to Zoom Link |
860 7024 5872 GR2223 |
No Surprises Act
Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or are treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from balance billing. In these cases, you shouldn’t be charged more than your plan’s copayment, coinsurance and/or deductible.
What is “balance billing” (sometimes called “surprise billing”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, like a copayment, coinsurance, or deductible. You may have additional costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” means providers and facilities that haven’t signed a contract with your health plan to provide services. Out-of-network providers may be allowed to bill you for the difference between what your plan pays and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your plan’s deductible or annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in- network facility but are unexpectedly treated by an out-of-network provider. Surprise medical bills could cost thousands of dollars depending on the procedure or service.
You’re protected from balance billing for:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of-network provider or hospital, the most they can bill you is your plan’s in-network cost-sharing amount (such as copayment, coinsurance, and deductibles). You can’t be balance billed for these emergency services. This includes services you may get after you’re in a stable condition, unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services. If your insurance ID card says “fully insured coverage,” you can’t give written consent and give up your protections not to be balance billed for post-stabilization services.
Certain services at an in-network hospital or ambulatory surgical center
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers can bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, and intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed. If you get other types of services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections. If your insurance ID card says “fully insured coverage,” you can’t give up your protections for these other services if they are a surprise bill. Surprise bills are when you’re at an in-network hospital or ambulatory surgical facility and a participating doctor was not available, a non-participating doctor provided services without your knowledge, or unforeseen medical services were provided.
Services referred by your in-network doctor
If your insurance ID card says “fully insured coverage,” surprise bills include when your in-network doctor refers you to an out-of-network provider without your consent (including lab and pathology services). These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed. You may need to sign a form (available on the Department of Financial Services’ website) for the full balance billing protection to apply.
You’re never required to give up your protections from balance billing. You also aren’t required to get out-of-network care. You can choose a provider or facility in your plan’s network.
When balance billing isn’t allowed, you also have these protections:
- You’re only responsible for paying your share of the cost (like the copayment, coinsurance, and deductibles that you would pay if the provider or facility was in-network). Your health plan will pay any additional costs to out-of-network providers and facilities directly.
- Generally, your health plan must:
- Cover emergency services without requiring you to get approval for services in advance (also known as “prior authorization”).
- Cover emergency services by out-of-network providers.
- Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
- Count any amount you pay for emergency services or out-of-network services toward your in-network deductible and out-of-pocket limit.
If you think you’ve been wrongly billed, you may contact CMS at 1-800-985-3059. Visit: http://www.cms.gov/nosurprises/consumers for information about your rights under federal law.
The contents of this notice explain all of your rights and protections related to balance billing under state and federal law. Visit https://m.flsenate.gov/Statutes for more information about Florida’s law.
You have the right to receive a Good Faith Estimate
Under the law, health care providers need to give patients who don’t have insurance or who are not using insurance an estimate of the bill for medical items and services.
- You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment, and hospital fees.
- Make sure your health care provider gives you a Good Faith Estimate in writing at least 1 business day before your medical service or item. You can also ask your health care provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
- If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
- Make sure to save a copy or picture of your Good Faith Estimate.
For questions or more information about your right to a Good Faith Estimate, visit www.cms.gov/nosurprises or call 850-908-2000.
Graduate Administrative Internship
The Graduate Student Administrative Internship at Nicklaus Children's Health System is a 10-12 week paid opportunity for graduate students enrolled in health management programs to gain unique and valuable experience for professional growth. The internship program establishes a platform for creating meaningful relationships within the organization and the South Florida community, as well as exposure to operating a health system.
Interns will join an NCHS team for the summer to complete a capstone project and understanding how the department functions. Project work will include initiatives that both fulfill an organizational need and align with the intern’s interests. The intern will also have the opportunity to shadow other NCHS teams. Upon completion, the intern should be able to summarize the department’s responsibilities within the health system and outline the key points of knowledge provided by the department director and staff.
Testimonials from our Interns
Teams to join include:
- Corporate Marketing & Communications
- Corporate Finance
- Information Technology
- Quality, Safety, and Innovation
- Talent Management & Effectiveness (HR)
Application Requirements
The application for the Nicklaus Children’s Health System Administrative Internship will be available in early January. Applicants will be asked to submit the following by Friday, February 28th, 2025 at 11:59 p.m. EST.:
- Resume
- Cover Letter (one page, single spaced, 12-point Times New Roman Font) answering the following questions:
- Why you are interested in Nicklaus Children’s Health System?
- What are your top 3 departments of interest out of the following and why: Finance; Information Technology (IT); Marketing & Communications; Quality, Safety & Innovation; and Talent Management & Effectiveness (HR).
- What are your goals for the internship and career objectives within healthcare administration?
Incomplete applications will not be considered.
Internship Application Timeline
Applications are rolling.
Application Receipt Deadline: Friday, February 28th, 2025 at 11:59 p.m. EST.
Selection Announcement: March, 2025
Start Date: June 2025
Qualifications
- Be currently enrolled in an accredited Master’s degree program with a concentration in healthcare.
- Able to work full-time during the summer (Monday-Friday, 8 hours/day during business hours).
- Be fluent in reading, writing and speaking English.
- Demonstrate intelligence, initiative, independence, adaptability and strong communication skills.
Selection Process
Interested applicants will submit their resume and cover letter defining their area of interest for the internship. Each application will be given careful review on a rolling basis, upon which qualified applicants will be contacted for first-round phone-interviews with the internship coordinator. After the round of phone-interviews, selected candidates will be invited to an additional round of interviewing via video conference with their potential preceptor team.
Please note that completion of the internship does not guarantee prolonged employment within Nicklaus Children’s Health System. Nicklaus Children’s Health System is an equal opportunity employer. Selection of applications will be conducted without regard to race, religion, creed, sex, national origin or disability.
Again, incomplete applications will not be considered. Nicklaus Children’s maintains the right to modify the application timeline (selection dates) as time and schedules permit.
Frequently Asked Questions
Where can I apply?
Please apply on our Career Portal by searching for the job title, Administrative Intern.
When are the application materials due?
Friday, February 28th, 2025 at 11:59 p.m. EST. Applications received after this date will not be considered.
What documents should I submit for consideration of the Internship program?
Updated resume and cover letter (one page, single spaced, 12-point Times New Roman Font) answering the following questions:
- Why you are interested in Nicklaus Children’s Health System?
- What are your top 3 departments of interest out of the following and why: Finance; Information Technology (IT); Marketing & Communications; Quality, Safety & Innovation; and Talent Management & Effectiveness (HR).
- What are your goals for the internship and career objectives within healthcare administration?
When will the intern be selected?
Applications are rolling, all applicants will be notified of a decision by early March 2024.
Will I have an opportunity to see other facets of Nicklaus Children’s?
Yes! Interns will have exposure to their preceptor’s team and the opportunity to take part in: hospital tours, off-site facility tours, corporate meet & greets, and other shadowing experiences. Please note, in-person opportunities are subject to change.
Does the administrative internship choose students from any university?
Nicklaus Children’s has a strong preference for choosing qualified applicants from an accredited graduate program.
Fellowship Training Programs Home
GME Home
Home
Coral Springs High School
Pompano Beach High School
St. Thomas Aquinas High School
POM Nicolas
Thank You
Thank you! Your request has been submitted.
RSVP Heart Reunion
Heart Institute Patient Reunion 2025
Registration is now open.
Thank You
giving council
Alexandra
2022 March 2
Survey Readiness
Survey Readiness
Kenneth C. Griffin Surgical Tower

As a representation of Nicklaus Children's Hospital's unwavering commitment to prioritizing pediatric healthcare, a new five-story, 131,000-square-foot surgical tower has been built to replace the existing operating rooms. The Kenneth C. Griffin Surgical Tower elevates the hospital's surgical care offerings in an environment that caters to the patient experience combined with leading-edge technology to ensure children and adolescents don’t have to leave South Florida for expert pediatric surgical care. The Griffin Surgical Tower is named for philanthropist Ken Griffin, Founder and CEO of Citadel and Founder of Griffin Catalyst, who made a transformational $25 million gift to support the tower and the future of pediatric surgical care.
The new tower is located at the center of campus, away from the hospital perimeter and neighborhood, includes state-of-the-art operating suites to replace facilities that were 35 years old and lack the size and ceiling height necessary to accommodate the latest equipment and surgical teams. Pediatric surgical offerings include trauma care, surgical cancer interventions, pediatric plastic and reconstructive surgeries including cleft lip-and-palate, orthopedic and spine, brain and heart surgeries.
Kenneth C. Griffin Surgical Tower by the Numbers
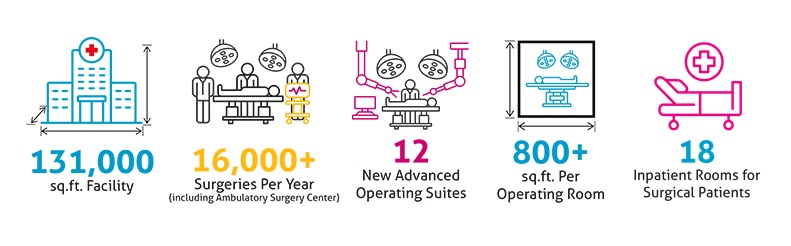
The addition of the Kenneth C. Griffin Surgical Tower also includes innovative features to provide elevate the comfort of our patients and their families before and during their procedure. Some highlights include:
-
Up-to-the-minute texting platform for surgical updates
-
Virtual reality tools to keep patients calm and entertained pre- and post- surgery
-
Immersive technology to display videos and reduce anxiety giving patients a theater-like experience
-
The Griffin Surgical Tower has connecting walkways to the cardiac intensive care unit, the intraoperative MRI suite, and the patient observation unit (3 south).
Learn more about the surgical technology and patient family amenities offered.
Service Offerings by Floors
| 6 |
Dedicated unit with 18 inpatient rooms for surgical patients.
*Due to the ceiling height necessary to accommodate the latest equipment, there is no fifth floor.
|
| 4 |
Sterile processing and surgical administrative offices
|
| 3 |
Pre-and post-operative suites, 2 anesthesia induction rooms, and 6 operating rooms dedicated to ENT, oncology, ophthalmology, orthopedics, pediatric general surgery, and urology.
|
| 2 |
Pre-and post-operative suites, 2 anesthesia induction rooms, and 6 operating rooms dedicated to brain, heart, orthopedic spine, pediatric trauma, and plastic surgery.
|
| 1 |
Lobby
Registration and access
|
If you’d like to learn more on how you can contribute to this ongoing project, please visit this page or email our foundation at nchf@nicklaushealth.org. Our staff is available to explore custom naming opportunities inside the new tower, which includes the hospital’s four institutes focused on providing pediatric care related to the brain, heart, cancer and blood disorders, and orthopedics.
Kenneth C. Griffin Surgical Tower

As a representation of Nicklaus Children's Hospital's unwavering commitment to prioritizing pediatric healthcare, a new five-story, 131,000-square-foot surgical tower has been built to replace the existing operating rooms. The Kenneth C. Griffin Surgical Tower elevates the hospital's surgical care offerings in an environment that caters to the patient experience combined with leading-edge technology to ensure children and adolescents don’t have to leave South Florida for expert pediatric surgical care. The Griffin Surgical Tower is named for philanthropist Ken Griffin, Founder and CEO of Citadel and Founder of Griffin Catalyst, who made a transformational $25 million gift to support the tower and the future of pediatric surgical care.
The new tower is located at the center of campus, away from the hospital perimeter and neighborhood, includes state-of-the-art operating suites to replace facilities that were 35 years old and lack the size and ceiling height necessary to accommodate the latest equipment and surgical teams. Pediatric surgical offerings include trauma care, surgical cancer interventions, pediatric plastic and reconstructive surgeries including cleft lip-and-palate, orthopedic and spine, brain and heart surgeries.
Kenneth C. Griffin Surgical Tower by the Numbers
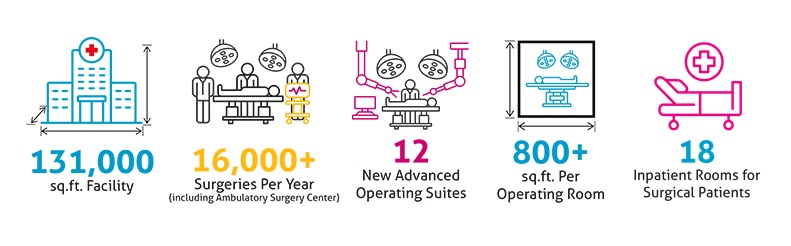
The addition of the Kenneth C. Griffin Surgical Tower also includes innovative features to provide elevate the comfort of our patients and their families before and during their procedure. Some highlights include:
-
Up-to-the-minute texting platform for surgical updates
-
Virtual reality tools to keep patients calm and entertained pre- and post- surgery
-
Immersive technology to display videos and reduce anxiety giving patients a theater-like experience
-
The Griffin Surgical Tower has connecting walkways to the cardiac intensive care unit, the intraoperative MRI suite, and the patient observation unit (3 south).
Learn more about the surgical technology and patient family amenities offered.
Service Offerings by Floors
| 6 |
Dedicated unit with 18 inpatient rooms for surgical patients.
*Due to the ceiling height necessary to accommodate the latest equipment, there is no fifth floor.
|
| 4 |
Sterile processing and surgical administrative offices
|
| 3 |
Pre-and post-operative suites, 2 anesthesia induction rooms, and 6 operating rooms dedicated to ENT, oncology, ophthalmology, orthopedics, pediatric general surgery, and urology.
|
| 2 |
Pre-and post-operative suites, 2 anesthesia induction rooms, and 6 operating rooms dedicated to brain, heart, orthopedic spine, pediatric trauma, and plastic surgery.
|
| 1 |
Lobby
Registration and access
|
If you’d like to learn more on how you can contribute to this ongoing project, please visit this page or email our foundation at nchf@nicklaushealth.org. Our staff is available to explore custom naming opportunities inside the new tower, which includes the hospital’s four institutes focused on providing pediatric care related to the brain, heart, cancer and blood disorders, and orthopedics.
2022 March 9
farah-garmany-cardiology
2022 March 16
Programs
Motor Development Milestones
Parents have several ways to track their children’s progress as they grow. Some of the most important tools for both parents and pediatricians in this effort are developmental milestones. These milestones essentially provide a checklist throughout early childhood to determine how your child is tracking compared to other children of the same age, according to the American Academy of Pediatrics.
The list of milestones is quite large and covers multiple categories, including social and emotional milestones, language and communication milestones, cognitive milestones and movement and physical development milestones. These milestones change over time as your children age. The CDC tracks milestones for the ages of 2 months, 4 months, 6 months, 9 months, 1 year, 18 months, 2 years, 3 years, 4 years and 5 years.
What are common fine motor delays to look for?
Here are just a few of the many milestones to look out for from birth to 3 years of age, and some of the implications if the milestones are not achieved. This chart was compiled using data from both the CDC and the American Occupational Therapy Association (AOTA).
Motor Skills Milestones in Babies

| Age |
Developmental Milestone |
Possible Implications If Milestones Not Achieved |
2-6 months
|
- Can hold head up and begins to push up when lying on stomach
- Follows things with eyes and recognize people at a distance
- Plays with both hands at midline and brings hands and toys to mouth
- Can hold, shake and swipe at toys
- Uses hands and eyes together to reach for toys
|
- Lack of muscle development
- Delay of independent play
- Delays in interactions with toys and sensory objects, contributing to delays in sensory development
|
| 6-12 months |
- Reaches and grasps in all directions
- Shows curiosity about things and tries to pick up things that are out of reach
- Picks things up with thumb and index finger
- Imitates simple motor actions (shaking, banging, clapping)
- Transfers object from one hand to the other
- Begins to use toys according to their purpose
- Begins to finger feed and to hold a bottle
|
- Lack of muscle development
- Delay of independent play
- Delays in interactions with toys and sensory objects, contributing to delays in sensory development
|
Motor Skill Milestones in Toddlers

| Age |
Developmental Milestone |
Possible Implications If Milestones Not Achieved |
| 1-2 years |
- Plays games such as “peek-a-boo” and “pat-a-cake”
- Starts to use common items such as eating utensils or hairbrushes correctly
- Puts objects in small spaces and stacks objects such as blocks
- Self-feeds with a spoon with minimal assistance
- Pokes with their index finger
- Begin to imitate drawing lines with a crayon
|
- Lack of hand and finger strength development
- Delay of independent play skills
- Delay of self-feeding and other self-care skills
- Delay of object manipulation skills
|
| 2-3 years |
- Might use one hand more than the other
- Builds towers of four or more blocks
- Follows two-step instructions, such as “Pick up your clothes and put them in the closet.”
- Draws or paints circles using a wrist action
- Dresses and undresses self
- Uses both hands to complete tasks such as snipping with scissors and buttoning
- Can work toys with levers and moving parts
|
- Delay of self-feeding and other self-care skills
- Delay of pre-writing skills development
- Delay of object manipulation skills, such as using pencils or scissors
- Frustration when trying to manipulate small objects or toys
|
Along with working closely with your pediatrician, you can also use the Milestone Tracker mobile app offered by the CDC to monitor developmental progress.

What should you do when you notice a motor delay in your child?
The large number of milestones for your children can be hard to monitor all by yourself, which is why it’s important to establish a close partnership with a trusted pediatrician. With each visit to the pediatrician’s office, you and your doctor can review your child’s progress and look for any areas where they may be showing delays.
If you or your pediatrician notice any developmental delays, you’ll want to discuss the treatment options available for your child. Early intervention is often the key to your child’s future social and academic success.
The Rehabilitation Services team at Nicklaus Children’s Hospital offers a wide range of services to help children with most types of developmental delays. From speech-language pathologists to physical therapists to occupational therapists and more, Nicklaus’s Rehabilitation Services team is ready to assist you and your family and help your children achieve their full potential.
While appointments are available throughout the day, appointments are available between the hours of 8 a.m. and 2 p.m. So, if your child is preschool age and in need of rehabilitation services, don’t delay. You can request an appointment by calling (305) 663-8413 or by scheduling an appointment online.
Prepared by:
Narda Henry, MS, OTR/L, Clinical Specialist
Jenny Guerrero, OTR/L, Clinical Specialist
DAISY Nurse Leader Award
 The DAISY (Diseases Attacking the Immune System) Award is an international recognition program that honors and celebrates the skillful, compassionate care nurses provide every day. The DAISY Foundation was established by the family of J. Patrick Barnes after he died from complications of the auto-immune disease ITP in 1999. During his hospitalization, they deeply appreciated the care and compassion shown to Patrick and his entire family. When he died, they felt compelled to say “thank you” to nurses in a very public way.
The DAISY (Diseases Attacking the Immune System) Award is an international recognition program that honors and celebrates the skillful, compassionate care nurses provide every day. The DAISY Foundation was established by the family of J. Patrick Barnes after he died from complications of the auto-immune disease ITP in 1999. During his hospitalization, they deeply appreciated the care and compassion shown to Patrick and his entire family. When he died, they felt compelled to say “thank you” to nurses in a very public way.
We are excited to add The DAISY Nurse Leader Award to our DAISY Program!
The DAISY Nurse Leader Award recognizes nurses who are extraordinary in the impact they have on compassionate patient care. Honorees can be any nurse leader who impacts patient care directly including supervisors, managers, educators or nurses who specialize in case management, informatics or patient flow.
Nominate a Nurse Leader by describing the impact they have had on staff and the patient care they manage!
Nominate a Nurse Leader for the Daisy Award
This Nurse Leader impacts staff and/or the patient care they manage by:
- Role modeling extraordinary behavior
- Creating an environment where attributes of trust, compassion, mutual respect, continued professional development and ethical behavior are modeled and supported
- Motivating staff with a shared vision and enthusiasm to achieve better outcomes for themselves and for their patients
- Promoting and enhancing the image of nursing within the organization, the community and the profession
Patients, visitors, employees or physicians may nominate a deserving nurse by filling out the nomination form and submitting it to the nominee's nursing manager. We will be presenting 4 awards per year.
Daisy Nurse Leader Award Nomination
The DAISY (Diseases Attacking the Immune System) Award is an international recognition program that honors and celebrates the skillful, compassionate care nurses provide every day.
Nominate a Nurse Leader by describing the impact they have had on staff and the patient care they manage! We will be presenting 4 awards per year. Share your story!
Fill out the Nomination Form
If you have any questions, please contact Miosotis Falcon at 786-624-3320 or via email at Miosotis.Falcon@Nicklaushealth.org.
Thank You
Undergraduate Administrative Internship
The Undergraduate Student Administrative Internship at Nicklaus Children's Health System is an opportunity for undergraduate students enrolled and majoring in any Business Management program to gain unique and valuable experience for professional growth.
Nicklaus Children’s Health System, offers administrative internships in areas as diverse as the hospital itself such as:
- Organizational Development
- Talent Management
- Law
- Finance
- Marketing
- Information Technology
- and many others.
All students requesting to rotate at Nicklaus Children's Hospital must be enrolled in a credit program with an affiliated institution (see our affiliated institutions).
Please keep in mind that due to the size of our patient population and staff, the processing of placements may take 4 to 6 weeks.
Nicklaus Children's Hospital and Health System employees are not able to do their rotations in the same department/center they currently work or during scheduled work hours. They must also follow all student requirements.
Allied Health Rotations
Nicklaus Children's Hospital hosts over 2,000 students annually for academic-credit programs, allowing the students to gain hands on experience as part of their school’s curriculum.
Thank you for your interest in joining Nicklaus Children's Hospital as student. Whether you are joining as an intern, extern, or rotation student, you’ll find Nicklaus Children's Hospital to be a rewarding place to receive hands on experience.
This page is for all students enrolled and majoring in patient contact fields of study. These include but are not limited to:
- Radiology Technologies
- Respiratory Therapy
- Social Work
- Physical Therapy, Occupational Therapy, Speech-Language Pathology and Audiology.
Please keep in mind that due to the size of our patient population and staff, the processing of placements may take 4 to 6 weeks.
All students requesting to rotate at Nicklaus Children's Hospital must be enrolled in a credit program with an affiliated institution (see our affiliated institutions).
What are the requirements for an Allied Health Rotation at Nicklaus Children's Hospital?
Students will be required to meet the following criteria:
- Background check
- Cleared drug test
- Must currently be in good health
- Current CPR card (required for most clinical/allied health students. If your CPR certification is due to expire during your rotation, you must renew it to have a viable certification)
- Current PPD check or Chest X-Ray
- Vaccination records (including Covid-19)
- Receive a flu vaccine if attending during Dec. 1st – April 1st. (Only medical exemptions will be considered if the Flu vaccine medical exemption form is completed by a certified medical professional)
- Once approved by your school, the school representative must request placement by contacting our Education Program/ Internship Specialist at studentplacement@nicklaushealth.org
- Your school program coordinator will provide you with all required forms and information to rotate at Nicklaus Children's Hospital.
After Approval is Confirmed
- You must ensure to always sign-in and out with your assigned number/userID, when doing your clinical hours.
- Wear your school student ID at all times.
- Wear clean school approved uniform.
- Follow all the Nicklaus Children's Hospital policies outlines in the Student Orientation Manual.
Nicklaus Children's Hospital and Health System employees are not able to do their rotations in the same department/center they currently work or during scheduled work hours. They must also follow all student requirements.
Teen Academic Year Program
Nicklaus Children’s Hospital has partnered with Miami-Dade County Public schools for full academic year internships (Aug-May) for students to gain relevant skills and experiences in healthcare administration, while receiving academic credit.
Program Details
- This program is for full–time M-DCPS High School junior or senior students who are enrolled in M-DCPS Academic Internship program with an unweighted GPA of 2.5 or better and have excellent school attendance.
- It requires a 5-10 hour a week commitment with a flexible schedule, which can be a virtual, hybrid or in-person capacity.
- Our mentors will offer their time and talents to the student intern providing meaningful, career-related experiences. The mentor provides weekly time sheets and quarterly grade evaluations during the internship
How to enroll
Students, all applications are facilitated through the schools. Please search for your school’s internship coordinator provide you with all required forms and information to rotate at Nicklaus Children's Hospital.
Search for your coordinator
For any other questions about this program please contact our Education Program/Internship Specialist by email at studentplacement@nicklaushealth.org
Student and Observer Programs
2022 March 23
NCPS Martin & Palm Beach
Physician Outreach Home
Meet the Physician Liaison Team
The Physician Liaisons and Outreach Services team connects with physicians, practice staff and other healthcare providers in multiple areas at a local, regional and national level to assist with service line access improvement and practice management support. Our goal is to visit, engage, educate and effectively communicate and serve physicians, practice staff, and other healthcare providers to develop and build lasting relationships as well as inspire loyalty.
Request a Meet & Greet
Request Marketing Collateral
Subscribe to Newsletter
DRIVE Program Home
Physician Outreach
Thank You
Thank You for submitting a request!
One of your physician liaisons will contact you shortly to schedule a Meet and Greet.
Patient Stories
Patient Stories
Sarcoma & Solid Tumor Program Home
Sarcoma & Solid Tumor Program Home
Treatments and Procedures
Treatments and Procedures
Conditions we Treat
Conditions we Treat
Developmental Screenings & Evaluations
Developmental evaluations are recommended from birth to identify potential developmental delays (motor, speech), learning and/or behavioral concerns during the different stages of childhood.
Infancy
- Within the first 3 months of life
- 6 months
- 9 months
- 12 months
Toddler (1 - 3 years of age)
- 18 months (1.5 years of age)
- 36 months ( 3 years of age)
Preschool (3 - 5 years of age)
School-Age (6+ years of age)
Neurology Evaluation
A neurologist will perform a neurological screening and work with the family to schedule follow-up visits. If necessary, the neurologist will provide recommendations for your child for physical, occupational or speech therapies.
Neuropsychological Assessments
If a developmental concern is identified, the patient will be referred to a comprehensive neurodevelopmental evaluation with a pediatric neuropsychologist. Evaluations can last between 90 minutes to three hours, depending on the child’s age.
Starting at age five, a neuropsychologist will perform comprehensive evaluations of cognitive, psychosocial and behavioral abilities to assess for school readiness. Outpatient comprehensive evaluations will continue through the child’s transition to adulthood.
Our experienced neuropsychologists are trained to:
- Evaluate a wide range of cognitive skills and abilities and provide a detailed profile of your child’s cognitive strengths and weaknesses
- Assist with academic and vocational planning (e.g., attend IEP meetings, assist with guardianship planning and transition into adulthood)
- Help determine the most appropriate intervention services
- Provide recommendations for parents to implement within the home setting
Skills and abilities often tested include:
- Intelligence
- Memory
- Processing Speed
- Attention
- Language
- Executive Functions
- Visual Spatial Processing
- Fine-Motor Speed and Dexterity
- Adaptive Abilities
Developmental Screenings & Evaluations
Developmental evaluations are recommended from birth to identify potential developmental delays (motor, speech), learning and/or behavioral concerns during the different stages of childhood.
Infancy
- Within the first 3 months of life
- 6 months
- 9 months
- 12 months
Toddler (1 - 3 years of age)
- 18 months (1.5 years of age)
- 36 months ( 3 years of age)
Preschool (3 - 5 years of age)
School-Age (6+ years of age)
Neurology Evaluation
A neurologist will perform a neurological screening and work with the family to schedule follow-up visits. If necessary, the neurologist will provide recommendations for your child for physical, occupational or speech therapies.
Neuropsychological Assessments
If a developmental concern is identified, the patient will be referred to a comprehensive neurodevelopmental evaluation with a pediatric neuropsychologist. Evaluations can last between 90 minutes to three hours, depending on the child’s age.
Starting at age five, a neuropsychologist will perform comprehensive evaluations of cognitive, psychosocial and behavioral abilities to assess for school readiness. Outpatient comprehensive evaluations will continue through the child’s transition to adulthood.
Our experienced neuropsychologists are trained to:
- Evaluate a wide range of cognitive skills and abilities and provide a detailed profile of your child’s cognitive strengths and weaknesses
- Assist with academic and vocational planning (e.g., attend IEP meetings, assist with guardianship planning and transition into adulthood)
- Help determine the most appropriate intervention services
- Provide recommendations for parents to implement within the home setting
Skills and abilities often tested include:
- Intelligence
- Memory
- Processing Speed
- Attention
- Language
- Executive Functions
- Visual Spatial Processing
- Fine-Motor Speed and Dexterity
- Adaptive Abilities
Developmental Screenings & Evaluations
Developmental evaluations are recommended from birth to identify potential developmental delays (motor, speech), learning and/or behavioral concerns during the different stages of childhood.
Infancy
- Within the first 3 months of life
- 6 months
- 9 months
- 12 months
Toddler (1 - 3 years of age)
- 18 months (1.5 years of age)
- 36 months ( 3 years of age)
Preschool (3 - 5 years of age)
School-Age (6+ years of age)
Neurology Evaluation
A neurologist will perform a neurological screening and work with the family to schedule follow-up visits. If necessary, the neurologist will provide recommendations for your child for physical, occupational or speech therapies.
Neuropsychological Assessments
If a developmental concern is identified, the patient will be referred to a comprehensive neurodevelopmental evaluation with a pediatric neuropsychologist. Evaluations can last between 90 minutes to three hours, depending on the child’s age.
Starting at age five, a neuropsychologist will perform comprehensive evaluations of cognitive, psychosocial and behavioral abilities to assess for school readiness. Outpatient comprehensive evaluations will continue through the child’s transition to adulthood.
Our experienced neuropsychologists are trained to:
- Evaluate a wide range of cognitive skills and abilities and provide a detailed profile of your child’s cognitive strengths and weaknesses
- Assist with academic and vocational planning (e.g., attend IEP meetings, assist with guardianship planning and transition into adulthood)
- Help determine the most appropriate intervention services
- Provide recommendations for parents to implement within the home setting
Skills and abilities often tested include:
- Intelligence
- Memory
- Processing Speed
- Attention
- Language
- Executive Functions
- Visual Spatial Processing
- Fine-Motor Speed and Dexterity
- Adaptive Abilities
Family Resources
Having a child with complex heart disease can be stressful for the entire family. There is support available for families, children and young adults.
Self Care for Parents and Caregivers
One of the best ways a parent or caregiver can support is a child’s development is to take care of yourself as well
- Get plenty of rest and sleep when you are able to
- Eat a healthy, well balanced diet and drink lots of water
- Try to get some physical activity every day (go for a walk, exercise, yoga)
- Spend some time with positive support people in your life
- Journal about your experiences
Resources for Hospitalized Families
- Cardiac Social Worker: Denisse Valor, LCSW
- Child Life Specialist: Becky Pickard, M.S., CLSS
- Cardiac Psychologist: Dr. Silvia Sommers, PysD
- Chaplin/Pastor (Family Centered Care Services)
Online Resources
Counseling Services
Catholic Charities
- Provides family and individual counseling. Locations in West Palm Beach, Miami, and Fort Myers area.
Jewish Community Services of South Florida
- Provides counseling services and psychoeducational testing. Services available in English, Spanish, and Creole.
Family Resources
Having a child with complex heart disease can be stressful for the entire family. There is support available for families, children and young adults.
Self Care for Parents and Caregivers
One of the best ways a parent or caregiver can support is a child’s development is to take care of yourself as well
- Get plenty of rest and sleep when you are able to
- Eat a healthy, well balanced diet and drink lots of water
- Try to get some physical activity every day (go for a walk, exercise, yoga)
- Spend some time with positive support people in your life
- Journal about your experiences
Resources for Hospitalized Families
- Cardiac Social Worker: Denisse Valor, LCSW
- Child Life Specialist: Becky Pickard, M.S., CLSS
- Cardiac Psychologist: Dr. Silvia Sommers, PysD
- Chaplin/Pastor (Family Centered Care Services)
Online Resources
Counseling Services
Catholic Charities
- Provides family and individual counseling. Locations in West Palm Beach, Miami, and Fort Myers area.
Jewish Community Services of South Florida
- Provides counseling services and psychoeducational testing. Services available in English, Spanish, and Creole.
Family Resources
Having a child with complex heart disease can be stressful for the entire family. There is support available for families, children and young adults.
Self Care for Parents and Caregivers
One of the best ways a parent or caregiver can support is a child’s development is to take care of yourself as well
- Get plenty of rest and sleep when you are able to
- Eat a healthy, well balanced diet and drink lots of water
- Try to get some physical activity every day (go for a walk, exercise, yoga)
- Spend some time with positive support people in your life
- Journal about your experiences
Resources for Hospitalized Families
- Cardiac Social Worker: Denisse Valor, LCSW
- Child Life Specialist: Becky Pickard, M.S., CLSS
- Cardiac Psychologist: Dr. Silvia Sommers, PysD
- Chaplin/Pastor (Family Centered Care Services)
Online Resources
Counseling Services
Catholic Charities
- Provides family and individual counseling. Locations in West Palm Beach, Miami, and Fort Myers area.
Jewish Community Services of South Florida
- Provides counseling services and psychoeducational testing. Services available in English, Spanish, and Creole.
Request an EKG Screening
Please fill out the form to place your request.
2022 March 30
victoria-fierro-MD
JP
Abdominal Injury
2022 April 6
BenefitforBradley
2022 April 13
Luca heart fund
Graceston
2022 April 20
Mamava Lactation Pods
Nicklaus Children’s Hospital now features three Mamava lactation pods at its main campus near Coral Gables. The pods provide breastfeeding mothers with a private, clean, and comfortable space to pump or nurse their babies. The pods were funded through iGIVE, the employee-giving fund of Nicklaus Children’s Health System.
Mamava pods are powered by a smart technology system that enables easy location sharing, autonomous access, and remote monitoring through use of the free Mamava app available for iOS and Android. Designed specifically for pumping and breastfeeding, these pods feature easy-to-clean surfaces, comfortable benches and a locking door.

Campus Locations
- Emergency Department waiting room
- Advanced Pediatric Care Pavilion lobby
- Location adjoining the Central Building lobby
Employee Lactation Rooms
The funds from our employee giving program iGIVE have also provided lactation rooms for our employees. They are now available to breast-feeding parents on the main campus.

Leaders in Lactation
The International Board of Lactation Consultant Examiners® (IBLCE®) and International Lactation Consultant Association® (ILCA®) have recognized Nicklaus Children’s Hospital for excellence in lactation care. Nicklaus Children’s received the IBCLC Care Award in recognition of its commitment to staffing the hospital with professionals who hold the prestigious International Board Certified Lactation Consultant® (IBCLC®) certification and providing a lactation program for breastfeeding families.
About Mamava
Mamava, the leading expert in lactation space design, is dedicated to transforming the culture of breastfeeding in the United States by providing flexible lactation space solutions designed to meet the needs of breastfeeding families. Mamava pods are linked into a proprietary smart technology system that empowers easy wayfinding and autonomous access. Parents can open them with Mamava’s free app (available for iOS and Android). The app also allows moms to see availability of pods, opt into vacancy alerts, adjust interior lighting and airflow, and leave digital notes of support for the next person. Best of all, the app helps breastfeeding people find thousands of (Mamava-vetted) places to pump on the go—not just Mamava pods, and never a bathroom. To learn more, visit Mamava and follow on Twitter, Facebook, and Instagram. Additional B-roll and imagery available upon request.
SE Grocers Kickoff 2022
CulinaryExperience
2022 April 27
2022 May 4
Meditations
GI
2022 May 11
Thank you
Child Life Resources
Toy Guide for Children
The following are toys recommended to support the growth and development of children of varying ages and abilities.
Toy Guide
Comfort Positions for Children During Procedures
Comfort positions support positive coping for children during procedures. They give caregivers a role and decrease anxiety for children during hospitalizations.
Comfort Positions Guide
Developmental-Behavioral Home
carmen-bustamante-escobar-md
2022 May 18
Bioethics Program Home
Joanna-perdomo-md
Meet the Bioethics Program Team
The role of the Bioethics Program team is to:
- Familiarize the hospital staff and the greater community with ethical issues faced by parents, families, and healthcare providers engaged in the ongoing care of desperately ill children.
- Meet in special session to provide guidance and/or serve as a sounding board for parents, families, and healthcare professionals to discuss specific ethical concerns.
- Recommend and review hospital guidelines for ethical issues that arise related to the care of children.
Patient Resources
To schedule a first time evaluation with the rehabilitation services department, please call 877-255-8437.
For questions regarding insurance authorizations or to schedule an appointment for an established patient of the rehabilitation services department, please call the location where the patient is receiving treatment.
List of telephone numbers by location:
| Location |
Phone Number |
Extension |
| Main Campus (Hospital) |
(786) 268-1819 |
Ext. 1819 |
| Palmetto Bay |
(786) 624-3636 |
Ext. 3636 |
| West Kendall |
(305) 278-5973 |
Ext. 5973 |
| Pinecrest (Sports Health Center) |
(786) 624-5150 |
Ext. 5150 |
| Doral |
(786) 624-5286 |
Ext. 5286 |
| Miami Lakes |
(786) 313-7846 |
Ext. 7846 |
| Midtown (Nirvair Chowdhury) |
(305) 571-8770 |
Ext. 8770 |
| Miramar |
(954) 517-8936 |
Ext. 8936 |
| Weston |
(954) 385-6298 |
Ext. 6298 |
| Palm Beach Gardens |
(561) 799-7271 |
Ext. 7271 |
Your Child's Medical Records
Access portions of your child's medical record by accepting an email invitation to enroll in the MyKids Patient Portal. For access, email mykidsportal@nicklaushealth.org.
For medical records not available on the portal, please visit this the Health Information Management page.
Billing Inquiries
For billing inquiries, please call 305-663-8452 option 2 from Monday - Friday 8 a.m. - 4:30 p.m.
Accepted by Most Commercial Insurance Plans
Nicklaus Children's rehabilitative services are covered by most commercial insurance plans, including:
- Aetna (commercial)
- Ambetter
- AVMED – Non-par with Jackson Select (JHS/JRP), first choice, LFP Premier, Entrust (Avmed Federal Marketplace Plan)
- BCBS Florida and Out of State – Non-par W/ Blue Select (can be seen with out of network benefits ONLY)
- Cigna – Non-par with Federal Exchange & EPO CONNECT
- Golden Rule
- Humana HMO
- Medicaid of Florida
- Oxford
- Amerihealth Caritas Medicaid
- Sunshine Medicaid
- Tricare
- United Medicaid (only accepted depending on diagnosis)
- United Healthcare Commercial
- United Bind
- United Healthcare (Neighborhood Health Plan)
- UMR
- Vivida Health Plan
Medicaid Plans that Cover Treatment at Palm Beach Gardens Location Only:
- Community Care Plan Medicaid
- Simply Medicaid & Healthy Kids
- Humana Medicaid
2022 May 25
2022 June 1
2022 June 8
Request a Consultation
India
2022 June 15
Project ADAM
Cardiac emergencies are the leading cause of death in the United States and unfortunately the young are not excluded from this statistic. A focused effort on cardiac arrest preparedness in schools is critical to protecting our children and others in the community.
Project ADAM South Florida is committed to helping schools implement and sustain lifesaving training and education to school faculty and community organizations where young people are present.
What is Sudden Cardiac Arrest (SCA)?
Sudden cardiac arrest is the result of an abrupt loss of heart function that occurs when the electrical system to the heart beats rapidly from a dangerously fast rhythm in the bottom chambers of the heart muscle. This rhythm becomes too fast and irregular to support enough oxygenated blood to the brain and body, resulting in a sudden loss of consciousness. Cardiopulmonary resuscitation (CPR) is necessary to support blood flow to the brain and vital organs until the electrical rhythm can be restored with use of an automated external defibrillator (AED), to prevent sudden cardiac death.
What is Project ADAM?

The Nicklaus Children's Heart Institute is proud to be an affiliate of Project ADAM®, a non-profit organization whose mission is to serve children and adolescents through educational, life-saving programs that help prevent sudden cardiac arrest (SCA).
This program provides schools and community organizations the education and tools to develop and sustain their SCA response programs. Clinicians from the Nicklaus Children's Heart Institute provide hands-on training and education to schools who wish to become a part of the Project ADAM program.
Program Highlights
As an affiliate of Project ADAM®, we provide schools and organizations:
- Cardiopulmonary resuscitation (CPR) training/certifications for school staff, and coaches
- Training to ensure that staff responds quickly and efficiently to SCA event
- Practice drills to promote staff familiarity, rapid on site communication and practiced coordination with your team and local Emergency Medical Services
- Training on the use of automated external defibrillators (AEDs) to provide rapid defibrillation in the event of sudden cardiac arrest
- Collaborate with staff on the development of an emergency response plan
How to Become a Heart Safe School
Schools that have completed the Project ADAM training and Heart Safe School checklist, become eligible for a Heart Safe School certification. For more information on how to become a Heart Safe school, contact:
Project ADAM Namesake
Adam was a young athlete from Wisconsin who loved to play basketball and tennis. His life was cut short in an instant when he collapsed while playing basketball due to sudden cardiac arrest. His heart and soul lives on in the legacy of Project ADAM (Automated Defibrillators in Adam's Memory), which has reached schools across the country, and has been responsible for more than 200 lives saved.
Project ADAM
Cardiac emergencies are the leading cause of death in the United States and unfortunately the young are not excluded from this statistic. A focused effort on cardiac arrest preparedness in schools is critical to protecting our children and others in the community.
Project ADAM South Florida is committed to helping schools implement and sustain lifesaving training and education to school faculty and community organizations where young people are present.
What is Sudden Cardiac Arrest (SCA)?
Sudden cardiac arrest is the result of an abrupt loss of heart function that occurs when the electrical system to the heart beats rapidly from a dangerously fast rhythm in the bottom chambers of the heart muscle. This rhythm becomes too fast and irregular to support enough oxygenated blood to the brain and body, resulting in a sudden loss of consciousness. Cardiopulmonary resuscitation (CPR) is necessary to support blood flow to the brain and vital organs until the electrical rhythm can be restored with use of an automated external defibrillator (AED), to prevent sudden cardiac death.
What is Project ADAM?

The Nicklaus Children's Heart Institute is proud to be an affiliate of Project ADAM®, a non-profit organization whose mission is to serve children and adolescents through educational, life-saving programs that help prevent sudden cardiac arrest (SCA).
This program provides schools and community organizations the education and tools to develop and sustain their SCA response programs. Clinicians from the Nicklaus Children's Heart Institute provide hands-on training and education to schools who wish to become a part of the Project ADAM program.
Program Highlights
As an affiliate of Project ADAM®, we provide schools and organizations:
- Cardiopulmonary resuscitation (CPR) training/certifications for school staff, and coaches
- Training to ensure that staff responds quickly and efficiently to SCA event
- Practice drills to promote staff familiarity, rapid on site communication and practiced coordination with your team and local Emergency Medical Services
- Training on the use of automated external defibrillators (AEDs) to provide rapid defibrillation in the event of sudden cardiac arrest
- Collaborate with staff on the development of an emergency response plan
How to Become a Heart Safe School
Schools that have completed the Project ADAM training and Heart Safe School checklist, become eligible for a Heart Safe School certification. For more information on how to become a Heart Safe school, contact:
Project ADAM Namesake
Adam was a young athlete from Wisconsin who loved to play basketball and tennis. His life was cut short in an instant when he collapsed while playing basketball due to sudden cardiac arrest. His heart and soul lives on in the legacy of Project ADAM (Automated Defibrillators in Adam's Memory), which has reached schools across the country, and has been responsible for more than 200 lives saved.
Thank you
2022 June 22
Review-Dr-Dobrolet
2022 June 29
Roy
2022 July 6
Art on Our Campus
Thyroid and Endocrine Surgery Home
Thyroid and Endocrine Surgery Home
Specialist Programs and Centers
Pediatric Hematology Oncology Fellowship
Employee Service Awards RSVP
Please fill out the form to RSVP
If you're experiencing issues submitting this form, please make sure you're using Chrome and not Edge as your web browser.
Thank You
2022 July 13
2022 July 20
Conditions we Treat
2022 July 27
MarquezPOM
2022 August 3
ryan-halickman-cardiology
NCYA Yoga
gift planning
2022 August 10
Psychology Training Programs
Psychology Fellowship Program
Psychology Internship Program
Salaries & Benefits
2022 August 17
Press Archive
groundbreaking
2022 August 24
omar-beckett-md
Enya
2022 August 30
Gianna-Sarcoma
Educational Initiatives
ELSO Certification for Hospital Infantil San Vicente Fundación
A team of nine medical staff members from the integrated cardiovascular surgery team of Hospital Infantil San Vicente Fundación are becoming internationally ELSO certified with support from Nicklaus Children's and the GHI. This initiative will involve the development of a formal ECMO management protocol for pediatric critical congenital heart disease cases that develop potentially recoverable cardiogenic shock after corrective cardiac surgery. Nicklaus Children's plays a central role in the development and support of this ECMO training program, including providing the theoretical and practical knowledge needed to establish an effective ECMO program.
Medical Conferences
First Pediatric Global Health Congress, Cartagena, August 9-10, 2024
This is the first pediatric conference organized by Casa del Niño Children's Hospital, the main tertiary pediatric hospital of the Bolívar region and our key regional partner. The LPR Foundation is the main sponsor of the conference, including two speakers from Nicklaus Children’s Hospital taking part in the key scientific activities. Dr. Cristina Abuchaibe, NCH cardiologist, will speak about advances in prenatal CHD diagnostics, as well as optimizing pulse oximetry in CHD screening. Dr. Guillermo de Angulo, NCH oncologist, will speak about the early diagnosis of cancer in children and the use of immunotherapy in pediatric leukemia.
SCP Congreso Pediátrico del Caribe, Barranquilla - May 22-24, 2024
As part of our continued partnership with the Sociedad Colombiana de Pediatría, GHI sponsored Dr. Cristina Abuchaibe, cardiologist from Nicklaus Children’s Hospital, to speak at their regional conference about her experience in implementing a successful congenital heart disease program. This was an impactful opportunity to highlight the importance of newborn CHD screening with pediatric physicians from throughout the Caribe region.
First Pediatric Seminar in Carmen de Bolívar - Carmen del Bolívar, May 31, 2024
Casa del Niño Children's Hospital and Fundación Ser hosted the first pediatric seminar in Carmen del Bolívar, a more remote town several hours from Cartagena. The LPR Foundation sponsored the participation of 11 physicians from the Casa del Niño Children's Hospital to attend the event. This is part of a concerted effort to improve access to quality pediatric care beyond Cartagena to the furthest reaches of the region. Dr. Andrea Maggioni from Nicklaus Children’s Hospital’s Global Health Department and Dr. Ana Macias from the Global Health Initiative spoke about the importance of early implementation CHD screening. This was preceded by CHD training at the largest local hospital, Hospital Nuestra Señora del Carmen de Bolívar. Topics focused on mainly on infectious diseases as this region has some of the highest incidences in Colombia and Latin America, as well as Chagas, Leptospirosis, malnutrition, renal diseases and quality management.
FIU Global Health Consortium Conference – Cartagena, September 13-15, 2023
FIU partnered with SCP and the Pan-American Health Organization (PAHO) for the expansion their annual Global Health Conference of the Americas. This was FIU’s first conference post-pandemic, which highlighted the need to foster regional collaborations for developing recommendations that governments and healthcare organizations can implement to further protect their communities. Over 300 international public health experts from government, medical and academic backgrounds convened in Cartagena to discuss global health challenges that are expected to arise due to climate change. Topics covered at the conference included pandemic preparedness, advances in immunizations, nutrition (including displacement and food insecurity) and environmental health. GHI hosted three physician speakers from Nicklaus Children’s Hospital:
- Dr. Rani Gereige: Climate Change and Impact on Pediatric & Population Health.
- Dr. Hernandez-Trujillo: Healthcare Disparities in Allergy, Asthma, and Immunodeficiency in the Latino population: What Can Be Done.
- Dr. Marcos Mestre: Hospital Operations during the Pandemic: Lessons Learned and Preparing for the Future.
SCP 33º Congreso Nacional de Pediatría – Barranquilla, July 6-8, 2023
Organized by our partners, the Sociedad Colombiana de Pediatría (SCP), this is the largest pediatric conference in Colombia with more than 3,000 pediatric clinicians attending from throughout Latin America. Key strategic partners for this conference included the Florida International University (FIU) Department of Public Health, the Asociación de Pediatría de Latinoamérica (ALAPE), Asociación Española de Pediatría (AEP), Sociedad Latinoaméricana de Infectología Pediátrica. GHI hosted several NCH speakers at the conference covering a wide range of pediatric topics, including:
- Dr. Juan Bolívar: Syncope in the Adolescent Athlete: Diagnosis and Management
- Dr. Luis Caicedo: Eosinophilic esophagitis: Increasing Occurrence in Latin America
- Dr. Monica Payares: Hip Dysplasia - Early Diagnosis
- Dr. Lourdes Prieto: Innovations in Cardiac Congenital Disease Interventions
The Initiative also hosted a co-branded booth that proved to be popular with conference attendees and spread the word on the initiative’s CHD screening efforts to the medical community.
American Academy of Pediatrics National Conference – Oct. 4 - 7th, 2022
Dr. Ana Macías, GHI Medical Coordinator in Colombia, represented the initiative at the American Academy of Pediatrics National Conference in Anaheim, California by presenting GHI’s poster, “Colombia Global Health Initiative - CCHD Screening Implementation”.

XI Congreso Panamericano de Neonatología – Oct. 13 -15th, 2022
GHI sponsored the accommodations and airfare for Drs. Carolina Jiménez and Juan Jiménez, the leading neonatologists from our partner site, Hospital General de Medellín, to attend the XI Congreso Panamericano de Neonatología in Cartagena, Colombia. The neonatologists presented various scientific posters and benefitted from exposure to a wide variety of topics on neonatal care, including the latest medical advances and best practices.
31st Foro Internacional de la Organización de Excelencia en Salud - Oct. 19 - 21st, 2022
The OES is an organization established in 1991 whose mission is to improve the national and international healthcare quality through concerted efforts with local health service providers, insurers, universities, foundations, and the government. At their annual international conference in Cartagena, Dr. Andrea Maggioni and Dr. Luis Alberto Percy Nuñez, CEO of our local partner hospital, Casa del Niño, formally presented the GHI project and CHD poster, which helped further promote our efforts across Colombia.
VIII Simposio Internacional de Actualización en Pediatría, Cartagena - June 29 - July 2, 2022
Hosted by the Sociedad Colombiana de Pediatría (Pediatric Society of Colombia), this is the largest pediatric conference in Colombia. The Global Health Initiative participated with five speakers from Nicklaus Children’s Hospital covering a wide range of pediatric topics. The LPR Foundation also hosted a co-branded booth with NCH that proved to be very popular with conference attendees and effectively spread the word of our GHI efforts in CHD to the participating medical community.
Global Health Initiative Regional Conference, Cartagena - May 26, 2022
GHI hosted a regional conference in Cartagena for its collaborating sites in the Bolívar department to share data and connect on opportunities to improve access to CHD screenings in the region. As a result of the input and surveys completed during the sessions, GHI has implemented additional improvements that have had an immediate impact on increasing the percentage of births screened at each site. As of the end of July 2024, the GHI program is screening an impressive 46% of the total newborn population in Bolívar for CHD.

First Scientific Conference on Congenital Heart Disease – November 21, 2021
On November 17, 2021, the Global Health Initiative successfully hosted its first bilingual pediatric CHD conference at the Hotel Santa Clara in Cartagena, Colombia. The goal of this conference was to present current efforts by the initiative to expand newborn cardiac screening in Colombia, with the aim of sharing lessons learned and potential synergies with other experts that will further foster local and global efforts toward the early detection of congenital heart disease.

Left to Right: Dr. Marcos Mestre, SVP and Chief Medical Officer, Nicklaus Children’s Hospital; Dr. Andrea Maggioni, Director, Global Health; Lorena Perozo-Rocha, President and CEO, LPR Foundation; Lawrence DeGeorge, Director, LPR Foundation, Matt Love, CEO, Nicklaus Children’s Hospital.
First GHI Medical Conference, Barranquilla – May 2021
The Global Health Initiative hosted its first medical conference at the new LPR Foundation offices in Barranquilla, inviting physician leaders from the initiative's new active sites to share their feedback on the program and how to expand usage throughout the Atlántico region.
Educational Initiatives
ELSO Certification for Hospital Infantil San Vicente Fundación
A team of nine medical staff members from the integrated cardiovascular surgery team of Hospital Infantil San Vicente Fundación are becoming internationally ELSO certified with support from Nicklaus Children's and the GHI. This initiative will involve the development of a formal ECMO management protocol for pediatric critical congenital heart disease cases that develop potentially recoverable cardiogenic shock after corrective cardiac surgery. Nicklaus Children's plays a central role in the development and support of this ECMO training program, including providing the theoretical and practical knowledge needed to establish an effective ECMO program.
Medical Conferences
First Pediatric Global Health Congress, Cartagena, August 9-10, 2024
This is the first pediatric conference organized by Casa del Niño Children's Hospital, the main tertiary pediatric hospital of the Bolívar region and our key regional partner. The LPR Foundation is the main sponsor of the conference, including two speakers from Nicklaus Children’s Hospital taking part in the key scientific activities. Dr. Cristina Abuchaibe, NCH cardiologist, will speak about advances in prenatal CHD diagnostics, as well as optimizing pulse oximetry in CHD screening. Dr. Guillermo de Angulo, NCH oncologist, will speak about the early diagnosis of cancer in children and the use of immunotherapy in pediatric leukemia.
SCP Congreso Pediátrico del Caribe, Barranquilla - May 22-24, 2024
As part of our continued partnership with the Sociedad Colombiana de Pediatría, GHI sponsored Dr. Cristina Abuchaibe, cardiologist from Nicklaus Children’s Hospital, to speak at their regional conference about her experience in implementing a successful congenital heart disease program. This was an impactful opportunity to highlight the importance of newborn CHD screening with pediatric physicians from throughout the Caribe region.
First Pediatric Seminar in Carmen de Bolívar - Carmen del Bolívar, May 31, 2024
Casa del Niño Children's Hospital and Fundación Ser hosted the first pediatric seminar in Carmen del Bolívar, a more remote town several hours from Cartagena. The LPR Foundation sponsored the participation of 11 physicians from the Casa del Niño Children's Hospital to attend the event. This is part of a concerted effort to improve access to quality pediatric care beyond Cartagena to the furthest reaches of the region. Dr. Andrea Maggioni from Nicklaus Children’s Hospital’s Global Health Department and Dr. Ana Macias from the Global Health Initiative spoke about the importance of early implementation CHD screening. This was preceded by CHD training at the largest local hospital, Hospital Nuestra Señora del Carmen de Bolívar. Topics focused on mainly on infectious diseases as this region has some of the highest incidences in Colombia and Latin America, as well as Chagas, Leptospirosis, malnutrition, renal diseases and quality management.
FIU Global Health Consortium Conference – Cartagena, September 13-15, 2023
FIU partnered with SCP and the Pan-American Health Organization (PAHO) for the expansion their annual Global Health Conference of the Americas. This was FIU’s first conference post-pandemic, which highlighted the need to foster regional collaborations for developing recommendations that governments and healthcare organizations can implement to further protect their communities. Over 300 international public health experts from government, medical and academic backgrounds convened in Cartagena to discuss global health challenges that are expected to arise due to climate change. Topics covered at the conference included pandemic preparedness, advances in immunizations, nutrition (including displacement and food insecurity) and environmental health. GHI hosted three physician speakers from Nicklaus Children’s Hospital:
- Dr. Rani Gereige: Climate Change and Impact on Pediatric & Population Health.
- Dr. Hernandez-Trujillo: Healthcare Disparities in Allergy, Asthma, and Immunodeficiency in the Latino population: What Can Be Done.
- Dr. Marcos Mestre: Hospital Operations during the Pandemic: Lessons Learned and Preparing for the Future.
SCP 33º Congreso Nacional de Pediatría – Barranquilla, July 6-8, 2023
Organized by our partners, the Sociedad Colombiana de Pediatría (SCP), this is the largest pediatric conference in Colombia with more than 3,000 pediatric clinicians attending from throughout Latin America. Key strategic partners for this conference included the Florida International University (FIU) Department of Public Health, the Asociación de Pediatría de Latinoamérica (ALAPE), Asociación Española de Pediatría (AEP), Sociedad Latinoaméricana de Infectología Pediátrica. GHI hosted several NCH speakers at the conference covering a wide range of pediatric topics, including:
- Dr. Juan Bolívar: Syncope in the Adolescent Athlete: Diagnosis and Management
- Dr. Luis Caicedo: Eosinophilic esophagitis: Increasing Occurrence in Latin America
- Dr. Monica Payares: Hip Dysplasia - Early Diagnosis
- Dr. Lourdes Prieto: Innovations in Cardiac Congenital Disease Interventions
The Initiative also hosted a co-branded booth that proved to be popular with conference attendees and spread the word on the initiative’s CHD screening efforts to the medical community.
American Academy of Pediatrics National Conference – Oct. 4 - 7th, 2022
Dr. Ana Macías, GHI Medical Coordinator in Colombia, represented the initiative at the American Academy of Pediatrics National Conference in Anaheim, California by presenting GHI’s poster, “Colombia Global Health Initiative - CCHD Screening Implementation”.

XI Congreso Panamericano de Neonatología – Oct. 13 -15th, 2022
GHI sponsored the accommodations and airfare for Drs. Carolina Jiménez and Juan Jiménez, the leading neonatologists from our partner site, Hospital General de Medellín, to attend the XI Congreso Panamericano de Neonatología in Cartagena, Colombia. The neonatologists presented various scientific posters and benefitted from exposure to a wide variety of topics on neonatal care, including the latest medical advances and best practices.
31st Foro Internacional de la Organización de Excelencia en Salud - Oct. 19 - 21st, 2022
The OES is an organization established in 1991 whose mission is to improve the national and international healthcare quality through concerted efforts with local health service providers, insurers, universities, foundations, and the government. At their annual international conference in Cartagena, Dr. Andrea Maggioni and Dr. Luis Alberto Percy Nuñez, CEO of our local partner hospital, Casa del Niño, formally presented the GHI project and CHD poster, which helped further promote our efforts across Colombia.
VIII Simposio Internacional de Actualización en Pediatría, Cartagena - June 29 - July 2, 2022
Hosted by the Sociedad Colombiana de Pediatría (Pediatric Society of Colombia), this is the largest pediatric conference in Colombia. The Global Health Initiative participated with five speakers from Nicklaus Children’s Hospital covering a wide range of pediatric topics. The LPR Foundation also hosted a co-branded booth with NCH that proved to be very popular with conference attendees and effectively spread the word of our GHI efforts in CHD to the participating medical community.
Global Health Initiative Regional Conference, Cartagena - May 26, 2022
GHI hosted a regional conference in Cartagena for its collaborating sites in the Bolívar department to share data and connect on opportunities to improve access to CHD screenings in the region. As a result of the input and surveys completed during the sessions, GHI has implemented additional improvements that have had an immediate impact on increasing the percentage of births screened at each site. As of the end of July 2024, the GHI program is screening an impressive 46% of the total newborn population in Bolívar for CHD.

First Scientific Conference on Congenital Heart Disease – November 21, 2021
On November 17, 2021, the Global Health Initiative successfully hosted its first bilingual pediatric CHD conference at the Hotel Santa Clara in Cartagena, Colombia. The goal of this conference was to present current efforts by the initiative to expand newborn cardiac screening in Colombia, with the aim of sharing lessons learned and potential synergies with other experts that will further foster local and global efforts toward the early detection of congenital heart disease.

Left to Right: Dr. Marcos Mestre, SVP and Chief Medical Officer, Nicklaus Children’s Hospital; Dr. Andrea Maggioni, Director, Global Health; Lorena Perozo-Rocha, President and CEO, LPR Foundation; Lawrence DeGeorge, Director, LPR Foundation, Matt Love, CEO, Nicklaus Children’s Hospital.
First GHI Medical Conference, Barranquilla – May 2021
The Global Health Initiative hosted its first medical conference at the new LPR Foundation offices in Barranquilla, inviting physician leaders from the initiative's new active sites to share their feedback on the program and how to expand usage throughout the Atlántico region.
Meet the Team
Meet the Team
GHI Home
GHI Home
Physician Appointment Request
2022 September 8
2022 September 14
stephanie-acosta-cardiology
2022 September 21
dana-decarlo-cardiology
2022 September 28
Nurse Scholars Program
Nicklaus Children's Hospital has partnered with local affiliates to offer funding for students accepted to their nursing programs.
Students may apply for an award toward their tuition in return for their work commitments at Nicklaus Children's Hospital.
Program Details
Miami Dade College
Thank you for your interest in the MDC Nurse Scholars Program.
At this time, we are not opening applications for Spring 2025.
Students accepted to the Generic Associate of Science in Nursing (ASN) program at Miami Dade College may apply for the Nicklaus Children's Nurse Scholars Program. The program consists of four semesters of didactic and clinical experiences as a student and Student Nurse Intern (SNIP). Up to 10 participants will be accepted during each fall and spring semester.
Florida International University
Students accepted to the Generic Bachelor of Science in Nursing (BSN) program at Florida International University may apply for the Nicklaus Children's Nurse Scholars Program. The program consists of five semesters of didactic and clinical experiences as a student and Student Nurse Intern (SNIP). Up to 10 participants will be accepted during each fall and spring semester.
Program Requirements
The SNIP is a per-diem employment opportunity for nurse scholars to be hired as care assistants to gain insight into the field of pediatric nursing. The pediatric and practicum experiences will be completed within Nicklaus Children's Hospital.
Students accepted into the Nicklaus Children's Nurse Scholars Program are provided with an award toward their school tuition. Tuition payments are made directly to the school, and nurse scholars are responsible for additional fees applied by the school.
After completion of the program, eligible graduates may be offered employment into the Horizon Nurse Residency program, which will figure a 2-year work commitment with Nicklaus Children's Hospital.
*If attending the ASN program at Miami Dade College, and hired as a Horizon RN, the graduating nurse scholar will be required to complete the RN to BSN program within a specific timeframe post hire.
How to Apply
All applications are facilitated through Edcor Data Services, LLC.
Go to Application
Dental Mobile Unit
Oliver POM
Patient Stories
2022 October 5
alejandro-martinez-herrada-cardiac-critical-care
/lauren-pronman-clinical-genetics-metabolism
ana-rodriguez-barreto-clinical-genetics-metabolism
2022 October 12
2022 October 19
CME Home
shanna-kowalsky-herbst-infectious-diseases
shruti-bassi-pediatric-anesthesiology
raul-fernandez-torrealba-pediatric-anesthesiology
aimee-gasior-bejar-pediatric-anesthesiology
nelson-riveros-perez-pediatric-anesthesiology
rafael-gonzalez-pediatric-anesthesiology
richard-lagueruela-pediatric-anesthesiology
debera-hui-pediatric-anesthesiology
sandra-rivera-luciano-general-pediatrics
stephanie-montarroyos-general-pediatrics
carla-barreau-general-pediatrics
Michael Fux Holiday Media Consent
Frequently Asked Questions
Click to expand
What is the Michael Fux Foundation?
The Michael Fux Foundation believes we, as a community, can overcome the challenges and isolation that families experience who care for a sick child. Together, we can cultivate a community that transcends racial and socioeconomic barriers as we focus on the care and well-being of the child and their family. This builds a wealth of human connections that are permanently linked by unconditional love and support.
What will my family & I do at the Michael Fux Foundation Holiday Event?
This outdoor event will have games, shows, face painting, balloon art, activities, music, food and a very special surprise visit.
What should my family and I wear?
We ask all members of the family to dress comfortably & accordingly to the weather as the event is held outdoors on the main hospital's campus.
Who can attend the party?
Seating is limited at the event. Only the guardians, patient and patient's siblings that were invited, will be able to attend. The names of each family member invited will be at the registration tables.
Are the toy wishes guaranteed?
The Michael Fux Foundation likes to be fair and consider all families attending when reviewing toy wishes. The Foundation tries its best to make your child's experience as personalized as possible. We use the toy wish lists to understand your child's interests, however, toy wishes are not guaranteed.
What do I do if I we need transportation or can't attend the party?
If transportation is a concern, we would be happy to accommodate transportation to and from the event. Please notify us If you are in need of transportation or are not able to attend the party.
If I have other questions, who should I contact?
Michael Fux Family Center at 305-663-8500.
Please fill in the media consent and waiver below.
Leer y llenar este formulario en español.
Thank You
2022 October 26
Surgical Tower
PETALS Recognition Program
PETALS are: Professional Extraordinaires That Always Lend Support
Every DAISY has petals extending from its core that make it a perfect flower. At Nicklaus Children’s Hospital, our PETALS are Nursing’s colleagues in departments such as Environmental Services, Case Management, Rehabilitation, Food and Nutrition, and Transport, as well as unit coordinators, behavioral health techs, nurse assistants, physicians and other employees throughout the health system. Please help the Department of Nursing recognize these individuals for the outstanding and compassionate care they deliver every day.

2022 November 2
wifiinfo
2022 November 9
FAC Membership
Thank you for your interest in joining the Family Advisory Council (FAC). Please fill out the form below to apply for membership. Ver en español.
Thank You
Please know Council membership requires successful completion of the application process, including but not limited to: interview, a health screening which includes TB questionnaire, flu vaccine (waiver option available), Convid-19 vaccine, criminal background check and an orientation.
If you have any questions, please contact Angel Sepulveda, Manager, Service Excellence, at 786-624-4435 or via email at angel.sepulveda@nicklaushealth.org
Family-Centered Care Services Home
Children's & Family Experiences Home
Child Life
2022 November 16
2022 November 23
/rene-lopez-guerrero-general-pediatrics
Daniel
PPGCPIP
2022 November 30
Review-Dr-Ruggles
/jonanlis-ramirez-alcantara-endocrinology
MichaelFuxHolidayParty
Observer Programs
The Observer Programs provide educational opportunities for members of the communities we serve, with the goal of increasing the number of future medical and healthcare professionals. Nicklaus Children's Hospital will consider requests from qualified applicants wishing to take part of our Observer Programs. International observer requests are NOT accepted at this time.
Teen Observer Program
This program provides teens who are in their junior or senior year in high school with the opportunity to observe a clinical staff member for the purpose of gaining knowledge and experience in a health care setting.
Program Details
- Applicants must be at least 16 years old by the start of the Program. Teen Observer opportunities will be honored during summer months only (June-August).
- Teen Observers Applicants must arrange to observe directly with a sponsoring clinician/individual before applying to the Program.*
General Observer Program
This program provides educational opportunities for members of the communities we serve, with the goal of increasing the number of future medical and healthcare professionals.
Program Details
- Applicants must be at least 16 years old by the start of the Program.
- Applicants must arrange to observe directly with a sponsoring clinician/individual before applying to the Program.*
Observation experiences will not be honored to pre-medical or medical students,
residents or physician observation requests.
*The Learning and Development department is not able to match participants with clinicians.
mckay-mckinnon-plastic-surgery
Adaptive Care Home
Social Narratives
Diagnostics and Treatments
West Broward Dancemarathon 23
2022 December 7
Kateryna
Videos
Patient Resources
The Inflammatory Bowel Disease (IBD) Center, within the Division of Gastroenterology at Nicklaus Children's Hospital, provides comprehensive support and management for children and young adults with Crohn's disease and ulcerative colitis.
The goal is to support children with IBD in attaining remission and optimizing quality of life.
Download Bilingual PDF Booklet
What are Crohn's and Ulcerative Colitis?
- Crohn's disease is a chronic inflammatory bowel disease that affects the lining of the digestive tract anywhere from the mouth to rectum. Crohn's disease can cause abdominal pain, diarrhea, weight loss, anemia and fatigue.
- Ulcerative colitis is a chronic, inflammatory bowel disease that causes inflammation in the lining of the large intestine. Symptoms include rectal bleeding, bloody diarrhea, abdominal cramps and pain.
- The IBD Center at Nicklaus Children's brings together a comprehensive team of experts to support patients and their families in the care journey. The entire team takes part in clinical management to enable your children and young adults to benefit from multispecialty collaboration and consultation. Specialists who collaborate within the IBD Center at Nicklaus Children's include nutritionists, behavioral medicine/ psychologists, pain management experts, child life specialists, social workers and pediatric surgeons.
As part of the comprehensive evaluation, your doctor may prescribe any of the following tests:
- Blood work/laboratory testing: These can include comprehensive metabolic blood panels, vitamin, D, hepatitis B, complete blood count (CBC), C-reactive protein (CRP), liver function, Epstein Barr Virus reactive and quantiferon.
- Skin testing: A skin test, also known as PPD test, may be performed to check for tuberculosis infection.
- Stool collection: Stool tests, including a gastrointestinal panel (GI panel) and cal protein, are important in the diagnosis and monitoring of inflammatory bowel disease.
Radiological Tests
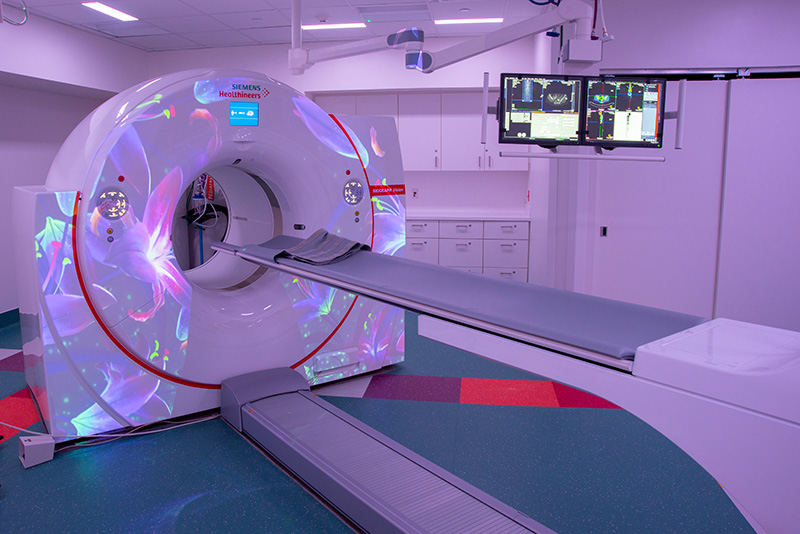
Magnetic resonance imaging (MRI) is an imaging test that provides detailed pictures of the small intestine. Patients may not be able to eat or drink six hours prior to this exam. During this exam, the patient will need to drink a liquid, called oral contrast, and will be asked to walk around so that the contrast can move through the intestines.

Computerized tomography (CT) is a type of imaging scan that takes detailed pictures of the intestine. The patient will drink a liquid (contrast) that allows the doctors to view inside the small intestine. The patient will not be able to eat or drink for 6 to 8 hours before this exam.
The following procedures may also be performed as part of the comprehensive evaluation:
- Esophagogastroduodenoscopy (EGD) with biopsy: This procedure provides the care team with a close up view of the gastrointestinal tract. A flexible tube with a camera on the tip is inserted through the esophagus and is used to view and collect samples of the gastrointestinal tract.
- Capsule endoscopy: During this procedure, a tiny wireless camera takes pictures as is passes through the small intestine. Images are recorded and stored in a device that is worn as a belt around the waist. The care team will remove the belt the next day.
- Colonoscopy with biopsy: This procedure uses a flexible tube with a camera to take images and samples of the bowels. To prepare for this test, the doctor may prescribe stool softeners, enemas and suppositories. For patients who are unable to drink by mouth, a nasogastric tube may be placed through the nose to administer the medications.
Daily Monitoring and Testing
Together with the care team, patients will be monitoring and tracking their food intake, as well as urine and bowel movements, as part of the comprehensive inpatient evaluation. The care team will work with the patient family to gather information such as:
- Daily weight monitoring will be performed before breakfast.
- Food and liquid intake (for children who are able to eat).
- Urine and stool output. The care team will provide families with a special “hat” to place on toilet rim to help collect specimens.
- The care team may place the patient under contact precautions which means the child may not be able to leave the room, room (unless it is for a procedure), until test results are returned and are negative. This can take between 48 to 72 hours).
- Some children will have an intravenous line (IV) to receive fluids for hydration.
- Your doctor may prescribe a bowel rest to give the child's digestive system a break from eating food by mouth. Patients on bowel rest will receive a peripherally inserted central catheter line (PICC) to receive nutrition, called total parenteral nutrition (tpn) and lipids (healthy fats). The PICC line typically stays in place longer than an IV and avoids the need for multiple IV placements. Some patients can have the PICC line placed at the bedside, while others may need to have it placed under anesthesia in the minor procedures suite.
- The doctor may request blood samples to monitor the child's electrolytes, triglycerides, and liver functions. Routine bloodwork can also be drawn from the PICC line.
- Some patients may be able to drink meal replacement shakes. These can be taken by mouth or through a nasogastric tube (NGT).
Diet
If the child can eat by mouth, a dietician will meet with the family to provide information on the types of foods the patient may consume. Dietary modifications may consist of following a low-fiber, low-lactose and/or a sugar-free diet. Families should follow the dietician's recommendations exactly as they are prescribed as this is a critical component of managing IBD.
Medications
Your doctor will discuss which medications or combinations of medications are best for your child.
- Steroids (methylpredinosolone) may be administered through the IV during the hospital stay. Your care team will begin to slowly transition the patient from IV to oral steroids (prednisone). In many cases, diet therapy may replace the need for steroids.
- Your doctor may also prescribe anti-inflammatory medications. They come in the form of oral medications, enemas, suppositories and rectal injectable foams (Mesalmine).
- During the hospital stay, some patients may also begin to receive immunosuppressive medications. These can be administered through IV infusions while others are given through injections. Your doctor will discuss options that best meet your needs.
- A special medication to reduce inflammation and calm the immune system, called methotrexate, may be prescribed, based on the patient's needs. This medication can be taken orally or as an injection.
Supplements
Your doctor will discuss supplements to support your child's individual needs. These may include vitamin D, iron, magnesium and folic acid.
Follow-Up Care
- Patients will have routine bloodwork performed until medication blood levels are within therapeutic range.
- Children will be required to have bloodwork annually to check their vitamin levels and other important factors including quantiferon.
- Stool collections and procedures to monitor the digestive tract and colon will also be prescribed, as needed. • Patients will be referred to a clinical dietician to support the child with his/her dietary needs. Routine imaging, via magnetic resonance imaging (MRI) or CT scan, will be prescribed by your gastroenterologist.
- Routine procedures, including EDGs and/or colonoscopies, may also be be prescribed.
Community Resources
Contact a Member of the Care Team
To reach a member of the Inflammatory Bowel Disease Center or to schedule an appointment please call 786-624-2546.
2022 December 14
Nursing Professional Practice Model Home
2022 December 21
2022 December 28
/sarcoma-solid-tumor-program
Review-Dr-Ramchandran
Review-Dr-Wright
Review-Dr-Saldana
Chat with a Billing Representative
wifi
Test Password
Patient and Family Resources Home
katharine-button-emergency-medicine
Meet the Team
Pediatric Neurocritical Care Fellowship
Leo POM
NCPS Directory
NCPS Specialists in Broward County
AHSDM23
CBHSDM23
FIUDM23
MSDDM23
MHSDM23
PPCSDM23
STADM23
WBHSDM23
Thank You
Physician Appreciation Reception RSVP
RSVP for the Physician Appreciation Reception hosted by Nicklaus Children’s Hospital
Thank you for your interest in the Physician Appreciation Reception, registration is now closed.
We hope you will be able to join us for future events.
Thank You
Cerebral Palsy and Spasticity RSVP
RSVP for Management of Cerebral Palsy & Spasticity at Nicklaus Children's Hospital
Wednesday, March 20 at 6:30 P.M.
The Brain Institute at Nicklaus Children’s Hospital presents an online educational presentation
on the Management of Cerebral Palsy and Spasticity.
Featured Speakers
Toba Niazi, MD
Medical Director of Neuro-Oncology Surgical Services
Nicklaus Children’s Hospital
Migvis Monduy, MD
Pediatric Neurologist Director of Neuromuscular and Movement Disorders Programs
Nicklaus Children’s Hospital
and
Monica Payares-Lizano, MD
Program Director, Cerebral Palsy and Spasticity Program
Nicklaus Children’s Hospital
Thank You
/melanie-suaris-general-pediatrics
DonorAdvisedFund
Dan Marino Center
Review-Dr-Martinez-Fernandez
Review-Dr-Acosta
Review-Dr-Adlakha
Review-Dr-DeCarlo
Review-Dr-Garmany
/Review-Dr-Halickman
Review-Dr-Abdulkarim
Review-Dr-Martinez-Herrada
Review-Dr-Duarte-Caceres
MyNicklaus
Simple Linear Skull Fracture
Patient Safety Awareness Week

Patient Safety Awareness Week
Patient Safety Awareness Week is an annual recognition event intended to encourage everyone to learn more about health care safety. During this week, the Institute for Healthcare Improvement (IHI) seeks to advance important discussions locally and globally and inspire action to improve the safety of the health care system – for patients and the workforce.
Click here for resources from IHI to help organize facility level activities for Patient Safety Awareness Week.
Activities
?width=453&height=255)
Zoom / Teams Background
(click image to download)

Humpty Dumpty Fall Prevention Tips
(click image to download bi-lingual flyer)
Complimentary On-Demand Webinars
Webinar Schedule
Learn More About Patient Safety at Nicklaus Children's Hospital
Infant Safe Sleep
Following Safe Sleep practices is a way to keep your baby safe while sleeping. Infants are safest when they sleep in their own crib, bassinet, or portable crib. Sometimes, healthy infants can unexpectedly die if they are placed in an unsafe sleep environment.

To create a safe sleep environment for your baby, follow these steps every night and during naptime:
- Always lay your baby to sleep on their back during naps and night time
- Place your baby to sleep in a safety-approved crib with a firm sleep surface. Cover mattress with a tight fitted sheet
- To avoid suffocation or entrapment, keep soft objects (ex: pillows, loose blankets, bumpers) out of the baby's sleeping area
- Do not allow your baby to sleep in an adult bed, couch, or chair, alone, with you, or with anyone else.
- Keep your baby's crib in the same room you sleep in for the first year of life. Room sharing is recommended NOT bed sharing
- Seating devices (ex: bouncy seats, swings, infant carriers, strollers) should not be used for routine sleep. Wedges and positioners should not be used
- Do not smoke during pregnancy or allow your baby to be exposed to smoke
- Do not allow your baby to get too hot while sleeping. Avoid over-bundling and covering the baby's face should be avoided
- Breastfeeding is recommended
- Allow your baby a dry pacifier (not attached to a string or clip) during sleep times
- Do not fall asleep while holding your baby
- Follow healthcare provider's guidelines for health checkups and vaccine administration
- Tell anyone who cares for your baby to follow these safe sleep practices
Remember the ABC's of Safe Sleep!
Alone
On the Back
In a Crib
CMNRSVP
CMNTOURS
Lecture
Review-Dr-Perdomo
Review-Dr-Suaris
Review-Dr-Monte-Fernandez
Review-Dr-Handal-Saca
Review-Dr-Chiriboga
Review-Dr-Frias
PsychologyFellowship
FAC Home
Meet the Members
Events & Meetings
Monthly Meeting
2nd Tuesday of the month (10 times a year)
6:30 pm - 8:00 pm
via Teams and some in person
Contact Us
Diamond Ball Special
Fabricio
COVID-19 Vaccines
The COVID-19 vaccine is available for adults and children through a variety of sources in our community. The link below can help you find locations near you. In addition, pharmacy chains, including CVS, Publix and Walgreens, also offer the vaccine. Please check the website of the pharmacy of your choice for more information.
Click here for a link to the Miami-Dade County COVID-19 Vaccine Locator
How You Can Help
Planning Your Visit to the Hospital
Points of Entrance to the Hospital
Resources For Your Family
Talking to Your Children About COVID-19
Not sure how to address COVID-19 with your children? Our Department of Psychology developed this informational flyer to help families manage feelings about stress and anxiety.
Download the Flyer (PDF)
Download the COVID-19 Coloring Book from Children's Hospital of Richmond at VCA
Do your children have questions about COVID-19? Children's Hospital of Richmond at VCU has developed this kid-friendly coloring book filled with factual and fun activities designed to inform kids about COVID-19.
Download the coloring book (PDF)
Do your part and be a health hero!
Let’s continue to protect ourselves, our family and those in our community by wearing a face covering when out in public spaces!
COVID-19 Behavioral Health App
Cincinnati Children’s Hospital and the University of Cincinnati worked in collaboration to develop a behavioral health app for COVID-19.
Learn more about the app
About us
Undiagnosed Disease Clinic Home
Chemotherapy Course Registration
Please complete the following form to register. You will be directed to online payment after completing the registration.
Payment
Click the button to pay with credit card. You will be re-directed to Authorize.net checkout.
For group rates, contact Kristen Mendez.
Local Participants - $300
Includes a NEW Pediatric Chemotherapy and Biotherapy Curriculum book (required for the course). The books hold a special code that will be used to access your provider test at the end of the course, therefore you are unable to use a used book. The book will need to be picked up prior to the class at Nicklaus Children's Hospital (3100 SW 62 Ave, Miami, FL 33155).
Non-local registration - $200
Book not included.
You will need to purchase the book directly from APHON and have it delivered to you prior to our class. Please do this ASAP to ensure you receive the book prior to the course.
Employee Referral
Employee Referral Program
Monthly Prize: $200 Amazon Gift Card
If the candidate is hired, Nicklaus Children's Health System may offer a bonus for
successfully referring candidates for hard-to-fill positions.
All referrals must be submitted prior to interview.

The Employee & Leader Referral Program is designed to provide a cash incentive to all NCHS employees and leaders who refer a candidate for any of the vacant positions on the employee referral list for “Hard to recruit positions and high volume roles".
Staff Referrals: To qualify for a referral bonus, you must complete the form before the candidate is hired and have the candidate include your name under the “referred by" in his/her application. TM&E will acknowledge the referral once a form is submitted via the online portal form and they will be processed in the order they are received. For candidates referred by more than one employee, the bonus will be awarded to the employee whose referral was received first. Referral bonuses are subject to all applicable taxes.
Leader Referrals: To qualify for the leader referral bonus, you must complete the form before the candidate is hired and have the candidate include your name under the “referred by" in his/her application. All leaders of Nicklaus Children's Health System (Supervisor, Manager & Director level) are eligible to participate in the program with the exception of TM&E Department, Talent Managers and VPs. TM&E will acknowledge the referral once a form is submitted via the online portal form and they will be processed in the ordered they are received. For candidates referred by more than one employee/leader, the bonus will be awarded to the employee/leader whose referral was received first. Leaders will be eligible for 50 % of the amounts for staff referral program. Leaders who refer a candidate for their own department (or within their span of control) do not qualify for the bonus. Referral bonuses are subject to all applicable taxes.
The following applicants are not eligible to participate: re-hires who left less than 24 months ago, candidates whose applications/resume have been entered into the database via any sources within the last six (6) months; persons who have been referred by employment agencies, candidates who are referred as a result of NCHS-sponsored sourcing events such as job fairs, advertising and college recruitment and recent graduates (i.e. with less than one year of experience). The referral program also excludes referrals for Per Diem, Staff Relief, Pool positions unless otherwise specified.
Meet the Team
We're proud to be a leader in orthopedic services, specializing in sports injuries and general pediatric orthopedics and surgery. The pediatric orthopedic specialists at Nicklaus Children's also specialize in diagnosing scoliosis of the spine and performing scoliosis surgery. Our orthopedic experts are dedicated to supporting the treatment and prevention of injuries in children and adolescents.
Meet the Team
The team includes the spine surgical team’s highly experienced board-certified orthopedic surgeons who perform spinal surgery in children, advanced practice professionals, dedicated spine-trained anesthesiologists and a PhD neurophysiologist who monitors the spinal cord and nerve function throughout surgery.
Dedicated spine nurses, technicians, and radiology technicians complete the spinal surgical team. The surgical nurses are experts in the care of spinal surgery patients, managing six to eight patients per week.
Meet the Team
The team includes the spine surgical team’s highly experienced board-certified orthopedic surgeons who perform spinal surgery in children, advanced practice professionals, dedicated spine-trained anesthesiologists and a PhD neurophysiologist who monitors the spinal cord and nerve function throughout surgery.
Dedicated spine nurses, technicians, and radiology technicians complete the spinal surgical team. The surgical nurses are experts in the care of spinal surgery patients, managing six to eight patients per week.
Special Event Agreement Application
Contact Us
LifeFlight Survey
LifeFlight® Customer Satisfaction Survey
RSVP BWS Conference Registration
Thank you
Webinar
Contact the Department
Contact the Department
Contact the Department
Contact the Department
Meet the Team
Our neurosurgery team works with other pediatric specialists at Nicklaus Children’s to establish an accurate diagnosis, develop a specialized treatment plan and provide comprehensive treatment to all patients. Our renowned pediatric neurosurgeons are recognized for excellence among their peers based upon their surgical expertise, their numerous publications in textbooks and peer-reviewed journals, and their lectures both nationally and internationally.
wilson-heredia-nunez-neurology
NICU TeleConsult
Resources and Training Materials Listed by Organizations
Click on the organization's name to view info, documents, and videos.
Clarus Care (Paging)
Clarus Care is the paging solution that affiliate hospitals will use to submit requests for consults.
Login Link
Clarus Care (Paging)
If you have trouble logging in to Clarus, or need your login information, please contact:
- Clarus 24/7 Support line: (615) 375-4500
- Telehealth team (available Monday-Friday from 8:00am-4:30pm, excluding holidays) via email: Telehealth.Office@nicklaushealth.org
- Your Practice Administrator
Support/Contacts
Onboarding/Getting Started
Training
Baptist Health
Login Link
Baptist EMR - Cerner
Support/Contacts
For support with EMR documentation, email the Medical Informatics Team at MedicalInformatics@baptisthealth.net
To reset your Baptist EHR password online, visit Password Reset
- Baptist Help Desk - Provider 24/7 Support Number: (833) 764-2156
- Press 1 - Provider Password resets, Remote Access, Multi-factor Authentication or Hardware Issues
- Press 2 - All other issues + Office Staff and Scribes
- Email: DGTDEHRSustainment@baptisthealth.net
Note: Baptist teleconsults will occur via Zoom, between the Baptist neonatologist and NCH affiliated subspecialist.
Onboarding/Getting Started
Training modules must be completed in CME prior to receiving access. Start with Accessing Cerner EHR Training PDF document for instructions in the Training section below.
After you have been credentialed & completed training, please contact the EHR Sustainment Team to set up your remote Cerner access and Cerner Apps: Powerchart, Secure Messaging and Camera Capture. Refer to the support contact information above.
Remote Access Setup Instructions - Remote Access Setup Instructions
Training
All of Baptist's Training Videos/Modules are available via the CME platform. Consulting physicians can take the 'Consultant Module' courses listed below.
Files
HCA Healthcare
Login Links
HCA Remote Access
HCA's Telehealth - Teladoc (InTouch)
Support/Contacts
Meditech
For support with HCA's EMR/Meditech, contact the Provider Solutions Specialist (PSS) Team at (888) 561-6599.
For password resets or other issues accessing the EMR, contact HCA's 24/7 Help Desk at (888) 561-6599.
Teledoc
For support with HCA's Telehealth system, contact Teladoc's Technical Assistance Center at (877) 484-9119.
The Teladoc Health Telehealth Network is supported 24/7 and can also be reached via email at Email: TAC@TeladocHealth.com and by Teladoc Live Chat
Onboarding/Getting Started
For initial onboarding and training, please complete the following steps after you have been credentialed with HCA.
- Validate your EMR/Meditech system access by following the Remote Access Setup steps (only requires to be set up one time). Meditech log-in credentials are provided after completion of HCA's Meditech training. - HCA Remote Access Setup (VDI) file on site currently under Files section.
- Teladoc will send providers a welcome letter via email. Access the email from Teladoc which includes your unique Teladoc username and a link to Reset your Password.
- Access the Software Center to download the Teladoc software on your computer - HCA Teladoc Software Download
- Validate your ability to access Teladoc with the provided username and your newly reset password - https://portal.intouchcustomer.com/
- Review all of the training files/videos linked in the subsection below
Training
EMR/Meditech - Files
Note: To access PatientKeeper, go to Meditech and click on the icon for PatientKeeper.
EMR/Meditech - Video Tutorials
Teladoc/InTouch - Files
Teladoc Training Video
Mount Sinai Medical Center
Login Link
EMR - Epic SinaiLink
Support/Contact
For support with your Login ID, password resets, or other login issues, contact the Mount Sinai Service Desk at 305-674-2545.
For support with the Epic SinaiLink EMR, contact Mount Sinai's Clinical Informatics team at 305-674-2638.
Onboarding/Getting Started
For initial onboarding and training, please:
- Review the Epic Sinai Link Consult Note Workflow Tip Sheet
- Watch the Epic Sinai Link Consult Training Video
- Log in to Epic - Physicians received an email from Mount Sinai. The email includes a link, personal Login ID (your 4-digit code), and temporary password: Welcome1234!. You will be prompted to change the password. The Mount Sinai link is https://sinailink.msmc.com
Note: Mount Sinai is a Telephone (audio-only) consultation service, between the Mount Sinai neonatologist and NCH affiliated subspecialist.
Files
Wellington Regional Medical Center
Login Link
Wellington's EMR - Cerner
Support/Contacts
- For support with Wellington’s EMR, contact their Clinical Informatics team at (561) 798-8693 or via email at Wellington.IS@uhsinc.com
- For support with Wellington’s Telehealth system, contact (561) 472-2501 or email Wellington.IS@uhsinc.com
- For urgent after-hours support, please contact the Facility night supervisor at (561) 798-8625.
- For password resets or any other support, contact Wellington’s Help Desk at (561) 798-5622.
Onboarding/Getting Started
For initial onboarding and training, please:
- Follow the Citrix Installation Link & Instructions. Supported browsers for the EMR system are Google Chrome or Microsoft Edge.
- Validate your EMR system access by following the instructions in this file: Cerner-Fusion Login 2-Factor Authenticator Tip Sheet
Note: Wellington teleconsults will occur via Zoom between the Wellington neonatologist and NCH affiliated subspecialist.
Files
For support regarding the overall NICU TeleConsult program, credentialing, and other inquiries,
contact the NCHS Telehealth team via email at Telehealth.Office@nicklaushealth.org
mobileapp-eula
Mobile Application EULA
EFFECTIVE: 1 MARCH 2023
YOU SHOULD READ CAREFULLY THE FOLLOWING TERMS AND CONDITIONS BEFORE UTILIZING THE APPLICATION. BY INSTALLING AND UTILIZING THE APPLICATION YOU ACKNOWLEDGE YOUR ACCEPTANCE OF THE TERMS AND CONDITIONS OF THIS APPLICATION EULA (“AGREEMENT”). IF YOU DO NOT AGREE TO THE TERMS AND CONDITIONS OF THIS AGREEMENT, THEN DO NOT UTILIZE THE APPLICATION.
VARIETY CHILDREN’S HOSPITAL (dba NICKLAUS CHILDREN’S HOSPITAL) OFFERS THIS SOFTWARE PLATFORM (THE “APPLICATION”) PURELY FOR ENTERTAINMENT PURPOSES. THIS APPLICATION IS NOT INTENDED OR IS TO BE CONSIDERED FOR ANY CLINICAL PURPOSES OR PATIENT CARE. THE APPLICATION IS NOT A MEDICAL DEVICE AND SHOULD NOT BE RELIED UPON FOR THE PROVISION OF MEDICAL INFORMATION OR FOR THE PURPOSES OF OBTAINING MEDICAL TREATMENT.
This Agreement is effective as of the day you first download the Application or first access the Application, whichever is earlier (“Effective Date”), by and between Variety Children’s Hospital (“Nicklaus Children’s Hospital”), and you (“User”). For the sake of clarity, if you downloaded or otherwise obtained the Application from a Store, the operator or owner of that Store (the “Proprietor”) is neither a party to this license nor responsible for the Application in any way. In consideration of the promises and the mutual obligations of the parties set forth herein, and for other good and valuable consideration, the adequacy and sufficiency of which are hereby acknowledged, the parties agree as follows:
- Applications. Nicklaus Children’s Hospital offers certain software products. These Applications may be proprietary work of Nicklaus Children’s Hospital or may be the proprietary work of third parties who have granted Nicklaus Children’s Hospital the right to sublicense the Applications.
- License to Applications. Nicklaus Children’s Hospital hereby grants to User a limited, non-exclusive, non-transferable, non-assignable license to install and use the object code of the Application on one device (e.g., computer, smart phone, or tablet) solely for use by one User at one time and solely in conjunction with User’s use of the Nicklaus Children’s Hospital Platform. User may not (i) install Applications on computer products designed to allow simultaneous access by multiple end users, such as those in a server or mainframe environment, or (ii) install Applications in a way to allow their utilization by anyone other than a human – computerized utilization of Applications is not allowed. User is responsible for ensuring that User has appropriate hardware, software, and connectivity to enable an Application to function in accordance with the documentation for the Application. User is solely responsible for ensuring that User's use of the Application is in keeping with the rights granted herein. User is responsible for keeping the Application up to date, including downloading and installing any new versions that may become available after installation. User is responsible for exercising appropriate care in all respects when using the Application so as to ensure User’s wellbeing and the wellbeing of those around User.
- Reservation of Rights. Nicklaus Children’s Hospital reserves all rights not expressly granted in Section 2 of this Agreement. Except as provided therein, User may not copy, use, sublicense, modify, adapt, or create derivative works of the Application or related documentation or remove any copyright or other proprietary rights notices. Nicklaus Children’s Hospital reserves the right to suspend or terminate access by any User accessing the Application if such use represents a breach of the terms and conditions of this Agreement, without prejudice to any other remedies available to Nicklaus Children’s Hospital. All rights granted herein are a license, not a sale. Other than the rights licensed to User hereunder, User has no other implied license or right of any kind regarding the foregoing. User shall not itself, and shall not permit any other party to, directly or indirectly, in whole or in part, sublicense, distribute, lease, make available as a service bureau or otherwise allow any third parties any right or access to the Application; disassemble, decompile, decrypt, or reverse engineer, or otherwise attempt to discover or replicate source code for the Application. User acknowledges and agrees that Nicklaus Children’s Hospital owns and retains all rights existing from time to time in any jurisdiction under copyright law, patent law, moral rights law, trade secret law, confidential information law, trademark law, unfair competition law or other similar rights (“Proprietary Rights”) in the Application, documentation, any training materials and any copies, modifications, adaptations, derivative works, and enhancements thereof, by whomever produced. User agrees that any threatened or actual breach of Nicklaus Children’s Hospital‘s Proprietary Rights by User shall constitute immediate, irreparable harm to Nicklaus Children’s Hospital for which monetary damages is an inadequate remedy and for which equitable remedies may be awarded by a court of competent jurisdiction without requiring Nicklaus Children’s Hospital to post any bond or any other security (or if a court shall require a bond, then a bond in no amount above US $1,000). Nothing contained herein shall limit either party's right to any remedies at law, including the recovery of damages for breach of this Agreement.
- Fees and Payment. User shall pay Nicklaus Children’s Hospital the applicable fees for all Applications, if any, in accordance with terms of the Store from which User obtained the Applications (“Application Fees”). User acknowledges and agrees that Nicklaus Children’s Hospital will have no liability for any loss of the use of data resulting from its exercising the rights set forth in this paragraph.
- Privacy. Nicklaus Children’s Hospital has created an Application Privacy Policy to inform you how Nicklaus Children’s Hospital might utilize information collected via the App.
- Warranty. User is solely responsible for ensuring that it exercises proper care at all times when using the application and user acknowledges that Nicklaus Children’s Hospital makes no representation or warranty as to the accuracy of the information provided or the results derived from the application. The application is not a medical device and should not be relied upon for the provision of medical information or for the purposes of obtaining medical treatment. All applications are provided “as is, where is.” Nicklaus Children’s Hospital provides no warranties, and to the maximum amount allowable by law expressly disclaims all warranties, guarantees, conditions, or representations, whether express, implied, statutory, or otherwise, with respect to any applications, including without limitation, any implied warranty of merchantability, error-free use, originality, or fitness for a particular purpose. User is solely responsible for ensuring that all applications operate in accordance with their documentation and user’s expectations. User’s sole remedy for any deviation thereto is to seek a refund for application fees as set forth in the first paragraph of this agreement.
- Term. This Agreement shall be effective as of the Effective Date. Nicklaus Children’s Hospital may terminate this Agreement at any time by providing User with written notice of Nicklaus Children’s Hospital’s intent to do so. This Agreement shall automatically terminate upon the earliest of (i) User erasing or uninstalling the subject Application, (ii) User selling or otherwise alienating the device upon which the Application is installed, (iii) User assigning any of its assets to its creditors, or voluntarily or involuntarily petitioning for the protection of bankruptcy court, or (iv) User otherwise expresses its intent to no longer utilize an Application. Rights of termination are in addition to any other remedies available to Nicklaus Children’s Hospital, at law or in equity. Upon any termination or expiration of this Agreement all license rights shall immediately terminate and User shall immediately cease use of the Application. The following sections of this Agreement shall survive: 1, and 3 - 11. Nicklaus Children’s Hospital shall have no obligation under this Agreement to provide any data or information of any kind to User following termination.
- Indemnification. User shall indemnify and hold harmless Nicklaus Children’s Hospital from any loss, damage, liability, cost or expense suffered or incurred in connection with any claim, suit or proceeding brought by a third party against Nicklaus Children’s Hospital to the extent that it arises out of User's use of the Application, use of the Application to obtain medical treatment, or User’s failure to exercise proper care while using the Application. This indemnity shall survive the termination of this Agreement. Nicklaus Children’s Hospital shall indemnify and hold harmless User for any third party claim that the Application, unmodified by anyone other than Nicklaus Children’s Hospital, in and of itself, violates that third party’s intellectual property rights.
- Limitations of Liability. Neither Nicklaus Children’s Hospital nor its officers, directors, employees, shareholders, agents, licensors, resellers or representatives (collectively “Nicklaus Children’s Hospital parties”) shall be liable for any incidental, indirect, special, exemplary or consequential damages, including but not limited to lost profits, time, savings, data, or goodwill, damages arising from use of or inability to use the application or any related applications, products or services, or cost of replacement goods or services, whether foreseeable or unforeseeable, that may arise out of or in connection with the application or any related functionality, services, products, applications or otherwise relating to the subject matter of this agreement, regardless of whether such damages are based in contract, tort (including negligence), warranty, strict liability, products liability or otherwise, even if they have been notified of the possibility or likelihood of such damages occurring. Except for any direct damages for bodily injuries or tangible property damage proximately caused by Nicklaus Children’s Hospital, the maximum aggregate liability of the Nicklaus Children’s Hospital parties in all events shall be limited to the higher of the price user paid to the store or Nicklaus Children’s Hospital for the application, one thousand US dollars (US $1,000), or the lowest amount allowable by law.
- Dispute Resolution and Arbitration. The parties agree that, except as otherwise provided below, they shall first attempt to resolve any dispute, claim or controversy relating in any way to this Agreement (a “Dispute”) between an officer (applicable to User only if User is an organization) of each party who has authority to resolve the Dispute. If any Dispute cannot be settled in this manner within sixty (60) days of written notice being served by a party on the other party, the parties agree that the Dispute may be settled by arbitration in accordance with the Commercial Arbitration Rules of American Arbitration Association (“Rules”) in Florida in the United States of America, with judgment upon the award rendered by the arbitrator to be entered in any court of competent jurisdiction. Any arbitrator selected pursuant to the Rules will conduct arbitration and the arbitrators will have a background or training in contract law and intellectual property. The arbitrators may award attorneys’ fees and costs to the prevailing party. Notwithstanding the foregoing, either party may apply to any court of competent jurisdiction for a temporary restraining order, preliminary injunction, or other interim, conservatory or equitable relief, as necessary, without breach of this arbitration Agreement and without any abridgment of the powers of the arbitrator(s).
- Generally. User may not assign this Agreement or any rights and obligations hereunder in whole or in part. Any attempted assignment in contravention hereof shall be void and of no effect. Nicklaus Children’s Hospital may assign this Agreement at will. The terms and conditions of this Agreement shall inure to the benefit of and be binding upon the respective successors and assigns of the parties. No delay or failure in exercising any right hereunder and no partial or single exercise thereof shall be deemed to constitute a waiver of such right or any other rights hereunder. No consent to a breach of any express or implied term of this Agreement shall constitute consent to any prior or subsequent breach. If any provision hereof is declared invalid by a court of competent jurisdiction, such provision shall be ineffective only to the extent of such invalidity, so that the remainder of that provision and all remaining provisions of this Agreement shall be valid and enforceable to the fullest extent permitted by applicable law. Should any provision of this Agreement require judicial interpretation, the parties agree that the court interpreting or construing the same shall not apply a presumption that this Agreement shall be more strictly construed against one party than the other. This Agreement shall be governed by and construed in accordance with the laws of the State of Florida, in the United States of America, without regard to its rules regarding conflict of laws or the application of UCITA or any international conventions on the transfer of technology or goods. Each party hereby consents to the exclusive jurisdiction of the state and federal courts located in and around Miami, Florida, in the United States of America.
- User Consent and Warranties. By utilizing the Application you agree to transact business with Nicklaus Children’s Hospital electronically and you represent and warrant that you have the authority to accept this Agreement on behalf of yourself and any institution you represent, that you are more than 18 years of age, will abide by and comply with this Agreement, are not located in a country that is subject to a U.S. Government embargo or that has been designated by the U.S. Government as a “terrorist supporting” country, are not listed on any U.S. Government list of prohibited or restricted parties, and shall not export the Application itself or use the Application to export any information in violation of the laws of the United States of America.
mobileapp-privacy-policy
Mobile Application Privacy Policy
EFFECTIVE: 1 MARCH 2023
VARIETY CHILDREN’S HOSPITAL (referred to as “Nicklaus Children’s Hospital”, “we,” “our,” “us,” or “Company”) recognizes that you care how information about you is collected and used. Nicklaus Children’s Hospital has created this Privacy Policy to inform you of our information collection, use and sharing practices.
Please be advised that the practices described in this Privacy Policy apply only to information gathered through mobile applications created by us for our customers (the “App”) and do not necessarily reflect our practices with respect to information gathered through other means. Use of the App is subject to our End User License Agreement (EULA) and to our personal information gathering and dissemination practices and policies as described below.
We Collect The Following Types of Information
Account Creation
We do not require that you create an account in order to utilize the App. Yet still, creating an account may be offered to personalize and enhance the user experience, but will always be optional. Whether you create an account or not, the App does use Unique Identifiers (as discussed below).
Additionally, the third party store that licensed the App to you (e.g., the Apple App Store or Google Play Store) may have collected personal information from you and may provide that information to us. We shall only utilize that information for the purposes of ensuring the proper licensing of the App.
App Usage
We may collect information regarding App usage such as geographic, specific feature usage, and search information. We utilize this information to analyze the performance of and improve the App to provide current and future users with a fulfilling experience.
Unique Identifiers
We use “Unique Identifiers” to enable your use of the App. Unique Identifiers are small files used by our App that are stored on your device when the App is first installed for the purposes of identifying your device for consistent usage across sessions in the App. Unique Identifiers are installation specific: if the App is uninstalled and reinstalled, the old Unique Identifier is deleted and a new Unique Identifier is installed. These Unique Identifiers do not contain any personally identifiable information or information that we could use to ascertain your identity, such as your name. We use Unique Identifiers to track the usage of the App and to enhance your use of the App.
To Contact You
If we are provided your personal information by you or the third party store that licensed the App to you, we may use your personal information to contact you. Using your personal information, we may also send you e-mail messages under the following circumstances, among others:
- to respond to an inquiry or request for information;
- to provide technical support;
- to thank you for contacting us;
- to welcome you to the App;
- to explain new offerings and features of Nicklaus Children’s Hospital;
- to communicate with you regarding your use of the App
Your contact information may be available or provided to third-party service providers and contractors that are contractually obligated to protect your information as disclosed in this App Privacy Policy.
We May Share And Disclose Your Information In The Following Ways
Aggregated Information
We may collect aggregated information about our users, such as geographic, App feature usage, search information, etc. We may share certain information that we collect with our business partners regarding the users of the App. The aggregated information that we provide is not directly linked to any personally identifiable information.
Services
We will use your information to provide information or perform services that you request we, or a third party, provide or perform. If the applicable information is to be provided or service is to be performed by a third party, then we will disclose the applicable information to the third party providing the information or performing the applicable service.
Internal Use
We may share your information within our business for the purposes of furthering our business, including analyzing your information and other uses.
Exceptions
We may use and disclose your information to the extent reasonably necessary to:
- correct technical problems and malfunctions in how we provide our products and services to you and to technically process your information;
- protect the security and integrity of the App and our service, including without limitation to enforce our End User License Agreement with you;
- protect our rights and property and the rights and property of others;
- take precautions against liability;
- respond to claims that your use of the App violates the rights and interests of third parties;
- the extent required by law or to respond to judicial process; and
- the extent permitted under other provisions of law, to provide personal information to law enforcement agencies or for an investigation on a matter related to public safety.
You understand and agree that your information may be required to:
- send and receive communications regarding your use of the App;
- conform to the technical requirements of connecting networks;
- conform to the limitations of our service; or
- conform to other, similar technical requirements.
Usage Tracking
We may monitor how our users use our App including without limitation search terms entered, screens/pages visited, and documents viewed. This information may be stored with your Unique Identifier. Aggregated forms of this data may also be used in order to help us understand areas for future research, identify future features and functions to develop for the App, and to market the App.
Links to Other Sites
This App may contain links to other applications, web sites, and products. We are not responsible for and shall not have any liability arising from the privacy practices or the content found by your utilization of such links.
Storage Of Information
We may store information collected via the App or provided to us, including without limitation your information, indefinitely.
Information Review
You may contact us to discuss changing and modifying any incorrect information that you provide to us by contacting us at: support@nicklauschildrens.org.
Security Precautions
Nicklaus Children’s Hospital takes commercially and technologically reasonable precautions to protect data and information under its control from misuse, loss, or alteration. Nicklaus Children’s Hospital’s security measures include industry-standard technology and equipment to help protect your information, and we maintain security measures to allow only the appropriate personnel and contractors access to your information. Unfortunately, no system can ensure complete security, and Nicklaus Children’s Hospital disclaims any liability resulting from use of the App. If you have any questions about the security at our App, please send an e-mail to: support@nicklauschildrens.org.
Notification of Changes to Our App Privacy Policy
We reserve the right to change or modify our information collection, use and disclosure practices set forth in this App Privacy Policy. If we decide to change our App Privacy Policy, we will post those changes to the App so our users and customers are always aware of what information we collect, use and disclose. If at any point we decide to use or disclose your information in a manner different from that stated at the time it was collected, we will notify you in writing, which may or may not be by e-mail. If you object to the change to our App Privacy Policy, then you must contact us using the information provided in the notice. We will otherwise use and disclose a user’s information in accordance with the App Privacy Policy that was in effect when such information was collected.
Change in Control
If Nicklaus Children’s Hospital experiences a “change in control” (defined below), then we may amend our information practices as described in this App Privacy Policy. We will disclose your information to the legal entity that succeeds our operation of the App. The privacy policy of the succeeding legal entity will then govern the information that we have collected from you under this App Privacy Policy. However, if applicable law prohibits the succeeding legal entity’s privacy policy from governing, then this App Privacy Policy shall continue to govern.
“Change in control” means any of the following events:
- we undergo a reorganization, merger, consolidation, acquisition or other restructuring involving all or substantially all of our voting securities and/or assets, by operation of law or otherwise;
- we become insolvent;
- we make a general assignment for the benefit of creditors;
- we suffer or permit an appointment of a receiver for our business or assets;
- we become subject to any proceedings under any bankruptcy or insolvency law, whether domestic or foreign; or
- we are liquidated, voluntarily or otherwise.
Questions about Our App Privacy Policy
If you have any questions about this App Privacy Policy and/or the personal information practices of our App, please email your questions to: support@nicklauschildrens.org.
Neurological Lecture

Neurological issues, surgical developments, & medical advances in the management of children with brain tumors
Wednesday, June 21, 2023
6:30 p.m. - 7:30 p.m.
Objectives:
- Describe the neurological issues, (symptoms, signs, & sequelae), related to brain tumors
- Discuss the surgical advances in neuro-oncology
- Describe the neurologic complications of Brain Tumors
Presenting Physicians/Titles:
- Toba Niazi, MD, Medical Director of Neuro-Oncology Surgical Services, Nicklaus Children’s Hospital
- Ziad Khatib, MD, Director Division of Pediatric Hematology Oncology, Director of Medical Neuro-Oncology
- Anuj Jayakar, MD, Medical Director of the Neurocritical Care Program, Nicklaus Children’s Hospital
Thank You
Backyard Pool Safety
Children love to play in water. Yet, children and bodies of water can be a dangerous combination. Nationally, drowning is the second cause of unintentional injury-related death among children ages 1 to 14.
Our Partners
In an effort to prevent drowning, Nicklaus Children’s Hospital, the YMCA of South Florida, Miami-Dade County Parks and Recreation, NBC 6 and Telemundo are collaborating to promote water safety.
Be a Water Watcher
The most important action one can take to protect children is to ensure they are attentively supervised when in or near water. That means an adult is constantly watching the child or children without distraction from tablets, smartphones, book, or other adults or children. Remember, drowning is a silent event and can occur within a matter of seconds.
Our Water Watcher card can be handed from adult to adult, to serve as a physical reminder as to who is the designated watcher. To request your Water Watcher card, click below.
Use Alarms During Swim Time

No matter how careful you are, it only takes a moment to lose sight of your kids. That's why one should ensure alarms and barriers are the next layer of safety to protect children. Install active alarms on doors leading to the outside so kids can't slip out without your knowledge.
Ensure you also have barriers around your pool or property if you live near water. That means property fences, pool fences, and even pool alarms that alert you to moving water when no one should be in the pool.
Drowning Prevention Tips
- Actively supervise children every time they are in or around water. Don't leave or look away, even for a moment.
- Use barriers (fences, pool covers, pool alarms) to keep kids away from water when you're not around. After use, empty buckets, tubs, and wading pools.
- Teach children never to go near a pool drain and to pin up long hair when in water.
- Everyone should know the water safety rules. No swimming alone!
- Make sure children take swimming lessons. But even those who have taken swim lessons should be supervised while in or around the water. Accidents can and do happen.
- Learn CPR and keep rescue equipment (like a life-saving ring), a telephone, and emergency phone numbers poolside.
Learn more about drowning prevention and visit RedCross.org for additional CPR Training.
Swimming Lessons in Your Community
Both the YMCA of South Florida and Miami-Dade County Parks and Recreation offer swimming instruction at a wide range of locations.For YMCA locations visit below.
Locate YMCA of South Florida Swimming Lessons
For locations in Miami-Dade County Parks, please click below.
Locate Miami-Dade County Parks Swimming Lessons
Additional Video Resources
Backyard Pool Safety
Children love to play in water. Yet, children and bodies of water can be a dangerous combination. Nationally, drowning is the second cause of unintentional injury-related death among children ages 1 to 14.
Our Partners
In an effort to prevent drowning, Nicklaus Children’s Hospital, the YMCA of South Florida, Miami-Dade County Parks and Recreation, NBC 6 and Telemundo are collaborating to promote water safety.
Be a Water Watcher
The most important action one can take to protect children is to ensure they are attentively supervised when in or near water. That means an adult is constantly watching the child or children without distraction from tablets, smartphones, book, or other adults or children. Remember, drowning is a silent event and can occur within a matter of seconds.
Our Water Watcher card can be handed from adult to adult, to serve as a physical reminder as to who is the designated watcher. To request your Water Watcher card, click below.
Use Alarms During Swim Time

No matter how careful you are, it only takes a moment to lose sight of your kids. That's why one should ensure alarms and barriers are the next layer of safety to protect children. Install active alarms on doors leading to the outside so kids can't slip out without your knowledge.
Ensure you also have barriers around your pool or property if you live near water. That means property fences, pool fences, and even pool alarms that alert you to moving water when no one should be in the pool.
Drowning Prevention Tips
- Actively supervise children every time they are in or around water. Don't leave or look away, even for a moment.
- Use barriers (fences, pool covers, pool alarms) to keep kids away from water when you're not around. After use, empty buckets, tubs, and wading pools.
- Teach children never to go near a pool drain and to pin up long hair when in water.
- Everyone should know the water safety rules. No swimming alone!
- Make sure children take swimming lessons. But even those who have taken swim lessons should be supervised while in or around the water. Accidents can and do happen.
- Learn CPR and keep rescue equipment (like a life-saving ring), a telephone, and emergency phone numbers poolside.
Learn more about drowning prevention and visit RedCross.org for additional CPR Training.
Swimming Lessons in Your Community
Both the YMCA of South Florida and Miami-Dade County Parks and Recreation offer swimming instruction at a wide range of locations.For YMCA locations visit below.
Locate YMCA of South Florida Swimming Lessons
For locations in Miami-Dade County Parks, please click below.
Locate Miami-Dade County Parks Swimming Lessons
Additional Video Resources
WaterSafety
DB Staff
Cardiovascular

Cardiovascular Prevention in Children: What the Pediatrician Needs to Know
Wednesday, July 26, 2023
Arrival & On-Site Registration 6:30 P.M. to 7 P.M.
Lecture to begin at 7 P.M.
Join us for an educational lecture on cardiovascular prevention in children presented by the Heart Institute at Nicklaus Children’s Hospital.
Objectives:
- The integrated cardiovascular health schedule
- Family history of early coronary artery disease
- Lipid screening and management of dyslipidemia
Registration is now closed.
Thank You
Doral Closure: Endo Clinics Dr. Carrillo
Un mensaje importante sobre las citas de Endocrinología en el Nicklaus Children's Doral Outpatient Center
Estimado padre/madre o cuidador:
Gracias por permitirme la oportunidad de cuidar de usted o su hijo/a. Quería informarle que las citas de Endocrinología ya no se ofrecen en el Nicklaus Children's Doral Outpatient Center.
Seguiré disponible para continuar brindando atención en el campus principal de Nicklaus Children's Hospital, ubicado cerca de Coral Gables (3100 SW 62 Avenue, Suite #102, Miami, FL 33155).
Si tiene alguna pregunta, no dude en ponerse en contacto con nosotros en el 305-662-8368. También puede llamar al 888-624-2778 (APPT) para programar citas.
Espero volver a verle pronto.
Con mis mejores deseos y sincero agradecimiento,
Adriana Carrillo Iregui, MD
Endocrinóloga Pediátrica y Directora Médica, Programa de Diabetes
Nicklaus Children’s Pediatric Specialists (NCPS)
Doral Closure: Endo Clinics Dr. Pagan
Un mensaje importante sobre las citas de Endocrinología en el Nicklaus Children's Doral Outpatient Center
Estimado padre/madre o cuidador:
Gracias por permitirme la oportunidad de cuidar de usted o su hijo/a. Quería informarle que las citas de Endocrinología ya no se ofrecen en el Nicklaus Children's Doral Outpatient Center.
Seguiré disponible para continuar brindando atención en el campus principal de Nicklaus Children's Hospital, ubicado cerca de Coral Gables (3100 SW 62 Avenue, Suite #102, Miami, FL 33155). Además, comenzaré a atender pacientes en el Centro Ambulatorio Nicklaus Children's Dan Marino (2900 S. Commerce Parkway, Weston FL 33331) a partir del 7 de julio de 2023.
Si tiene alguna pregunta, no dude en ponerse en contacto con nosotros en el 305-662-8368. También puede llamar al 888-624-2778 (APPT) para programar citas.
Espero volver a verle pronto.
Con mis mejores deseos y sincero agradecimiento,
Pedro Pagán, MD
Endocrinólogo Pediátrico
Nicklaus Children’s Pediatric Specialists (NCPS)
Nicole POM
Meet the BMT Team
Our Pediatric BMT program is comprised of a multidisciplinary team of clinicians that come together to provide consultation, evaluation and follow up care to each individual patient's needs.
ToMyNicklaus
Free EKG Screening Event RSVP
Doral Closure: Gastro Dr. Caicedo
Un mensaje importante sobre las citas de Endocrinología en el Nicklaus Children's Doral Outpatient Center
Estimado padre/madre o cuidador:
Gracias por permitirme la oportunidad de cuidar de usted o su hijo/a. Quería informarle que las citas de Gastroenterología ya no se ofrecen en el Nicklaus Children's Doral Outpatient Center.
Seguiré disponible para continuar brindando atención en el Nicklaus Children's Pediatric Specialists en Alton Road (4308 Alton Road, Suite #940, Miami Beach, FL 33140). Tenga en cuenta que también tendré citas limitadas disponibles en el campus principal de Nicklaus Children's Hospital (3100 SW 62 Avenue, Suite #6-100, Miami, FL 33155), donde se realizarán todos mis procedimientos.
Si tiene alguna pregunta, no dude en ponerse en contacto con nosotros en el 786-624-3400. También puede llamar al 888-624-2778 (APPT) para programar una cita conmigo.
Espero volver a verle pronto.
Con mis mejores deseos y sincero agradecimiento,
Luis F Caicedo Oquendo, MD
Director Médico del Programa de Trasplante Fecal
Director del Programa de Becas de Gastroenterología, Hepatología y Nutrición Pediátricas
Nicklaus Children’s Pediatric Specialists (NCPS)
Doral Closure: Dev-Behav Dr. Fierro
Un mensaje importante sobre las citas de Endocrinología en el Nicklaus Children's Doral Outpatient Center
Estimado padre/madre o cuidador:
Gracias por permitirme la oportunidad de cuidar de usted o su hijo/a. Quería informarle que las citas de desarrollo y comportamiento ya no se ofrecen en el Nicklaus Children's Doral Outpatient Center.
Seguiré disponible para continuar brindando atención en el Nicklaus Children's Pediatric Specialists en Pinecrest (11521 South Dixie Highway, Suite #201, Pinecrest, FL 33156), también atenderé a pacientes en el Glady's M. and Frederick Stewart Pediatric Care Center, ubicado en el primer piso del Blue Garage, en el campus principal de Nicklaus Children's Hospital cerca de Coral Gables (3100 SW 62 Avenue, Miami, FL 33155).
Si tiene alguna pregunta, no dude en ponerse en contacto con nosotros en el 786-624-5108. También puede llamar al 888-624-2778 (APPT) para programar una cita conmigo en cualquiera de las dos ubicaciones.
Espero volver a verle pronto.
Con mis mejores deseos y sincero agradecimiento,
Victoria Fierro, MD
Pediatra del desarrollo y el comportamiento
Nicklaus Children’s Pediatric Specialists (NCPS)
Campaign
Meet the Team
Mask Wearing Requirements
As of August 1, 2023, masks are required only in certain circumstances. Examples include persons exhibiting signs or symptoms of an infectious disease, in areas of the facility that are designated sterile, or if the applicable person will be around an immunocompromised patient. This policy applies to all Nicklaus Children's staff members, patients, and visitors two years of age and older. Patients and visitors can contact the patient’s healthcare team (e.g., the treating provider’s office or inpatient unit) and staff members can contact the Infection Prevention and Control Department at ext. 2399.
Patients
Patients will be required to wear a mask in the common areas of Nicklaus Children’s locations if the patient is exhibiting signs or symptoms of respiratory illness or has a diagnosed infectious disease that can be spread through droplet or airborne transmission.
- In such circumstances, patients should ask for a mask upon arrival to Nicklaus Children’s or patients will be given a mask by a staff member.
- Subject to Florida Statutes Section 381.026, if an alternative method of infection control is available, patients may opt out of such existing masking requirement by notifying a staff member and such request will be reviewed in consultation with the hospital’s Infection Prevention and Control Department. Notwithstanding this opt-out provision, a patient may not opt out if:
- opting out would infringe upon the rights of another patient and would risk the safety or health of other patients, visitors, or staff members (e.g., patient could transmit an infection to another patient), or
- the patient is medically or programmatically contraindicated for documented medical, safety or programmatic reasons.
Visitors
Visitors will be required to wear a mask if the visitor is:
- Exhibiting signs or symptoms of respiratory illness or has a diagnosed infectious disease that can be spread through droplet or airborne transmission;
- In any sterile area of any Nicklaus Children’s location or an area where sterile procedures are being performed; • In an inpatient or clinical room with a patient who is exhibiting signs or symptoms of respiratory illness or has a diagnosed infectious disease that can be spread through droplet or airborne transmission; or
- Visiting a patient whose (i) treating healthcare practitioner has diagnosed the patient with an immunocompromising condition, which is known to increase the risk of transmission of an infection to the patient from others without signs or symptoms of infection, and (ii) whose treating practitioner has determined that masks are necessary for the patient’s safety.
If any of these circumstances apply, visitors should ask for a mask upon arrival to the Nicklaus Children’s location or visitor will be given a mask by a staff member.
Visitors may opt out of these masking requirements if an alternative method of infection control or infectious disease prevention is available. Visitors seeking to opt out in accordance with this policy shall notify a staff member and such request will be reviewed in consultation with the hospital’s Infection Prevention and Control Department on a case-by-case basis.
Staff Members
Staff members should avoid entering Nicklaus Children’s locations if they are sick. Staff members include any person that is a Nicklaus Children’s employee, volunteer, student, resident, independent contractor, vendor, consultant, traveler, or any other person who provides any care, treatment, or other services (including clinical staff and physicians) to any Nicklaus Children's locations and/or patients of Nicklaus Children's locations. Staff members who are sick should contact their immediate supervisor, as applicable and in accordance with their department call out procedures, and the Employee Health Office (if on Nicklaus Children’s payroll) for further direction.
Staff members will be required to wear a mask if staff members are:
- Conducting a sterile procedure;
- Working in a sterile area or an area where sterile procedures are being performed;
- Working with a patient who is exhibiting signs or symptoms of respiratory illness, has a diagnosed infectious disease that can be spread through droplet or airborne transmission, or is on droplet or airborne isolation;
- Working with a patient (i) whose treating healthcare practitioner has diagnosed the patient with an immunocompromising condition, which is known to increase risk of transmission of an infection from staff members without signs or symptoms of infection, to the patient, and (ii) whose treating practitioner has determined that masks are necessary for the patient’s safety; or
- Engaging in non-clinical potentially hazardous activities that require masks to prevent physical injury or harm in accordance with industry standards.
Staff members may request to opt out of any Nicklaus Children’s Hospital existing masking requirements, except in circumstances set forth above, and such request will be reviewed by Employee Health Office in consultation with the hospital’s Infection Prevention and Control Department on a case-by-case basis. Documentation of this process will be kept in the staff member’s employee health file, if applicable.
Nicklaus Children’s reserves the right to require the use of masks at all locations in other circumstances and consider other exclusions from all of the opt-out provisions in this policy, consistent with national and state standards, and state and federal laws, rules, requirements and regulations.
Patient Resources
Hospitals can be intimidating places for children, especially those with behavioral, sensory, or communication vulnerabilities. Having a plan to support your child before, during, and after their hospital visit or stay can help provide a more comfortable experience.
Before Coming to the Hospital
Talking to your child about the upcoming hospital visit can help manage fears or anxiety. When talking to your child about their upcoming visit:
- Have open communication about what to expect, using language they can understand.
- Use pictures as an added resource to support your conversation.
- Answer any questions to the best of your ability.
Your child may also benefit from:
- Roleplay, reading books or social narratives about the hospital and healthcare providers
- Medical play kits can be a helpful tool in normalizing the hospital experience
- Pictures and videos of the hospital before their stay
Whether you are coming for a short visit or overnight stay, bringing items that are comforting to your child can contribute to your child feeling less anxious during their stay. Allowing your child to choose their favorite blanket, toy, or sensory tool to bring may also provide comfort. If your child uses a communication device, tool, or aid, remember to bring it along.
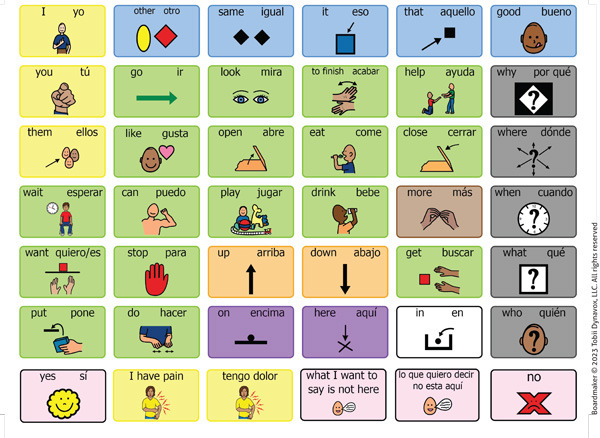
Click to download the Core Word Board (PDF)
While at the Hospital
- If staying overnight, continue your child’s home routine as much as possible. Daily tasks like brushing teeth, bathing, napping, and mealtimes can provide the comfort of consistency in a different environment.
- Allow your child to make as many choices as possible during their visit. Some examples include the color of socks or food choice (dietitian and medically appropriate, based on current diagnosis/care plan).
- Communicate needs or preferences to your child’s care team, including their likes, dislikes, significant fears or triggers, communication method(s), and anything crucial to your child’s care. Reach out to the Child Life/Adaptive Care team before the hospitalization with any additional needs.
After the Hospital
A hospital visit may be scary and disruptive, which can impact your child’s behavior. To support your child during this transition, allow time for your child to adjust, and resume your home routine as soon as they are ready. Talk to your child about the hospital visit and allow them to ask questions. Communication will help your child in understanding and preparing for future visits.
Prepared by:
Gisselle Arriete, BCBA, Behavior Liaison Clinical Coordinator
Gabriela Baralt, BCBA, Behavioral Resource Advocate
Medical Chaperone Policy Attestation
Thank You
Pharmacy Residency Program
Who We Are
Salaries & Benefits
How To Apply
Scholarly Activity
Advance Directives
You have the right to fill out a form known as an Advance Directive. The form explains in advance how you would want to be cared for if a serious medical condition arises that would prevent you from telling your doctor how you want to be treated. For example, if you were brought to a healthcare facility in a coma, what would you want the facility’s staff to know as decisions are made regarding your care?
Download Form Download Form (Creole)
What is an Advance Directive?
An Advance Directive is a written or oral statement that is made and witnessed in advance of serious illness or injury, stating how you want medical decisions made. There are different types of advance directives, including:
- A “living will” and
- Healthcare surrogate designation
An Advance Directive allows you to express your decisions about your healthcare or to name someone to make those decisions for you, if you become unable to make decisions about your own medical treatment.
What is a Living Will?
A living will generally states the kind of medical care you want or do not want if you become unable to make your own decisions.
It is called a “living will” because it takes effect while you are still living. Florida law provides a suggested form for a living will. You may use this form or other living will models. A form designed by Nicklaus Children’s Hospital is available to you. You may wish to speak to an attorney or physician to be certain you have completed the living will in a way that your wishes will be understood.
What is a Healthcare Surrogate Designation?
A healthcare surrogate designation is a signed, dated and witnessed document naming another person such as parent, friend, husband, wife or close friend as your agent to make medical decisions for you, if you become unable to make them for yourself. You can include instructions about any treatment you want or wish to avoid. Florida law provides a suggested form for designation of a healthcare surrogate. You may use it or some other form, such as one available to you at Nicklaus Children’s Hospital. You may wish to name a second person to represent you, in case your first designee is not available.
Which is Better?
You may wish to have both a living will and a healthcare surrogate designation, or combine them into a single document that describes treatment choices in a variety of situations, and names someone to make decisions for you should you be unable to make decisions for yourself.
Why Should I Complete an Advance Directive?
Advance directives can protect people who are very ill and unable to communicate. They can help give you control over your control over your health care. They also relieve loved ones of the burden of guessing what you would want to do.
Do I Have to Write an Advance Directive under Florida Law?
No, there is no legal requirement to complete an Advance Directive. However, if you have not made an Advance Directive or designated a healthcare surrogate, care decisions may be made for you by your court-appointed guardian, your parent, adult sibling, spouse, adult relative or close friend. This person should be called a proxy.
Can I Change My Mind After I write a Living Will or Designate a Healthcare Surrogate?
Yes, you may change or cancel these documents at any time. It is important that you review the documents regularly to make sure that they clearly reflect your current thoughts and wishes. Any changes should be written, signed and dated.
You can also change an Advance Directive by oral statement.
What If I Have Filled Out An Advance Directive In Another State and Treatment in a Healthcare Facility In Florida?
An Advance Directive completed in another state, in compliance with the other state’s law, can be honored in Florida.
What Should I Do With My Advance Directive if I Choose to Have One?
Make sure that someone such as your doctor, lawyer, or family member know that you have an Advance Directive and where it is located. Consider the following:
- If you have designated a healthcare surrogate, give a copy of the document to this person.
- Give a copy of your Advance Directive to your doctor for your medical file.
- Keep a copy of your Advance Directive in a place where it can be found easily.
- Keep a card or a note in your purse or wallet which states that you have an Advance Directive and where it is located.
- If you change your Advance Directive, make sure your doctor, lawyer and/or family member has the latest copy.
Reference: Florida Statutes Chapter 765
UDCWebinar
Review-Dr-Fierro
Review-Dr-Tawfik
Review-Dr-Beckett
/Review-Dr-Bustamante-Escobar
Review-Dr-Granados
Review-Dr-Ramirez-Alcantara
Review-Dr-Irastorza
Review-Dr-Medina
/sari-kay-gastroenterology
abigail-ley-neurology
christopher-carafa-cardiac-critical-care
laura-irastorza-gastroenterology
gabriel-vidal-rodriguez-gastroenterology
/mercedes-bello-neurology
/Review-Dr-Lallas
Review-Dr-Monduy
Review-Dr-Ball
Review-Dr-Korman
Review-Dr-Kay
/Review-Dr-Vidal
Review-Dr-Mahfood
Review-Dr-Erkonen
Review-Dr-Pulido
Review-Dr-Sy
Review-Dr-McKinnon
Review-Dr-Ehret
Review-Dr-Horan
Review-Dr-Sanzo-Ramirez
Review-Dr-Bruscantini
Review-Dr-Kuluz
Review-Dr-Kowalsky
Review-Dr-Rodriguez-Barreto
Review-Dr-Pronman
Movement Disorders Program Home
Movement Disorders Program Home
Conditions we Treat
Conditions we Treat
Treatments and Procedures
Treatments and Procedures
Patient Stories
Patient Stories
Pediatric Neurosurgery
2023-2025 Strategic Plan

Leading children’s hospitals like ours have long recognized the need for innovation — not only to compete with new players disrupting traditional healthcare delivery, but also to provide care differentiated on the quality, outcomes, cost, and experience that today’s tech-savvy parents expect and demand.
At the core of our new strategic plan is a single north star: We must innovate with a goal of making the impossible possible for every child. No child should ever have to leave home to seek care, and other parents from around the world should be able to get answers from us they cannot find elsewhere. We must — and will — take the lead in radically redesigning our pediatric care pathways to meet the needs of children and families in the digital age.
I hope you will take a moment to review our strategic plan and reflect upon your part in helping us achieve our key priorities as we go forward for the children. We are proud of Nicklaus Children’s role in advancing the health and well-being of Florida’s children and look ahead to fulfilling our vision of creating a healthy future for every child for generations to come. Nicklaus Children’s will always be where your child matters most.
Download the 2023-2025 Strategic Plan in PDF (2 MB)RSVP Special Event

You are invited to a Fundraising Celebration in support of Nicklaus Children's Hospital at the home of:
Mr. & Mrs. Smith
Please join supporters and friends as we invest in a new era of healthcare for children and adolescents in South Florida.
Date: TBD
Time: 6:30-8:30 p.m.
Location: Café Vialetto Restaurant
Address: 4019 S Le Jeune Rd, Coral Gables, FL 33134
Please complete the form below to confirm attendance:
Thank you
Medical Staff Dues
Please select the fee you would like to pay for:
Annual Dues
Application Fee
Annual Dues - Allied Health Professional
Please fill out the registration to proceed to payment.
Payment
Annual Dues - Allied Health Professional $100
Click the button to pay with credit card.
Annual Dues - Physician
Please fill out the registration to proceed to payment.
Payment
Annual Dues - Physician $200
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
Application Fee - Allied Health Professional
Please fill out the registration to proceed to payment.
Payment
Application Fee - Allied Health Professional $200
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
Application Fee - Physician
Please fill out the registration to proceed to payment.
Payment
Application Fee - Physician $500
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
Application Fee - Recent Graduate
Please fill out the registration to proceed to payment.
Payment
Application Fee - Recent Graduate $250
Click the button to pay with credit card.
You will be re-directed to Authorize.net checkout.
NCPS Mixer

NCPS Mixer hosted by Nicklaus Children's Hospital
Thursday, January 18, 2024
6:00 p.m.
Nicklaus Children's Pediatric Specialists invites you to a physician meet and greet at Nicklaus Children's Hospital.
Season's 52
1862 Sawgrass Mills Circle
Sunrise, FL 33323
Thank You
ariella-barhen
Review-ED
CommunityResources
Pharmacy Program Home
Precision Analytics
What We Do
The Precision Analytics division of the Center for Precision Medicine includes projects and collaborations with physicians and researchers that leverage the power of genetic and health outcomes data to improve the lives of children and their families. Precision Analytics focuses on curating and sharing data within Nicklaus Children's Health System and with external partners for approved research use. The Precision Analytics program is in a unique position to lead genetics data curation and research with the diverse patient populations broadly represented within the health system.
OneFlorida+ Partnership
Precision Analytics is proud to be a part of the OneFlorida+ Clinical Research Network. OneFlorida+ is a patient centered research partnership across 15 academic institutions and healthcare systems spanning Florida, and regions of Georgia and Alabama. Our overarching goal is to improve patient care and health outcomes through the implementation of innovative research findings. A key part of our participation in OneFlorida+ is our support of the Data Trust, where we transform, curate, and securely store anonymized health related data to support ongoing OneFlorida+ research studies. Our contribution to OneFlorida+ has helped advance pediatric research on various topics, such as COVID-19 recovery and long-term health.
Patient Stories
Rare and Undiagnosed Disease Programs Home
FundCancer
Epilepsy Webinar

Evaluations in Epilepsy Management: Neurophysiology and Imaging
Wednesday, November 15, 2023
7 p.m. - 8 p.m.
Webinar link provided upon registration.
Topics:
Developmental regression in infancy and childhood
Surgical options and advances in the treatment of childhood epilepsy
Speakers:
Shelly Wang, MD
Pediatric Neurosurgeon
Nicklaus Children’s Hospital
Matt Lallas, MD
Pediatric Neurologist and Epileptologist
Nicklaus Children’s Hospital
Trevor Resnick, MD
Pediatric Neurologist
Nicklaus Children’s Hospital
Thank You
Clinical Trials
A Feasibility Safety Study of Benign Centrally-Located Intracranial Tumors in Pediatric and Young Adult Subjects
The goal of this prospective, non-randomized, single-arm, feasibility study is to develop data to evaluate the safety and feasibility of ExAblate 4000 treatment of benign intracranial tumors which require clinical intervention in pediatric and young adult subjects.
Indication of Use: Ablation of benign intracranial tumors in children and young adults which are ExAblate accessible.
Conditions: Intracranial Tumors
Interventions: Device: ExAblate 4000 System
Eligibility: 8 Years to 22 Years
Principal Investigator: John Ragheb
Learn more at https://clinicaltrials.gov/study/NCT03028246.
Predicting Seizure Responsiveness to Neuromodulation Using Connectomic Profiling (Vagus Nerve Stimulation [VNS] Study)
Conditions: Epilepsy
Principal Investigator: Shelly Wang
Learn more at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8995963/.
A Phase 2 dose-escalation study examining the safety, pharmacokinetics, and preliminary efficacy of ascending drug and energy dose combinations for sonodynamic therapy using SONALA-001 in combination with Exablate 4000 Type 2.0 MR-Guided Focused Ultrasound in subjects with Diffuse Intrinsic Pontine Glioma (DIPG)
Conditions: Glioma
Principal Investigator: Toba Niazi
Learn more at https://clinicaltrials.gov/study/NCT05123534.
A Safety and Feasibility Study to Evaluate Blood Brain Barrier Disruption Using Exablate MR Guided Focused Ultrasound in Combination With Doxorubicin in Treating Pediatric Patients With Diffuse Intrinsic Pontine Gliomas (DIPG)
Conditions: Diffuse Intrinsic Pontine Gliomas
Principal Investigator: Toba Niazi
Learn more at https://clinicaltrials.gov/study/NCT05630209.
Clinical Trials
Neurosurgery Clinical Trials
A Feasibility Safety Study of Benign Centrally-Located Intracranial Tumors in Pediatric and Young Adult Subjects
The goal of this prospective, non-randomized, single-arm, feasibility study is to develop data to evaluate the safety and feasibility of ExAblate 4000 treatment of benign intracranial tumors which require clinical intervention in pediatric and young adult subjects.
Indication of Use: Ablation of benign intracranial tumors in children and young adults which are ExAblate accessible.
Conditions: Intracranial Tumors
Interventions: Device: ExAblate 4000 System
Eligibility: 8 Years to 22 Years
Principal Investigator: John Ragheb
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT03028246.
Epilepsy Clinical Trials
A Phase 3, Randomized, Double-blind, Placebo-controlled Trial of Adjunctive Ganaxolone (GNX) Treatment in Children and Adults with Tuberous Sclerosis Complex (TSC)-related Epilepsy
Conditions: Epilepsy
Principal Investigator: Matt Lallas
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT05323734.
A Multicenter, Open-Labe, Randomized, Active Comparator Study to Evaluate the Efficacy, Safety, and Pharmacokinetics of Lacosamide in Neonates with Repeated Electroencephalographic Neonatal Seizures
Conditions: Epilepsy
Principal Investigator: Anuj Jayakar
CRA: Marinellie Vega
A double-blind, randomized, placebo-controlled study to evaluate the efficacy and safety of intravenous Ganaxolone in status epilepticus Ganaxolone
Conditions: Epilepsy
Principal Investigator: Anuj Jayakar
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT04391569.
A Randomized, Dose-Finding and Confirmatory, Double-Blind, Placebo-Controlled, Parallel-Group Multicenter Study with a 2-Stage Adaptive Design and Randomized Withdrawal to Evaluate the Efficacy, Safety, and Tolerability of Brivaracetam as Monotherapy in Patients 2 to 25 Years of Age with Childhood Absence Epilepsy or Juvenile Absence Epilepsy
Conditions: Epilepsy
Principal Investigator: Anuj Jayakar
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT04666610.
Neurology Clinical Trials
Early Access Program with Arimoclomol for the Treatment of Niemann-Pick disease Type C in the US
Conditions: Niemann-Pick
Principal Investigator: Paula Schleifer
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT04316637.
Intrathecal 2-Hydroxypropyl-B-cyclodextin for Neurological Decline in Patients with Niemann-Pick Disease Type C1
Conditions: Niemann-Pick
Principal Investigator: Paula Schleifer
CRA: Marinellie Vega
Clinical Needs of Individuals with a Chromosome 15 Condition
Conditions: Angelman Syndrome
Principal Investigator: Paula Schleifer
CRA: Marinellie Vega
TS Alliance Tuberous Sclerosis Complex (TSC) Biosample Repository and Natural History Database
Conditions: Tuberous Sclerosis Complex
Principal Investigator: Paula Schleifer
CRA: Marinellie Vega
A Phase 3, Randomized, Double-Blind, Placebo-Controlled Study to Assess the Efficacy, Safety, and Tolerability of Valbenazine for the Treatment of Dyskinesia Due to Cerebral Palsy
Conditions: Cerebral Palsy
Principal Investigator: Migvis Monduy
CRA: Marinellie Vega
Learn more at https://clinicaltrials.gov/study/NCT05206513.
menu
menu-2
Brain
Ortho
Fundraise
Member Testimonials

 “I was blessed to be involved in the launch of the Nicklaus Children’s Hospital Family Advisory Council (FAC) in 1998. Our daughter Allyson had been born prematurely and she spent her first days of life in the NICU. A few months later, she was diagnosed with cerebral palsy and our family (my husband Nelson and son, Eric) were told she would not be able to walk, there was uncertainty about how long she would life and she might not even smile. Our family became committed to her development as well as to partnering with other families, hospital staff, the community, and the organization to support Nicklaus Children’s Hospital.
“I was blessed to be involved in the launch of the Nicklaus Children’s Hospital Family Advisory Council (FAC) in 1998. Our daughter Allyson had been born prematurely and she spent her first days of life in the NICU. A few months later, she was diagnosed with cerebral palsy and our family (my husband Nelson and son, Eric) were told she would not be able to walk, there was uncertainty about how long she would life and she might not even smile. Our family became committed to her development as well as to partnering with other families, hospital staff, the community, and the organization to support Nicklaus Children’s Hospital.
While those first few years were challenging with several visits every week for therapy, medical visits and surgery, she has thrived through it all and as you can see she does smile – a lot! Consequently, our family is deeply grateful for the excellent care she/we have received.
The work of the Family Advisory Council is to serve and support families, as well as to be a voice and advocate for those who come to the organization for care. Council members give back with their heart to assure that family needs are heard, and they provide encouragement and feedback to the organization as it cares for each and every child and their family.
Today, I am a member of the Council as a grandmother of two beautiful grandchildren, ages 3 and 1. We celebrate them along with their Aunt Allyson in supporting the excellent care that Nicklaus Children’s continues to provide. I am honored to continue to give my best in this capacity. I look forward to working with other committed families to continue to support the fundamental and essential work of Nicklaus Children’s Hospital and Health System, through the FAC.”
– Jackie Gonzalez
 “We spend a lot of time at Nicklaus Children's Hospital, both inpatient and outpatient, to work with numerous specialists. I chose to get involved with the Family Advisory Council for three main reasons. First and foremost, I want this hospital to be the best that it can be, so I'm excited to offer my insight. Second, I enjoy being able to participate in the development of new programs – it's empowering to be able to listen to staff from various departments make presentations and they greatly value our feedback. Last but not least, my family and I enjoy the camaraderie of the other families at the monthly meetings and special events. I encourage other families to join the FAC for these reasons, and many more!”
“We spend a lot of time at Nicklaus Children's Hospital, both inpatient and outpatient, to work with numerous specialists. I chose to get involved with the Family Advisory Council for three main reasons. First and foremost, I want this hospital to be the best that it can be, so I'm excited to offer my insight. Second, I enjoy being able to participate in the development of new programs – it's empowering to be able to listen to staff from various departments make presentations and they greatly value our feedback. Last but not least, my family and I enjoy the camaraderie of the other families at the monthly meetings and special events. I encourage other families to join the FAC for these reasons, and many more!”
– Andrea Abramowitz
 "My journey with Nicklaus Children's Hospital began in the most personal way possible — my daughter was diagnosed with an ultra-rare and mortal disease, making her the only known case in Miami. As a parent, this was a daunting revelation, but it was also the catalyst that drove me to become more involved in the healthcare community. Nicklaus Children's, being the sole freestanding children's hospital in Miami, became our second home, with my daughter seeing a myriad of specialists there.
"My journey with Nicklaus Children's Hospital began in the most personal way possible — my daughter was diagnosed with an ultra-rare and mortal disease, making her the only known case in Miami. As a parent, this was a daunting revelation, but it was also the catalyst that drove me to become more involved in the healthcare community. Nicklaus Children's, being the sole freestanding children's hospital in Miami, became our second home, with my daughter seeing a myriad of specialists there.
Joining the Family Advisory Council was a conscious decision driven by my desire to give back to the institution that has been pivotal in my daughter's care. My primary goal has always been clear: to aid Nicklaus Children's in its journey to become the premier children's hospital, ensuring that families like mine don't feel the need to seek care elsewhere. I believe that with the right guidance, dedication, and feedback, we can make Nicklaus Children's a beacon of hope and excellence for all families in Miami and beyond.
The Family Advisory Council, in my eyes, plays a monumental role in the broader healthcare landscape. It serves as the voice for those little souls who spend countless hours within the hospital walls, many of whom cannot articulate their needs, fears, or desires. We are their advocates, ensuring that their experiences are not just heard but acted upon. Our role is to bridge the gap between medical professionals and the families they serve, ensuring that every child's journey is as comfortable, compassionate, and effective as possible.
Your involvement with the Family Advisory Council will be more than just a membership; it's a commitment to bettering the lives of countless children. It's about ensuring that every child, irrespective of their medical challenges, receives the best care right here in Miami."
- Carolina Montoya
 "I serve on the Family Advisory Council because I wanted to make a difference in the lives of other families at Nicklaus Children's Hospital and make their experience a smooth one. My son was inpatient and as a mom I was frazzled. Anything I can do to alleviate even a little bit of that feeling for other parents, I want to do."
"I serve on the Family Advisory Council because I wanted to make a difference in the lives of other families at Nicklaus Children's Hospital and make their experience a smooth one. My son was inpatient and as a mom I was frazzled. Anything I can do to alleviate even a little bit of that feeling for other parents, I want to do."
-Michelle Appelrouth-Rader, MHC
 "We actively engage with the Family Advisory Council to contribute a distinct parental perspective on essential services for our children and collaborating on goal priorities."
"We actively engage with the Family Advisory Council to contribute a distinct parental perspective on essential services for our children and collaborating on goal priorities."
-Jorge and Leyma Menocal
Treatment Options
Treatment Options
Treatment Options
Diagnostic Imaging Tests
Diagnostic Imaging Tests
Diagnostic Imaging Tests
Meet the Neuro-Oncology Team
Meet the Neuro-Oncology Team
Meet the Neuro-Oncology Team
Games
Play AR Games
Enter the world of AR Games (Augmented Reality Games), where you can have a blast while you play with, care for, wash, feed, and pamper your favorite pet therapy dog! Each dog comes to life inside your daily world to keep you company.
Download AR Games
Play GameWorld
Explore the exciting collection of kids’ games including Spot the Difference, Four in a Row, and other popular puzzles, word searches, and challenging crosswords.
Enter GameWorld, where you can play to win, beat all the levels, find hidden objects, and learn new skills every time!
CASA Program Home
ConcoursClub
Service Award Recognitions
IRA
Home
At Nicklaus Children's Health System's Information Technology (IT) department work-life balance refers to the equilibrium between one's professional commitments and personal life, and ensuring that both aspects are adequately prioritized and nurtured. The work environment within the IT department provides numerous benefits for individuals who work for the company. The benefits help promote physical and mental well-being, reducing stress levels and preventing burnout. A balanced lifestyle at Nicklaus Children's Health System's Information Technology (IT) department enhances productivity and job satisfaction, it also helps individuals feel more motivated and engaged when they have time for activities outside of work.
Resources
At Nicklaus Children's Health System's Information Technology (IT) department work-life balance refers to the equilibrium between one's professional commitments and personal life, and ensuring that both aspects are adequately prioritized and nurtured. The work environment within the IT department provides numerous benefits for individuals who work for the company. The benefits help promote physical and mental well-being, reducing stress levels and preventing burnout. A balanced lifestyle at Nicklaus Children's Health System's Information Technology (IT) department enhances productivity and job satisfaction, it also helps individuals feel more motivated and engaged when they have time for activities outside of work.
Articles
At Nicklaus Children's Health System's Information Technology (IT) department work-life balance refers to the equilibrium between one's professional commitments and personal life, and ensuring that both aspects are adequately prioritized and nurtured. The work environment within the IT department provides numerous benefits for individuals who work for the company. The benefits help promote physical and mental well-being, reducing stress levels and preventing burnout. A balanced lifestyle at Nicklaus Children's Health System's Information Technology (IT) department enhances productivity and job satisfaction, it also helps individuals feel more motivated and engaged when they have time for activities outside of work.
Meet the Team
Program Leadership

Jenny Cordo, DNP, RN, NE-BC
Director of Professional Nursing Practice
Jenny Cordo is a board-certified nurse executive (NE-BC) with over 12 years of experience in nursing leadership, and 17 years overall with Nicklaus Children’s Hospital.
She completed bachelor’s degree in nursing from Boston College, master’s degree in nursing from Florida International University, and a doctorate degree (DNP) from the University of Miami in which she was recognized with the DNP Academic Excellence & Clinical Performance Award. Jenny has published various scholarly articles and has presented both podium and poster presentations across several professional organization conferences. She is a member of the American Nurses Association (ANA)/Florida Nurses Association (FNA), Florida Organization of Nurse Leaders (FONL)/South Florida Organization of Nurse Executives (SFONE), Sigma Theta Tau International (STTI), and the Nursing Consortium of Florida (NCOF). In addition, Jenny is the FONL Public Relations Committee Chair and sits on the FONL board as a representative of Nicklaus Children’s Hospital and the South Florida community of nursing leaders.
Flor Tena, MSN-Ed, RN, CBE, CCRN
Nurse Manager
Flor Tena is a nurse manager within the professional practice nursing team at Nicklaus Children’s Hospital. She completed a bachelor’s degree in nursing at Florida International University and a master’s degree in nursing education at Aspen University in Colorado. She has over 20 years of experience in neonatal nursing.
Her clinical interests are focused on supporting families with navigating healthcare systems. Mrs. Tena is passionate about implementing the latest evidence-based practices and quality improvement projects in the NICU, while collaborating with other areas in the institution where neonates receive care. Her work has been highlighted at poster and podium presentations at local and national conferences.
Mrs. Tena is a member of National Association of Neonatal Nurses (NANN) and American Association of Critical Care Nurses (AACN). She is bilingual in Spanish and English.
Patient Navigators
Patient Navigator Program (Home)
Pediatric Specialty Centers
Corp
Meet the Team
Infection Prevention and Control
Hand Hygiene
Hand hygiene plays a pivotal role in ensuring a healthy and safe travel experience. Traveling often involves being in crowded spaces and frequent contact with high-touch surfaces, making it crucial to prioritize hand hygiene. Utilizing hand sanitizer after touching surfaces like doorknobs, railings, or shared devices helps reduce the potential transmission of germs. Sanitizing hands before meals or touching one's face also serves as a strong protection against infection. Hand sanitizer is easy to pack and access, making it a great tool to promote hand hygiene while traveling.
Masking
When embarking on a journey during respiratory viral seasons (fall/winter), wearing a face mask is an essential practice, especially while in a crowded location. Packing a face mask before your trip is a proactive measure to lessen the risk of respiratory infections. Crowded environments, such as hospitals, heighten the potential for exposure to airborne pathogens. Wearing a face mask not only protects you but also contributes to community well-being by reducing the transmission of respiratory infections. This simple yet effective precautionary step becomes particularly important for individuals anticipating hospitalization, strengthening their defense against respiratory infections during the travel phase and ensuring a healthier transition into the medical setting.
Read about the hospital’s mask-wearing requirements
Safety Protocols for All Visitors
- All parents/guardians accompanying children must be free of signs and symptoms of infectious disease, including cough, runny nose, rash, vomiting, and fever. Please notify the medical provider caring for your child if you are anyone else in the home has a fever, cough, rash, shortness of breath, or any other sign of respiratory infection.
- Please remember to wash your hands or use alcohol-based hand sanitizer frequently during your visit.
Post-Care Infection Risk Management
Minimizing infection risk after a procedure or hospitalization is crucial for a smooth recovery. Following healthcare provider's guidelines for wound care, medication compliance, and hygiene practices is essential to their post-treatment health. It's important to maintain cleanliness, regularly wash hands, and avoid touching wounds without proper sanitation. If a patient suspects a post-op or post-hospital infection, immediately consult a healthcare professional. Timely reporting contributes significantly to the effective management and prevention of complications, ensuring a safe transition from hospital to home.
Blog
At Nicklaus Children's Health System's Information Technology (IT) department work-life balance refers to the equilibrium between one's professional commitments and personal life, and ensuring that both aspects are adequately prioritized and nurtured. The work environment within the IT department provides numerous benefits for individuals who work for the company. The benefits help promote physical and mental well-being, reducing stress levels and preventing burnout. A balanced lifestyle at Nicklaus Children's Health System's Information Technology (IT) department enhances productivity and job satisfaction, it also helps individuals feel more motivated and engaged when they have time for activities outside of work.
Meet the Team
Webinars & Lectures
Financial Transactions
The Nicklaus Children’s Hospital Global Health Department will assist you with your estimated financial responsibility for all scheduled visits prior to your arrival. To properly prepare for your visit, please be sure to provide your global health rep with any insurance information (if applicable).
Learn more about pricing transparency and estimates.
International patients have several payment options:
- Cash
- Visa
- MasterCard
- Discover
- American Express
- eChecking (ACH)
- Direct wire transfer (instructions provided upon request)
Please note complete payment is required prior to services being rendered.
Additionally, before leaving home please be sure to:
- Notify your bank and credit card companies in advance of any international transactions.
- Inquire about exchange rates that may impact your credit card charges and be aware of any foreign transaction fees you may incur.
Self-Parking and Valet Service
As you plan your visit to the hospital campus, we'd like to help you by providing suggested parking instructions. The hospital's My Nicklaus Children's app offers detailed instructions to our campus and detailed step by step directions once you have arrived and parked. We encourage you to download this app.
There are three separate garages on the hospital campus, each identified by a color, blue, green and yellow. Their use is entirely complimentary. Complimentary valet service is offered 24-hours a day in front of the Central Building, near the Devonshire Boulevard entrance to the campus. Additional complimentary valet services are available during select hours in the blue and yellow garages.

The Blue Garage is the first structure you will see upon entering via our 62 avenue entrance. This is a mixed occupancy garage, used by visitors and staff. Designated guest parking is offered on the first and second floors. While other floors may be used by staff, visitors may use all floors. Complimentary valet service will be offered on the ground floor of the Blue Garage, Monday through Friday from 7:00 a.m. – 9:00 p.m., for patients and visitors.
Please park in the Blue Garage if this is your planned destination:
Please park in the Green Garage, the first parking structure you will see upon entering from the SW 57 avenue (Red Road) and Devonshire Blvd. (SW 30 street) if this is your planned destination:
Yellow Garage
Complimentary valet services will be offered on the ground floor of the Yellow Garage, Monday through Friday from 6:00 a.m. – 6:00 p.m., for the Emergency Department and the Center for Spinal Disorders.
Self-Parking and Valet Service
As you plan your visit to the hospital campus, we'd like to help you by providing suggested parking instructions. The hospital's My Nicklaus Children's app offers detailed instructions to our campus and detailed step by step directions once you have arrived and parked. We encourage you to download this app.
There are three separate garages on the hospital campus, each identified by a color, blue, green and yellow. Their use is entirely complimentary. Complimentary valet service is offered 24-hours a day in front of the Central Building, near the Devonshire Boulevard entrance to the campus. Additional complimentary valet services are available during select hours in the blue and yellow garages.

The Blue Garage is the first structure you will see upon entering via our 62 avenue entrance. This is a mixed occupancy garage, used by visitors and staff. Designated guest parking is offered on the first and second floors. While other floors may be used by staff, visitors may use all floors. Complimentary valet service will be offered on the ground floor of the Blue Garage, Monday through Friday from 7:00 a.m. – 9:00 p.m., for patients and visitors.
Please park in the Blue Garage if this is your planned destination:
Please park in the Green Garage, the first parking structure you will see upon entering from the SW 57 avenue (Red Road) and Devonshire Blvd. (SW 30 street) if this is your planned destination:
Yellow Garage
Complimentary valet services will be offered on the ground floor of the Yellow Garage, Monday through Friday from 6:00 a.m. – 6:00 p.m., for the Emergency Department and the Center for Spinal Disorders.
Graduate Administrative Internship Home
Meet the Team
The Division of Pediatric Endocrinology team at Nicklaus Children's Hospital consists of board certified pediatric endocrinologists and a multi-specialty trained pediatric staff (certified diabetes nurse educator, registered dietitian, child life specialist, pharmacist, social worker and psychologist). Together they treat diabetes in children with a tailored program that fits the needs of the child and family and promotes the outcomes desired of the medical team.
The division is supported by a full-service on-site laboratory and outpatient center for your convenience.
Meet the Team
The Division of Pediatric Endocrinology team at Nicklaus Children's Hospital consists of board certified pediatric endocrinologists and a multi-specialty trained pediatric staff (certified diabetes nurse educator, registered dietitian, child life specialist, pharmacist, social worker and psychologist). Together they treat diabetes in children with a tailored program that fits the needs of the child and family and promotes the outcomes desired of the medical team.
The division is supported by a full-service on-site laboratory and outpatient center for your convenience.
Meet the Team
The Division of Pediatric Endocrinology team at Nicklaus Children's Hospital consists of board certified pediatric endocrinologists and a multi-specialty trained pediatric staff (certified diabetes nurse educator, registered dietitian, child life specialist, pharmacist, social worker and psychologist). Together they treat diabetes in children with a tailored program that fits the needs of the child and family and promotes the outcomes desired of the medical team.
The division is supported by a full-service on-site laboratory and outpatient center for your convenience.
Meet the Team
Ground Transportation
Nicklaus Children’s Hospital is not responsible for ground transportation services. We highly recommend that you budget transportation costs for your visit.
Florida law requires that children ages 0 through 3 years ride in an age-appropriate safety seat while traveling in a car. You can bring one from home to use during your trip or you can buy one while in Miami.
Driving or using a Rideshare App
It is recommended you use a smartphone map app (ex. Google Maps®, Waze®, etc.) for current traffic conditions.


Public Transportation
You can download local transit Apps such Moovit® or GO®.


Review-Dr-Contreras
Review-Katherine-Ponsoldt
Review-Dr-Agenia-Delouche
Review-Danielle-Quintana
Review-Dr-Forbess
Review-Dr-Lowisz
Review-Dr-Mejia-Otero
Review-Elisa-Echevarria
Review-Jacqueline-Verme
Review-Roberta-Zbar
Review-Isabela-Leon-Moll
Review-Danny-Luna
Review-Dr-Abigail-Ley
Review-Jacqueline-Bomhoff
Review-Karla-Novo
Review-Nike-Sitzman
Review-Andrea-Trevilla
Review-Christina-Valdes
Review-Damaris-Monzon-Aguirre
Review-Eli-Figueroa
Review-Magdalena-Garcia
Review-Elizabeth-Guerra
Review-Opal-Hamilton
Review-Vanessa-Manzie
Review-Sheryl-Stanley
Review-Carolina-Gonzalez
Review-Mia-Kalisch
Review-Anna-Pelligra
Review-Yessenia-Becraft
Review-Alejandra-Patterson
Review-Evelyn-Silva
Review-David-Figueroa
Review-Miguel-Lopez
Review-Patrice-Neil
Review-Eduardo-Romero
Review-Dr-Contreras
Review-Dr-Colon
Review-Dr-Colon
Review-Dr-Bismark-Gonzalez
Review-Dr-Vazquez
Review-Dr-Kleinberg
Review-Tania-Veloz
Review-Belinda-Godfrey
info
info-2
Metabolic Clinic Home
Diagnostics and Treatments
Carlin Prom Register 2024
Thank You
A member of our team will contact you shortly regarding your request.
grace-padron
Meet the Team
Summer Youth Internship Program
Nicklaus Children's Hospital collaborates with M-DCPS to facilitate summer internships to rising 10th through 12th Grade high school students between the ages of 15-18 enrolled in a Miami-Dade County Public School to gain experience and knowledge in their intended collegiate fields of study and/or careers.
Program Details
As required by M-DCPS, the Summer Youth internship program is a 5-week work-based learning experience between M-DCPS high school students and businesses and organizations throughout Miami-Dade County. It fosters a collaborative work/learn exchange between students and mentors, offering a comprehensive understanding of various aspects of the workplace.
Key Features of the Program Include:
- Minimum commitment of 30 hours per week for a duration of five weeks
- Opportunity for interns to earn academic credit, contingent upon a successful internship evaluation and completion of assigned academic tasks
- Interns are covered by the school accident policy throughout the program
- Oversight provided by both an instructional supervisor and a workplace supervisor
Mentors play a crucial role in the program, contributing their time and expertise to provide interns with meaningful, career-related experiences. They are responsible for submitting weekly timesheets and conducting quarterly grade evaluations to ensure the ongoing progress and development of the interns during the internship period.
How to Enroll
Students, all applications are facilitated through MDCPS directly.
A student must first complete the online pre-internship course and submit required completed documentation to the School Champion through miamiinterns.org.
Enroll
Parents and students can contact the Internship Hotline (305-693-3005) to find out more about enrollment and their School Champion.
For any other questions about this program please contact our Education Program/Internship Specialist by email at studentplacement@nicklaushealth.org

Programs
rx
recetas
cristina-abuchaibe
Food for Salud Home
Food for Salud Blogs
Miami Dade County Public Schools Telehealth Service
Telehealth Technology Supports Health Assessment at Your Child’s School

Have you ever been called away from work when your child’s school reports that your son or daughter is ill?
When health questions arise, the school-based nurses at your child’s school now have access to telehealth technology, made possible through Nicklaus Children’s Health System. The technology can be used to link your child and the school nurse to advanced care providers to assess certain conditions of the skin, ears, eyes, throat and lungs, while the child is still at school.
What is telehealth service and technology?
Telehealth technology can connect patients and caregivers at separate locations via a secure audiovisual connection to support health evaluation and assessment. School nurses at your child’s school can use his connection to consult with an advanced registered nurse practitioner (ARNP) or a medical doctor at Nicklaus Children’s Hospital. These experts will be able to use both visual and audio tools to assess your child’s medical condition through the remote connection. No video will be recorded during the consult to preserve student privacy.
What medical conditions can be assessed?
Conditions that can be assessed through the school’s telehealth connection include: fever, sore throat, earaches, cold symptoms and rashes.
How does this benefit me or my child?
An assessment may indicate that your child is well enough to stay in school. If the assessment identifies the source of the symptoms, it may be possible for you to pick up your child and go directly to the pharmacy of your choice to pick up a prescription to assist your child.
Does telehealth replace the school nurse or my primary care provider (PCP)?
No. Telehealth consults offer enhanced clinical services at school, including diagnosis and potential treatment of medical conditions. Your child’s PCP will be provided a summary of the visit. Follow up with the PCP within 48 to 72 hours is recommended.
Is there a fee for school-based telehealth services?
No. There will not be a charge for the service.
If you have questions about this service, please contact your school nurse as follows:
W.R. Thomas Middle School: 305-995-3993
Southwest Miami Sr High School: 305-274-0181
Airbase K-8 Center for International Education: 305-258-3676

West Coast University RN-MSN Scholarship

West Coast University is proud to offer one
100% Online RN-MSN full tuition scholarship.
100% Online Learning + CE Discounts + Student Support Services + Much More!
West Coast University is a nursing education partner of Nicklaus Children’s Hospital offering one RN to MSN online program scholarship to a Nicklaus Children’s Hospital employee. The two available track options are Nurse Leader or Nurse Educator. This RN to MSN online program is tailored for the working RN and is aimed at enhancing leadership and management skills. The program can be completed in as little as 24 months. Courses are delivered completely online with access to on-campus student services.
- Classes begin every 8 weeks
- Access to student services including Career Services
- Assistance securing practice experience
- Streamlined curriculum allows for up to 90 transfer credits
- Discounted CEs through Contemporary Forums
Deadline
Applications are due by April 15, 2024.
Eligibility Criteria
The scholarship criteria includes the following:
- Work in a clinical support role or within the nursing department, and be in good standing.
- Maintain employee benefit status, whether full-time or part-time status.
- Hold a current Florida nursing license.
Application Process
- Download and save the application in your files.
- Completely fill-in the application form (including essay and all required elements).
- Make digital copies of all the required documentation.
- Nursing License
- Unofficial transcripts
- Two letters of recommendation
- Submit your application and all files via email to Nursing.Scholarships@nicklaushealth.org.
Transfer Credits for RN to MSN Online Program
Nursing applicants requesting transfer credit evaluation must provide official transcripts no later than the first day of the first semester in which the student commences their education at West Coast University. College-level coursework will be considered and evaluated for transfer credit and all college-level coursework must have been taken at an institution accredited by an agency recognized by the U.S. Department of Education.
Virtual Care
Nicklaus Children's Hospital's Telehealth Center is a high-tech program designed to advance pediatric care for children around the world through enhanced access to pediatric subspecialty physicians and remote reading of diagnostic tests by highly trained experts.
For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org

Physician-to-Physician Videoconferencing
The center makes possible sophisticated videoconferencing, bringing together referring physicians from countries all over the world to consult with renowned subspecialty physicians based at Nicklaus Children's Hospital. Physician-to-physician consultative offerings include:

- Pediatric subspecialist consults
- Emergency care consults
- Complex multi-specialty team consultations
- Second opinions
Remote Reading of Diagnostic Tests
Nicklaus Children's Hospital also offers remote reading of diagnostic tests. The imaging teams at Nicklaus Children's Hospital, are among the region’s most experienced at reviewing and interpreting diagnostic tests.
Consultative Services with a Pediatric Leader
Nicklaus Children's Hospital, is one of the leading pediatric hospitals in the United States, with a 650-member medical staff that includes experts in virtually every pediatric subspecialty.
Consultations can be scheduled with individual subspecialists or a team of subspecialists as needed. Medical translation services are also provided when needed to support communications.
Offering Benefits for Overseas Patients and Partners
The Telehealth Center offers benefits to our overseas patients, physician colleagues and insurers.
- Participation in plan of care
- Educational opportunities
- Quality service offerings
- Efficient response time
Benefits to Overseas Patients
Physician-to-physician consultative services benefit patients in many ways. Families avoid the stress and expense of traveling, saving on airfare, local transportation and accommodations. They also avoid missing school and work days.
For More Information
The Nicklaus Children's Hospital Telehealth Center is a service of Global Health Services, which offers coordinated care and ease of access for international children and their families. For more information, please call Global Health at 305-662-8281 or email globalhealth@nicklaushealth.org
Roberto POM
About the Speakers
Podcast Home
Subscribe
Research & Reports
The Helen & Jacob Shaham Cancer and Blood Disorders Institute at Nicklaus Children's is engaged in more than 75 clinical cancer research studies, all of which are focused on finding new cures, treatments and diagnostic procedures for pediatric malignancies. No hospital in the region features such a wide array of clinical trials for childhood cancer research. As such, the Shaham Cancer & Blood Disorders Institute offers its patients unparalleled hope, offering the latest drug treatments, medical devices, biotechnology and other technological innovations in the fight against pediatric cancer.
The Children's Oncology Group (COG)
The Shaham Cancer & Blood Disorders Institute at Nicklaus Children's has been recognized as a full member of the prestigious Children’s Oncology Group (COG), a nationally funded group of pioneering physicians and institutions. To maintain this standing, full compliance with COG requirements is mandated. Compliance in this group involves not only participation in and adherence to multi-center research protocols, but also submission of accurate and timely data. The Institute has also been awarded a grant by the National Cancer Institute to advance childhood cancer research. In addition, members of the team share their knowledge through publication of clinical research study findings and presentations to national societies of physician scientists.
Laboratory Cancer Research
Significant progress has been made in the early development of new treatments and diagnosis through childhood cancer research in laboratories at Nicklaus Children's. Molecular and genetic diagnosis and classification of pediatric brain tumors is being developed by micro-array technology. This leading-edge approach is being used for diagnostic and prognostic evaluation of malignant solid tumors. Also underway is work focused on the roles of cell growth in the development of drug resistance in pediatric cancers. In an exciting new effort, Nicklaus Children's has made progress in evaluating alternative medicines that are used to treat cancer in other cultures.
Brain Cancer Research Program
Nicklaus Children's Hospital and Research Institute has initiated pediatric neuro/oncology research as a collaborative effort between the Divisions of Pathology, Hematology/Oncology, Blood and Marrow Transplantation and Neurological Surgery. Several investigators from these departments are involved in brain cancer research to improve the brain cancer treatment and disease free survival.
The major focus of the brain cancer research program is to understand the mechanisms behind the failure of chemotherapy and radiation therapy, and the reasons for the aggressiveness and invasiveness of brain tumors. The program is investigating the prognostic significance several genetic markers associated with cellular oncogenesis, drug resistance, cell proliferation, angiogenesis, differentiation and programmed cell death (apoptosis). The role of telomerase enzyme in the oncogenesis and aggressive behavior of certain brain tumors is also investigated in this research program. Alternative Medicine Projects include evaluation of the anticancer effects of curcumin and other "natural" compounds.
Through brain tumor research, our aim is to understand the origin, diagnosis, development and differentiation of brain tumor cells during the process of carcinogenesis. Simultaneously, we plan to translate the brain tumor research findings from evaluation of prognostic factors into the treatment of brain cancer patients.
Clinical trials including stem cell transplantation and anti-angiogenesis protocols are being used for patients with brain tumors. Young children are treated without radiation therapy to avoid late effects.
Active COG Trials
Click the tabs to expand.
Blood Trials
- AALL1631 – International Phase 3 Trial in Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia Ph+ ALL Testing Imatinib in Combination with Two Different Cytotoxic Chemotherapy Backbones.
- AALL1732 – A Phase 3 Randomized Trial of Inotuzumab Ozogamicin (IND#:133494, NSC#: 772518) for Newly Diagnosed High-Risk B-ALL; Risk-Adapted Post-Induction Therapy for High-Risk B-ALL, Mixed Phenotype Acute Leukemia, and Disseminated B-LLy.
- AAML1531 – Risk-stratified Therapy for Acute Myeloid Leukemia in Down Syndrome.
- AAML1831 – A phase 3 randomized trial for patients with de novo AML comparing standard therapy including gemtuzumab ozogamicin GO to CPX-351 with GO, and the addition of the FLT3 inhibitor gilteritinib for patients with FLT3 mutations.
- AAML18P1 – Stopping Tyrosine Kinase Inhibitors (TKI) to Assess Treatment-Free Remission (TFR) in Pediatric Chronic Myeloid Leukemia - Chronic Phase (CML-CP).
CNS Trials
- ACNS1422 – A Phase 2 Study of Reduced Therapy for Newly Diagnosed Average-Risk WNT-Driven Medulloblastoma Patients.
- ACNS1831 – A Phase 3 Randomized Study of Selumetinib (IND # 77782) versus Carboplatin/Vincristine in Newly Diagnosed or Previously Untreated Neurofibromatosis Type 1 (NF1) Associated Low-Grade Glioma (LGG)
- ACNS1833 – A Phase 3 Randomized Non-Inferiority Study of Carboplatin and Vincristine versus Selumetinib (NSC# 748727, IND# 77782) in Newly Diagnosed or Previously Untreated Low-Grade Glioma (LGG) not associated with BRAFV600E Mutations or Systemic Neurofibromatosis Type 1 (NF1)
Various Tumors Trials
- ADVL1521 – A Phase 2 Study of the MEK inhibitor Trametinib (IND#119346, NSC#763093) in Children with Relapsed or Refractory Juvenile Myelomonocytic Leukemia.
- ADVL1823 – Larotrectinib (LOXO-101, NSC# 788607, IND# 141824) for Previously Untreated TRK Fusion Pediatric Solid Tumors and TRK Fusion Relapsed Pediatric Acute Leukemias.
Germ Cell Trials
- AGCT1531 – A Phase 3 Study of Active Surveillance for Low Risk and a Randomized Trial of Carboplatin vs. Cisplatin for Standard Risk Pediatric and Adult Patients with Germ Cell Tumors.
- AGCT1532 – A Randomized Phase 3 Trial of Accelerated versus Standard BEP Chemotherapy for Patients with Intermediate and Poor-risk Metastatic Germ Cell Tumors.
- A031102 – A Randomized Phase III Trial Comparing Conventional-dose Chemotherapy using Paclitaxel, Ifosfamide, and Cisplatin (TIP) with High-dose Chemotherapy using Mobilizing Paclitaxel plus Ifosfamide followed by High-dose Carboplatin and Etoposide (TI-CE) as First Salvage Treatment in Relapsed or Refractory Germ Cell Tumors.
Hodgkin Lymphoma
- S1826 – A Phase III, Randomized Study of Nivolumab (Opdivo) Plus AVD or Brentuximab Vedotin (Adcetris) Plus AVD in Patients (Age >/= 12 Years) with Newly Diagnosed Advanced Stage Classical Hodgkin LymphomaHodgkin Lymphoma.
Hepatic Trials
- AHEP1531 – Pediatric Hepatic Malignancy International Therapeutic Trial (PHITT).
Neuroblastoma Trials
- ANBL00B1 – Neuroblastoma Classification Biology Studies.
- ANBL1232 – Utilizing Response- and Biology-Based Risk Factors to Guide Therapy in Patients with Non-High-Risk Neuroblastoma.
- ANBL1531 – A Phase 3 Study of 131I-Metaiodobenzylguanidine (131I-MIBG) or Crizotinib Added to Intensive Therapy for Children with Newly Diagnosed High-Risk Neuroblastoma (NBL) (IND# 134379) Arm C Temporarily Closed.
- ANBL1821 – A Phase 2 Randomized Study of Irinotecan/Temozolomide/Dinutuximab with or without Eflornithine (DFMO) (IND# 141913) in Children with Relapsed, Refractory or Progressive Neuroblastoma.
Registry and Biology
- APEC14B1 – Project: EveryChild A Registry, Eligibility Screening, Biology and Outcome Study.
MATCH Trials
- APEC1621A – Phase 2 subprotocol of LOXO-101 (larotrectinib) in patients with tumors harboring actionable NTRK fusions.
- APEC1621B – Phase 2 subprotocol of JNJ-42756493 (Erdafitinib) in patients with tumors harboring FGFR1/2/3/4 alterations.
- APEC1621D – Phase 2 subprotocol of LY3023414 in Solid Tumors.
- APEC1621F – Phase 2 subprotocol of Ensartinib in patients with tumors harboring ALK or ROS1 genomic alterations.
- APEC1621G – Phase 2 subprotocol of Vemurafenib in patients with tumors harboring actionable BRAF V600 mutations.
- APEC1621H – Phase 2 subprotocol of olaparib in patients with tumors harboring defects in DNA damage repair genes.
- APEC1621I – Phase 2 subprotocol of Palbociclib in Patients with Tumors Harboring Activating Alterations in Cell Cycle Genes.
- APEC1621K – Phase 2 Subprotocol of AG-120 (Ivosidenib) in Patients with Tumors Harboring IDH1 Mutations.
- APEC1621M – Phase 2 subprotocol of Tipifarnib in patients with tumors harboring HRAS genomic alterations.
- APEC1621N – Phase 2 Subprotocol of LOXO-292 in Patients with Tumors Harboring RET Gene Alterations.
- APEC1621SC – NCI-COG Pediatric MATCH (Molecular Analysis for Therapy Choice) Screening Protocol
Renal Trials
- AREN03B2 – Renal Tumors Classification, Biology, and Banking Study.
- AREN1721 – A Randomized Phase 2 Trial of Axitinib/Nivolumab combination therapy vs single agent Nivolumab for the treatment of TFE/Translocation Renal Cell Carcinoma across all age groups.
Rhabdo-Sarcomas Trials
- ARST1431 – A Randomized Phase 3 Study of Vincristine, Dactinomycin, Cyclophosphamide (VAC) Alternating with Vincristine and Irinotecan (VI) Versus VAC/VI Plus Temsirolimus (TORI, Torisel, NSC# 683864) in Patients with Intermediate Risk (IR) Rhabdomyosarcoma (RMS).
Miscellaneous Trials
- ALTE07C1 – Neuropsychological, Social, Emotional and Behavioral Outcomes in Children with Cancer.
Active Non-COG Trials
Click the tabs to expand.
Leukemia/Hematology Trials
- Novartis CPKC412A2218 [Dr. De Angulo] – Phase II, Open-Label, Single Arm Study To Evaluate The Safety, Efficacy, And Pharmacokinetics Of Twice Daily Midostaurin (PKC412) Combined With Standard Chemotherapy And As A Single Agent Post-Consolidation Therapy In Children With Untreated FLT3-Mutated AML.
Transplant Trials
- PBMTC_ONC1701 - EndRad [Dr. Galvez] – A Phase II Pilot Trial To Estimate Survival After A Non-Total Body Irradiation (TBI) Based Conditioning Regimen In Patients Diagnosed With B-Acute Lymphoblastic Leukemia (ALL) Who Are Pre-Allogeneic Hematopoietic Cell Transplantation (HCT) Next-Generation-Sequence (NGS) Minimal Residual Disease (MRD) Negative.
- CIBMTR 2500 [Dr. Galvez] – Protocol for a research database for hematopoietic cell transplantation, other cellular therapies and marrow toxic injuries.
- CIBMTR 2501 [Dr. Galvez] – Protocol for a research sample repository for hematopoietic cell transplantation, other cellular therapies and marrow toxic injuries.
- 10 CBA [Dr. Galvez] – A Multicenter Access And Distribution Protocol For unlicensed Cryopreserved Cord Blood Units (Cbus) For Transplantation In Pediatric And Adult Patients With Hematologic Malignancies And Other Indications.
- 1507 [Dr. Galvez] – Reduced Intensity Conditioning for Haploidentical Bone Marrow Transplantation in Patients with Symptomatic Sickle Cell Disease.
- WASHU 01-0923 [Dr. Galvez] – A Study Of Hematopoietic Stem Cell Transplantation (HSCT) In Pediatric Nonmalignant Disease Using A Reduced-Intensity Preparatory Regime.
- PBMTC SUP1801 17-SIBS (Donor Kids) [Dr. Galvez] – Identifying Predictors of Poor Health-Related Quality-of-Life among Pediatric Hematopoietic Stem Cell Donors.
- Astellas 9766-CL-0107 [Dr. Galvez] – A Phase 2, Open-Label, Non-Comparative, Multicenter Study To Evaluate the Safety and Tolerability, Efficacy and Pharmacokinetics of Isavuconazonium Sulfate for the Treatment of Invasive Aspergillosis (IA) or Invasive Mucormycosis (IM) in Pediatric Subjects.
CNS Trials
- Head Start 4 [Dr. Khatib] – Newly Diagnosed Children (Less Than 10 Years Old) With Medulloblastoma And Other Central Nervous System Embryonal Tumor.
Various Tumor Trials
- Ex-Vivo Drug Screen [Dr. Salyakina] – Personalized Ex Vivo Drug Screening and Genomic Profiling to Guide Individualized Treatments for Children with Relapsed or Refractory Solid Tumors and Leukemias.
- CHLA Onco-Kids [Dr. Fader] – Next-Generation Sequencing of Pediatric Tumor Samples (OncoKids®) from a Multi-Institutional Consortium of Clinical Cancer Programs
Neuroblastoma Trials
- NMTRC012 [Dr. De Angulo] – A Study Using Molecular Guided Therapy with Induction Chemotherapy followed by a Randomized Controlled Trial of standard immunotherapy with or without DFMO followed by DFMO maintenance for Subjects with Newly Diagnosed High-Risk Neuroblastoma.
Miscellaneous Trials
- Nourish-T+ [Dr. Abdella] – A Randomized Control Trial Targeting Parents in Promoting Healthy Eating and Exercise Behaviors in Pediatric Cancer Survivors with Overweight/Obesity.
- Pfizer B0661037 [Dr. Fader] – A Randomized, Open-Label, Active Controlled, Safety And Descriptive Efficacy Study In Pediatric Subjects Requiring Anticoagulation For The Treatment Of A Venous Thromboembolic Event.
Sarcomas Trials
- BIO-11006 [Dr. De Angulo] – A Phase 2 Study of the Safety and Efficacy of BIO-11006 in the Treatment of Recurrent Osteosarcoma and Ewing’s Sarcoma in Patients with Lung Metastases.
- Ex-Vivo Observation [Dr. Fader] – Drug Sensitivity Testing and Mutation Profiling in Childhood Sarcomas.
Reports
Published reports are in compliance with the ACoS, CoC and are standard specific.
Thank You
Thank you for submitting your registration!
Widget (hidden)
Observer Program Payment
Click the button to pay.
You will be re-directed to Authorize.net to complete the credit card payment.
LifeFlight Survey Referral Hospital
LifeFlight® Referral Hospital Survey
Symptom Checker
Symptom Checker
Disclaimer
This Symptom Checker allows you to choose a variety of factors, to help guide consideration of some potential medical conditions related to your symptom. This tool does not incorporate all the personal, health and demographic factors related to you, individually, that would allow a diagnosis or treatment to be suggested.
The best way to determine the cause of your symptom, and what to do, is to visit your healthcare provider. Always seek the advice of your physician or other qualified healthcare provider before starting any new treatment or discontinuing an existing treatment. Talk with your healthcare provider about any questions you may have regarding a symptom or medical condition. Nothing in these pages may be used for medical diagnosis or treatment.
Not a Substitute: The information and materials in these pages are not a substitute for the personalized care and knowledge that your physician can provide to you. It is not intended nor implied to be a substitute for professional medical advice. It is not a diagnostic tool, and is provided for educational purposes only. You assume full responsibility for how you choose to use this information.
Supplement: The information and materials presented here in this website are meant to supplement information that you obtain from your physician. Any discrepancy between the information presented in this website and any statement by your physician should be resolved in favor of your physician. He or she has the benefit of knowing your individual medical situation.
Limitations: You should recognize that the information and materials presented in this website have the following limitations, in comparison to being examined by your own physician:
- You can have a conversation with your doctor.
- Your doctor can perform a physical examination and any necessary tests.
- You could have an underlying medical problem that requires a physician to detect.
- If you're taking medications, they could influence how you experience various symptoms.
If you think that you are having a medical emergency, call 911 or whatever the number is for the local emergency ambulance service right away. When in doubt, call your doctor or go to the closest emergency department.
By using this website, you accept the information provided herein “AS IS." Neither Nicklaus Children's, nor the providers of the information contained in this website, will have any liability to you arising out of your use of the information contained in this website, nor make any express or implied warranty regarding the accuracy, content, completeness, reliability, or efficacy of the information contained within this website.
savannah-moon
Giving Docs
Create a Will
stacie-peddy
ask-nick
Cardio-Oncology Clinic Home
Cardio-Oncology Clinic Home
Cardio-Oncology Clinic Home
Cardio-Oncology Clinic Home
Resources for Scoliosis Patients
News
NCH-Housestaff-Institutional-Manual-2021.pdf
nicole-redondo
Treatments and Procedures
sarah-jernigan
Empower Personal Cash Savings
Review-Dr-Stabingas
CPR Classes Payment
Friends and Family CPR
$20
Click the button to pay with credit card.
Heartaver CPR
$45
Click the button to pay with credit card.
BLS (Basic Life Support) CPR
$45
Click the button to pay with credit card.
PALS (Pediatric Advanced Life Support)
$85
Click the button to pay with credit card.
NRP (Newborn Resucitation Program)
$85
Click the button to pay with credit card.
Trevor-Resnick
Sayed-Naqvi
mark-epstein
Fellowship Home
Thelma-Sugranes
In-Person Palm Beach Cardiology Lecture and Dinner

In-Person Palm Beach Cardiology Lecture and Dinner
Thursday, September 12, 2024
6 p.m: Registration
6:30 p.m. - 8:30 p.m.: Lecture and Q & A
Location:
Seasons 52
11611 Ellison Wilson Rd
Palm Beach Gardens, FL 33408
Topics:
Preventive cardiology and syncope
Chest pain and murmur
Free ECG Screening
Speakers:
Joanna Lowisz, DO
Medical Director, Preventive Cardiology Program
Pediatric and Fetal Cardiologist
Nicklaus Children's Hospital
Cristina Abuchaibe, DO
Fetal and Pediatric Cardiologist
Nicklaus Children's Hospital
Himanshu Adlakha, MD
Fetal and Pediatric Cardiologist
Nicklaus Children's Hospital
Emergency Rooms
Partner Units
Counties
As part of our commitment to be where the children are, we bring world-class specialty care to you because your child matters most. Our locations across South Florida offer appointments with board-certified physicians, diagnostics and imaging services, rehabilitation and walk-in urgent care. Please click the links below to see the services offered at each location.
Miami-Dade County
As part of our commitment to be where the children are, we bring world-class specialty care to you because your child matters most. In Miami-Dade county, we offer appointments with board-certified physicians, diagnostics and imaging services, rehabilitation and walk-in urgent care (services vary by location).
Please click the links below to see the services offered at each location.
Palm Beach & Martin Counties
As part of our commitment to be where the children are, we bring world-class specialty care to you because your child matters most. In Palm Beach & Martin counties, we offer appointments with board-certified physicians, as well as advanced medical and therapeutic services through our collaboration with Jupiter Medical Center.
Please click the links below to see the services offered at each location.
Child Neurology Residency Program
Psychology Programs Home
Collier County
Nicklaus Children's is collaborating with NCH Healthcare System to provide pediatric medical services at NCH North Naples Hospital with the aim of supporting families in Collier County in receiving top-quality pediatric inpatient care close to home.
Clinicians employed by Nicklaus Children's Pediatric Specialists (NCPS), the physician-led medical group practice of Nicklaus Children's Health System, are staffing inpatient services for the NCH neonatal intensive care unit, pediatric intensive care unit and other pediatric inpatients as well as newborn routine screenings.
Broward County
As part of our commitment to be where the children are, we bring world-class specialty care to you because your child matters most. In Broward county, we offer appointments with board-certified physicians, diagnostics and imaging services, rehabilitation and walk-in urgent care (services vary by location).
Please click the links below to see the services offered at each location.
Luciana POM
thomas-utset-ward
Meet the Team
The team provides medical care using evidence-based tools, a proficient level of training and education, clinical research and state-of-the-art medical technology. The goal is to provide excellent care and to ensure that each infant achieves his or her full potential.
Intestinal Ultrasound Program Home
Pulmonary Vein Stenosis Program Home
Review-Nicklaus-Childrens-Hospital
julia-zubillaga
jennifer-thompson
andrea-alonzo
Kenneth C. Griffin Surgical Tower Social Media Toolkit
Kenneth C. Griffin Surgical Tower Social Media Toolkit
We are excited to announce the opening of the Kenneth C. Griffin Surgical Tower at Nicklaus Children's Hospital!
This state-of-the-art facility is designed to enhance patient care and support the incredible work our medical teams do every day. Featuring advanced technology and innovative spaces, the new tower marks a major milestone in our commitment to delivering the highest standard of care to children and families.
We encourage all employees to share the news on their social media platforms and help spread the word about this exciting new chapter in the future of pediatric healthcare!
Facebook, Instagram, and LinkedIn In-feed Post
Right click the image, or long press to save.
Caption
We’re thrilled to announce the grand opening of the Kenneth C. Griffin Surgical Tower at Nicklaus Children’s Hospital! 🎉 This state-of-the-art, five-story tower is a monumental step toward our commitment to providing world-class pediatric care. Spanning 131,000 square feet, the new tower features advanced surgical suites and spacious recovery areas designed for our patients and their families. Thanks to a generous $25 million donation from Kenneth C. Griffin, this tower represents the future of pediatric surgery. The new space will allow us to offer life-saving care with the latest medical technology and equipment. We’re excited to continue serving our community and look forward to making a bigger impact in children’s health. #nicklaus4kids #nicklauschildrenshospital #Pediatrics
Post on Facebook – Tag us at: @Nicklaus Children’s Hospital
Post on LinkedIn – Tag us at: @Nicklaus Children’s Health System
On Instagram – Tag us at: @nicklaus4kids and add our location: Nicklaus Children’s Hospital
How to Post an Instagram In-feed Post
- Open Instagram and tap the "+" icon at the bottom to start a new post.
- Choose a photo or video of the Kenneth C. Griffin Surgical Tower provided in this toolkit. After selecting, click "Next."
- Write a caption by using the approved caption provided above.
- Tag Nicklaus Children's Hospital by typing @nicklauschildrens in the caption.
- Click "Share" to post!
How to Post a Facebook In-feed Post
- Open Facebook and tap “What’s on your mind?” to start a new post.
- Write a post announcing the opening of the Kenneth C. Griffin Surgical Tower using the approved caption above.
- Add a photo or video by clicking the “Photo/Video” button and selecting one of the images provided on slide 3 of this toolkit.
- Tag Nicklaus Children’s Hospital by typing “@NicklausChildrens” in your post.
- Click “Post” to share with your friends!
How to Post a LinkedIn In-feed Post:
-
Go to LinkedIn and click “Start a post” at the top of your feed.
-
Write a professional post announcing the grand opening of the Kenneth C. Griffin Surgical Tower using the approved caption above.
-
Attach a photo by clicking the “Photo” icon and selecting an image provided on slide 3 of this toolkit.
-
Add hashtags like #nicklaus4kids and #pediatrics. Tag Nicklaus Children’s in the post by typing @Nicklaus Children's Health System.
-
Click “Post” to share with your professional connections!
Facebook & Instagram Stories
Right click the image, or long press to save.
On Instagram – Tag us at: @nicklaus4kids
On Facebook – Tag us at: @Nicklaus Children’s Hospital
How to Post an Instagram Story
- Open Instagram and swipe right on your home screen to access the Stories camera.
- Tap the square icon at the bottom left to upload a provided image from this slide.
- Tag Nicklaus Children’s Hospital by typing @nicklauschildrens in the text.
- Tap "Your Story" at the bottom to share it with your followers!
How to Post a Facebook Story
- Open Facebook and tap “Create a Story” at the top of your news feed.
- Select a photo or video by uploading a provided image from this slide.
- Tag Nicklaus Children’s Hospital by typing @Nicklaus Children’s Hospital in the text field.
- Tap "Share to Story" to post it!
X (Formerly Twitter) In-feed Post
Right click the image, or long press to save.
Caption
We’re thrilled to announce the grand opening of the Kenneth C. Griffin Surgical Tower at Nicklaus Children’s! This state-of-the-art facility marks a major step toward world-class pediatric care, featuring advanced surgical suites and spacious recovery areas. #nicklaus4kids
Post on X– Tag us at: @nicklaus4kids
How to Post on X
- Open Twitter and tap the "+" icon to create a new tweet.
- Write a tweet announcing the grand opening of the Kenneth C. Griffin Surgical Tower using the approved caption provided on this slide.
- Add a photo by tapping the camera icon and selecting an approved image provided on this slide.
- Include hashtags like #nicklaus4kids and tag Nicklaus Children’s Hospital by typing @Nicklaus4kids.
- Tap “Tweet” to share with your followers!
mikhaylo-szczupak
joaquin-jimenez
CPI Course Payment
$85
Click the button to pay.
You will be re-directed to Authorize.net to complete the credit card payment.
Ortho-Oncology Program Home
Ortho-Oncology Program Home
Treatments and Procedures
Treatments and Procedures
Conditions we Treat
Conditions we Treat
Menu-espanol
Menu-creole
DBStaffFlashSale
Dan Marino Outpatient Center Home
Articles
Home
Neurosurgery Update for Pediatric Providers

Neurosurgery Update for Pediatric Providers
Tuesday, November 12, 2024
6:00p.m. - 9:00p.m. -- Dinner Lecture and Q & A
Location:
Caffe Vialetto - Coral Gables
4019 Le Jeune Road
Coral Gables, FL 33134
Speakers & Topics
Dr. John Ragheb, MD
Department of Surgery and Director of the Division of Neurosurgery
Topic :
Advances in Neuromodulation and Epilepsy Surgery in Children
Dr. Sarah Jernigan, MD
Medical Director of Quality, Nicklaus Children’s Hospital, Brain Institute
Neurosurgery Surgical Director, Spasticity and Movement Disorders
Topic:
Spasticity
Dr. Kristen Stabingas, MD
Pediatric Neurosurgeon
Topic:
Brachial Plexus
Thank You
Meet the Team
Meet the Team
SilentAuction24
Jameson
Wishlist
Our City
Where We Work
stephanie-mangles
CoachSpos5k
Wyatt-POM
Review-Dr-Ehret
magic
Review-Galloway
Patient Stories
Patient Stories
Review-Dr-Mangels
News
License
Contact Us
About Us
Review-Dr-Padron
Review-Dr-Abuchaibe
Review-Dr-Moon
Review-Dr-Redondo
Review-Dr-Sugranes
Review-Dr-Thompson
Review-Dr-Szczupak
Review-Dr-Zubillaga
Review-Dr-Jimenez
Review-Dr-Utset-Ward
Review-Dr-Jernigan
Review-Dr-Gandhi
Review-Dr-Jan
CraneTwins
Patient Stories
Patient Stories
donna-k-rhoden
Discount
Click on the button to pay with credit card.
The link will open Authorize.net to complete the transaction.
Discounted Registration
$637.50
© 2025 Nicklaus Children's Hospital. All Rights Reserved.